Items
topic_interest is exactly
healthcare
-
 2020-12
2020-12The impact of COVID on the LGBTQ+ Community
This PDF details data related to the LGBTQ+ Community's relationship with COVID in America. Based on the data, it is clear many within the community struggled with excessive financial issues, the inability to receive medical care, and the loss of insurance. While the pandemic has placed serious burdens as a whole on society, data such as this is valuable as it allows a look into the most vulnerable communities within society already, and how COVID has destroyed the once normal lives of so many. -
 2022-05-27
2022-05-27Moving away from the pandemic in Arkansas
This article details a sharp decline in the number of Arkansans on ventilators due to COVID-19. It further provides information on a new oral drug to combat the pandemic in Arkansas. While cases in Arkansas regularly fluctuate, it is encouraging to see individuals off ventilators which removes some of the strain most Arkansas hospitals have been experiencing over the last two years. A rise in vaccinations and a greater understanding of the disease allows for a return to normalcy that many states are now experiencing. Additionally, and oral drug to combat COVID-19 is helpful and will allow the disease to be easily managed. -
 2022-05-12
2022-05-12Covid-19 narrows long-standing Latino mortality advantage, study finds
This is a news story from NBC News by Nicole Acevedo. Latinos have been shown to have lower mortality rates compared to non-Hispanic whites, where they live an average of three extra years. This changed with the virus. In a study published by the Lerner Center for Public Health Promotion, COVID-19 has been shown to kill Latinos 65 or older at 2.1 times the rate of whites in 2020. This number decreased slightly in 2021, which was at 1.6 times the rate of whites. So far this year, it has been at 1.2 times the rate of death. In total, COVID has killed 124,000 Latinos since the start of the pandemic in the United States, which accounts for 17% of deaths. The reason the Latino death rate is high is debated, but some say it is because Latinos in the United States are less likely to have access to quality healthcare or have jobs that would expose them to the virus more often. -
 2020-03-15
2020-03-15Together and Apart
Flagstaff AZ. My husband was an occupational therapist who regularly worked in the ICU at Flagstaff Medical Center. I remember the week after the lockdown started (March 15th or so) the Covid-19 numbers were doubling every week at FMC. My husband started changing out of his scrubs and shoes in the garage. I was a speech therapist with the school district and we were all asked to stay home, which was good because I have two school-aged children. As the Covid numbers started to skyrocket in our region due to a devastating outbreak on the Navajo nation, my husband became more and more worried about bringing the virus home since there was a shortage of PPE. When it was announced that my own job would go remote and I would need to start scheduling teletherapy sessions with my students, we decided it would be better for me and the kids to go live with my mom and dad in Tempe for a few weeks. My mom is a retired teacher and offered to teach my kids while I worked with my students online. The kids loved having grandma be their teacher. I had to learn how to work with preschoolers with disabilities over Zoom, which is no easy task! Meanwhile, my husband was providing us updates; when he finally got fitted for a tyvek suit was a happy day because he could spend all day in it helping patients. The doctors were trying new therapies with patients every week, but mostly he saw many people seem to get better and then take unexpected deadly turns. Treating isolated, scared patients while feeling helpless to know what to do was taking a toll on everyone at the hospital. The kids and I spent 7 weeks with my mom, face-timing him every night. Finally, as the school-year came to a close, we were able to reunite. I captured the moment we got home and my husband hugged my 5 year old son. We were so lucky; no one in the family had gotten sick so far despite my husband being in close proximity to patients each day. Over the summer and into the next school year we were hoping for some normalcy to return but it was nothing but adapting to change. The kids made friends with the neighbors down the street not by playing in the front yard, but by yelling greetings over the fence. When they started school in the fall we organized a "pod" with other families whose children were in the same classes as ours at DeMiguel elementary. We had four kindergarteners and three 2nd graders all doing school over Zoom at the same time, which was not easy for the parents who had to oversee them (my husband had the honor at least once a week), but the kids really benefitted from having friends to play with during breaks. We saw them become more motivated to participate and happier overall. I started seeing some students in-person for the first time at the school on a very limited basis. I wore clear PPE products so my students could see my mouth. The kids didn't go back to in-person school until about a year after the lockdown (Spring 2021). As the school year ended, the wildest school year of our lives, things did start to seem normal again, but we ended up leaving Flagstaff for Tucson due to soaring high home prices and my husband needing a fresh start away from the memories of the early pandemic. -
 2021-04-22
2021-04-22Hospice and hospitals during a pandemic
This is a photo of my grandfather's glasses and a blanket given to him by one of the hospice nurses. He passed in April of 2021, not due to Covid. There were still a lot of Covid restrictions put in place by the hospital, and the hospice center. Everyone had to be checked in at the front desk, temps were taken, questionnaires filled out, and the number of guests at a time was limited. He was moved to a hospice facility down the road from the hospital that he had been in. I was spending 10-12 hours a day with him at this time. He passed very late in the night and the next morning I went to pick up his remaining items. Most I gave to my dad, but I kept the blanket and his glasses. This, I believe, shows a broader picture of the pandemic in relation to healthcare during this time. Everyday healthcare still was taking place, it couldn’t just stop, but they had to adapt. I’ve heard stories from social media and directly from healthcare workers about being exhausted due to the pandemic and Covid guidelines. All I can say is that even after being tired and working through horrible conditions for over a year, every person I talked to for the week that he was there was kind and caring. Healthcare for the last two years has focused a lot of Covid healthcare, which makes sense, but this, in my mind at least, serves as a reminder of the continuous healthcare that has always been happening. I am so grateful for the team of professionals that helped and cared for him that last week. -
 2022-04-18
2022-04-18Natural Medicine
This is an Instagram post by angelicaviator. This person suggests that more natural cures can help with COVID symptoms. Since natural cures don't make profit for the healthcare industry, this is why this person thinks that they are often overlooked. The picture that goes with this has types of juicing suggestions on what goes best against a certain ailment. -
 2022-04-19
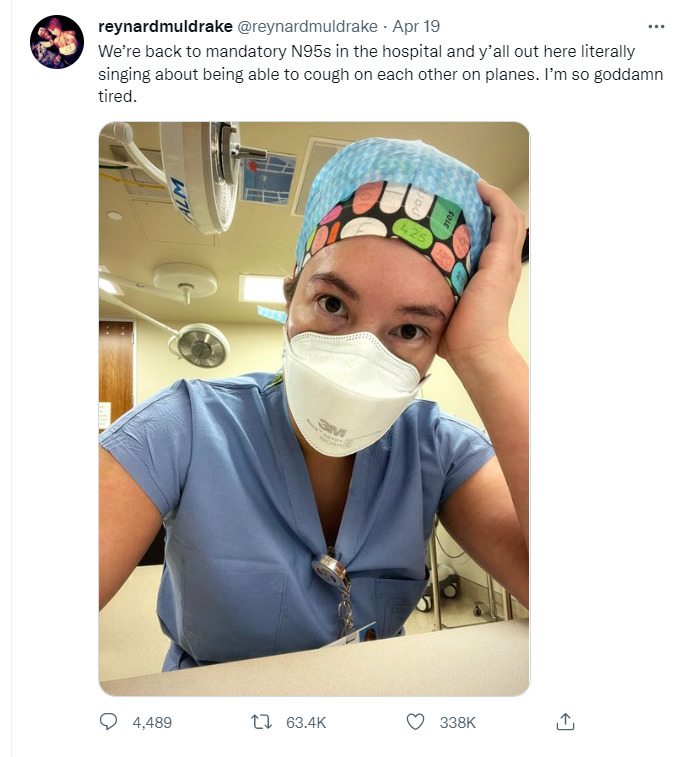
2022-04-19Twitter post in response to masks no longer being federally required on planes
A Twitter user, who works in a hospital, shares her frustrations after masks are no longer federally required on planes. Many people are happy about this ruling, but others, especially those on the "frontlines" in the hospitals, are expressing their frustrations with people acting as if the pandemic is over. -
 2022-04-12
2022-04-12Even the Pandemic Didn't Stop STDs From Spreading in the U.S.
This is a news story from Bloomberg by Madison Muller and Ella Ceron. According to recent reports, the overall amount of STDs went down with the lockdowns in early 2020, but then started to rise again near the end of 2020. Gonorrhea, syphilis and congenital syphilis all surged later in the year to exceed 2019 totals, the Centers for Disease Control and Prevention said in the report. Chlamydia remained the most common STD for the year, although cases declined overall, likely because of under-diagnosis. Possible reason why the numbers may be decreased for the beginning of 2020 might not be because of the lockdowns entirely. Some people in 2020 skipped doctor's appointments where they could have gotten diagnosed, in addition to resources being low during the height of the pandemic. Other trends included in this study are the rates of health insurance among certain demographics. Black people, in addition to LGBTQ people, are shown to have lower rates of having health insurance. -
 2022-04-11
2022-04-11It's Not Over Yet
This is a Twitter update from DrLindaMD. This is about a doctor rebutting claims that COVID is over now. She says that she has had five patients in the last week who thought they just had a cold, but it turned out that they had COVID. None of those patients chose to isolate because "it was just a cold." -
 2022-01-09
2022-01-09Dear Unvaxxed Friends: I Don't Want To Judge You, I Just Don't Want You To Die
This is a text story by YourTango, written by Joanna Schroeder. This is a story written from the point-of-view by someone that wants others to be vaccinated. At the beginning, she brings up the feelings of distrust some have towards the government, which has been a big reason why some are refusing to get vaccinated. The author then mentions that she has been seeing an increase in patients with heart problems in the pediatric section of hospitals, with some of those cases being due to COVID. Continuing on with this point, the author mentions a peds cardiologist she has been in contact with, and the cardiologist says that there has been an increase in myocarditis cases due to COVID. Later, she says that her left-leaning friends are receptive to data like this, but her right-leaning friends are not. She then pleads that she does not want her unvaccinated friends to die, and that they have a greater chance of getting hospitalized compared to those that are vaccinated. Finally, she ends by saying to not let policies get in the way of good judgement, saying that she is tired of misinformation coming from both sides. -
 2022-04-11
2022-04-11COVID-19 Testing
This is an Instagram post by medrite_springfieldnj. This is a PSA welcoming people to get free COVID testing. It says that no appointments necessary and walk-ins are welcome. Since the start of the pandemic, rapid testing and PCR tests have become more available and free of charge in many places. The reason many of these are free is due to state and federal governments subsidizing the costs of the tests, in addition to people volunteering to help them get done. -
 2022-04-11
2022-04-11Medicare Y COVID-19
This is an Instagram post by crespoinsurance. This is a post written in Spanish giving advice to elderly on vaccines. It advises people fifty and older, and those that are immunocompromised to get vaccinated. It also says that Medicare covers COVID vaccines. -
 2022-04-07
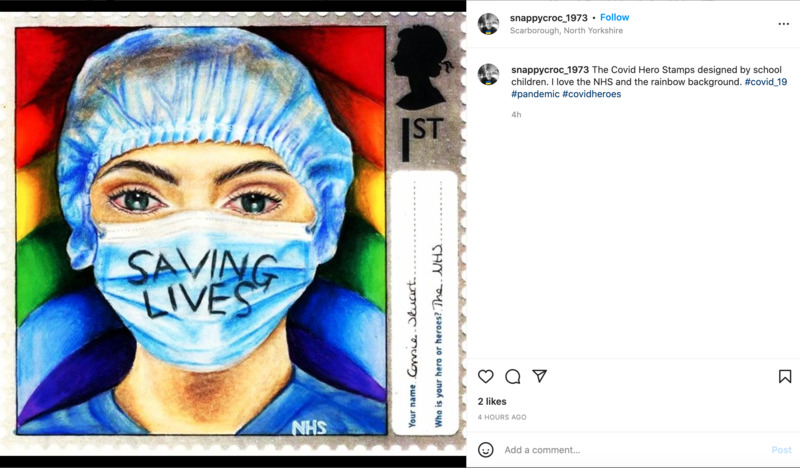
2022-04-07COVID Heroes
This is an Instagram post by snappycroc_1973. This user posted a picture of one of the COVID Hero Stamps designed by school children. These stamps are meant to support the NHS (National Health Service), which is based in the United Kingdom. -
 2022-04-07
2022-04-07Where the Government Requires Masks
This is an Instagram post by urbanpeaceinstitute. This post refers to places where mask mandates are still in existence. Even though mask mandates have been lifting in many places, certain places still want masks. Some of these places include: emergency and homeless shelters; public transit; healthcare settings; long-term care facilities; and correctional and detention facilities. These places are either government or healthcare associated. This post links to the County of Los Angeles Public Health for more information on the Coronavirus. -
 2022-04-07
2022-04-07Ways of Prevention
This is an infographic on Instagram posted by fairhavenhealthcare. This infographic advises people to: use tissues when sneezing or coughing; wash hands often; refrain from crowded places; not to touch hands, mouth, or eyes; follow recommendations from healthcare providers; and get vaccinated. -
 2022-04-07
2022-04-07Get Vaccinated
This is an Instagram post from myinnovage. This is a team that worked on getting people vaccinated. Here, one of the pictures that was chosen was of a woman holding a blank vaccine card and wearing a mask. This team is in Colorado and is encouraging people to get their booster shots. -
 2022-03-07
2022-03-07Maternity wards are shuttering across the US during the pandemic
This is a news story from Vox, written by Dylan Scott. Across the nation, maternity wards have been shutting down, making things more dangerous for new mothers. Due to these closures, there has been an increased number in deaths of both infants and pregnant women. These losses of maternity wards have been harshest on those of low income, as well as Black and Hispanic women. Part of these closures have happened due to shortages of doctors, nurses, and other hospital staff during the pandemic. The closure of more maternity wards also means women having to travel further to get the care they need. The timing makes this even more difficult during labor, as complications can happen during that, increasing chances of death. Overall, this article shows the ways that the ripple effects from COVID not only affect the mortality rates of mothers and babies, but disproportionately hurt poor, Black, and Hispanic women. -
 2022-03-31
2022-03-31COVID-19 and pregnancy: More new mothers dying, increasing women's fears during tense time
This is a news story from The Columbus Dispatch by Megan Henry. This story is about the rising fears of new mothers as COVID has increased their chances of dying. In 2020, motherhood mortality rate increased by 20% in the United States. There were also large disparities in who died, with Black women dying three times the rate of White women during pregnancy. Dr. Jason Melillo, an OB-GYN for OhioHealth claims that COVID is the main culprit for the rise in pregnancy related deaths. Pregnant women are more prone to complications from COVID, with things such as blood clots, stillbirth, and preeclampsia happening more often. This concern has made some couples only deciding on pregnancy until they have both been vaccinated. Dr. Melillo hopes that over time, mortality rates associated with pregnant women will go down. -
 2022-01-19
2022-01-19Man Calls Out PM Orbán after Mother Dies from Coronavirus
This is a news story from Hungary Today by Júlia Tar. A man's mother and sister from Nagykanizsa both died from the Coronavirus. Later, this man calls out Prime Minister Viktor Orbán because he believes PM Orbán did not properly protect his family. His mother was vaccinated with Sinopharm, a Chinese vaccine. The PM himself received Sinopharm as his first two doses, with Moderna as his third dose. The man describes feeling hurt seeing his mother die in the hospital after she contracted the Coronavirus. -
 2022-03-17
2022-03-17Working Remotely, Some Transgender People Saw an Opportunity to Change
This is a news story from the New York Times by Jenny Gross and Alyssa Lukpat. This story is about people that have transitioned during COVID, or before that, and their work experiences. Some of the data present is interesting to look at. In 2021, healthcare providers reported a stronger demand for confirmation surgeries compared to 2020 when many elective surgeries were postponed. Though, demand was even higher in 2021 compared to 2019, before the pandemic. Some doctors say that this influx is partly due to surgeries being postponed, but there are other explanations. At Mount Sinai Hospital in New York City, the Center for Transgender medicine and surgery performed a total of 938 surgeries in 2021, 60 percent more than the previous year, and 43 percent higher than 2019. While there is this influx, the story links to a YouGov poll showing that many Americans are still divided on if others should be legally allowed to switch their sex. The article then goes on to discuss other inequalities trans people face, such as earning 32 percent less than the general population. Trans people are also twice as likely to be unemployed compared to the general population. Later on, there is a discussion on what trans people face in the workforce. Even in more liberal and progressive work environments, some trans people still report feeling unsafe working in person. There are complaints that diversity training in the workplace focuses mainly on gays, but glosses over trans people and their issues. Other trans people, like Rae Lee, fears she will be fired if she came out to public administrators. Working from home has allowed Rae Lee to feel safer. -
 2022-03-16
2022-03-16Sign in Staff Area of St. Olav's Hospital
This sign is located in the staff area of St. Olav's Hospital in Trondheim, Norway. This photo was taken on March 16th, 2022 inside of a staff-only area. The sign reads as follows: Habits that prevent infection Paper tissues Cover your mouth and nose to protect others when coughing or sneezing. Through away the tissue after use. Then wash your hands. Use the hook of your elbow When you need to cough or sneeze and you do not have a paper tissue. Wash your hands With hand sanitizer when hand washing is not possible; for example, when traveling. In 2022, many places in the world have taken down signs and other precautionary rules that have to do with limiting the spread of coronavirus. This sign, which can only be seen by hospital staff, shows how precautions are still being enforced for hospital staff. This is important as it shows what rules and regulations are still being enforced in 2022. -
 2022-03-16
2022-03-16Sign at St. Olav's Hospital
This photo was taken in the lobby of St. Olav's Hospital in Trondheim, Norway on March 16th, 2022. The signs reads as follows: INFORMATION WEAR A MASK - Available at the front desk DO NOT ENTER IF YOU - Have symptoms of COVID-19 - Tested positive for COVID-19 - Had contact with a corona positive patient Please arrange visits with the ward in advance. I believe that this is important because this shows have precautions are being taken in the hospital in 2022. In many parts of the world, two years into the pandemic, a lot of rules and regulations regarding the prevention of COVID-19 have relaxed. In some cases, there are no precautions at all. This sign shows have precautions are still being taken in a major hospital by requiring masks and asking people who have been exposed to not enter the hospital. -
 03/30/2020
03/30/2020Jeanie and Edward Lehew Oral History, 2020/03/30
This is interview from Edward and Jeannie Lehew focuses on the COVID-19 pandemic experience in the United States. The Lehews, both born in the 1930s, provide an enriching interview connecting the current pandemic to past historical and personal events ranging from the Great Depression to the loss of an infant grandchild. The Lehews detail many personal life experiences and offer their opinions on the current political and healthcare issues in the United States by explaining how the current presidential administration is at fault for the lack of medical supplies in America. -
 2021-03-14
2021-03-14Paradigm Shifts
The COVID-19 pandemic has brought about many paradigm shifts; everyone I know has undergone a lot of change in themselves, their beliefs, and in how they view and interact with the world. There is a lot of grief these days but there are changes worth being happy about. -
 2021-09-24
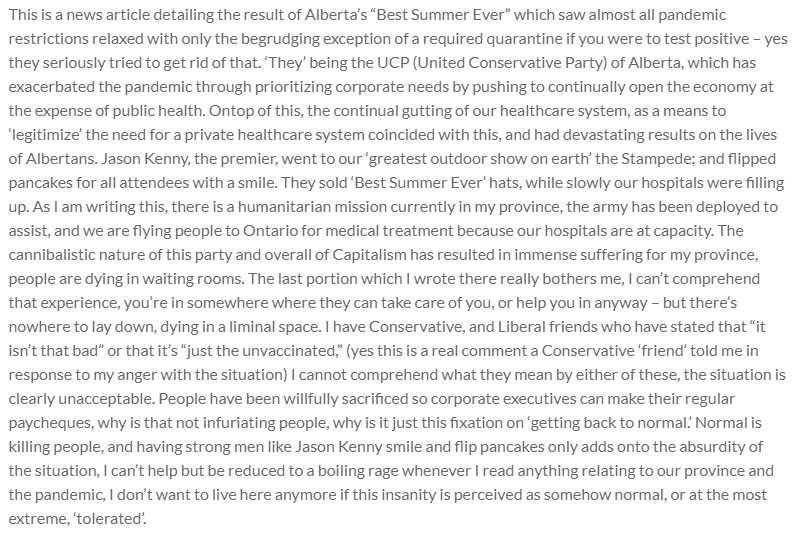
2021-09-24Best Summer Ever
This is a news article detailing the result of Alberta’s “Best Summer Ever” which saw almost all pandemic restrictions relaxed with only the begrudging exception of a required quarantine if you were to test positive – yes they seriously tried to get rid of that. ‘They’ being the UCP (United Conservative Party) of Alberta, which has exacerbated the pandemic through prioritizing corporate needs by pushing to continually open the economy at the expense of public health. Ontop of this, the continual gutting of our healthcare system, as a means to ‘legitimize’ the need for a private healthcare system coincided with this, and had devastating results on the lives of Albertans. Jason Kenny, the premier, went to our ‘greatest outdoor show on earth’ the Stampede; and flipped pancakes for all attendees with a smile. They sold ‘Best Summer Ever’ hats, while slowly our hospitals were filling up. As I am writing this, there is a humanitarian mission currently in my province, the army has been deployed to assist, and we are flying people to Ontario for medical treatment because our hospitals are at capacity. The cannibalistic nature of this party and overall of Capitalism has resulted in immense suffering for my province, people are dying in waiting rooms. The last portion which I wrote there really bothers me, I can’t comprehend that experience, you’re in somewhere where they can take care of you, or help you in anyway – but there’s nowhere to lay down, dying in a liminal space. I have Conservative, and Liberal friends who have stated that “it isn’t that bad” or that it’s “just the unvaccinated,” (yes this is a real comment a Conservative ‘friend’ told me in response to my anger with the situation) I cannot comprehend what they mean by either of these, the situation is clearly unacceptable. People have been willfully sacrificed so corporate executives can make their regular paycheques, why is that not infuriating people, why is it just this fixation on ‘getting back to normal.’ Normal is killing people, and having strong men like Jason Kenny smile and flip pancakes only adds onto the absurdity of the situation, I can’t help but be reduced to a boiling rage whenever I read anything relating to our province and the pandemic, I don’t want to live here anymore if this insanity is perceived as somehow normal, or at the most extreme, ‘tolerated’. -
 2020
2020My Mom Working in the COVID ICU
While this is not me, it is still important to me since it is my mom. She has worked in the COVID ICU almost the entire time, and I was really affected by seeing her gowned up like that the first time. Her career during my lifetime has not required so much PPE, so it was a really surreal moment that forced me to really appreciate the extremity of the pandemic and how much danger my mom was in. -
 2021-10-08
2021-10-08Idaho and the Overrun Hospitals
Idaho hospitals are so overrun with Covid patients and so understaffed that they are drowning. Idaho has one of the lowest vaccination rates in the nation and many people are getting sick. Many hospitals on the border Idaho shares with Washington are choosing to send their sick patients to Washington. This in turn is adding to the burden carried in Eastern Washington. Many healthcare workers in Idaho are burnt out and they are helpless because of the divisiveness caused by politics and Covid. -
 2021-09-29
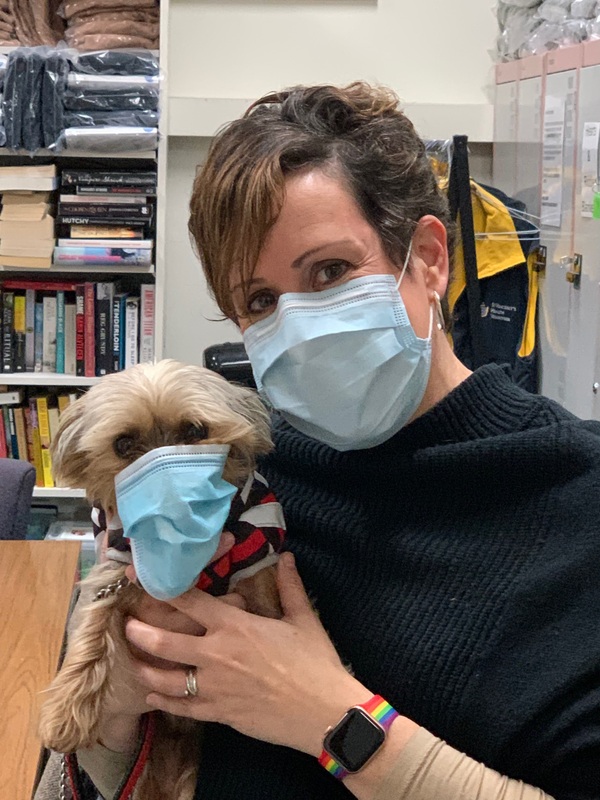
2021-09-29St Vincent's Hospital Melbourne masked up therapy dog Macca with hospital Volunteer Services Coordinator
Therapy dog Macca lifts the spirits of all whom he encounters and he has proven to be a greater stress reliever for staff working longer and harder due to the pandemic. The true magic of Macca’s contribution has been visible at the bedside. There have been patients who have spoken their first words after surgery while holding Macca and others who have been unable to use their arms who suddenly move to pat him. In recognition of his work he was crowned "Top dog with a job" from a field of 500 in the inaugural "Oz Top Dog Award" in September 2021. This was welcome good news in a difficult week where there was a surge of cases in Victoria's third wave. Macca's story attracted diverse media coverage including features in "The Herald Sun", ABC Radio 774 Melbourne and Channel 10 News. -
 2021-03-31
2021-03-31Gyre Oral History, 2021/03/31
Self-Description: “My name is Gyre. I am a multidisciplinary artist based in South Africa with global ambitions. I specialize in music, but I also work as a freelance writer as well as in dance. I’m a dancer learning to choreograph. Political commentator, particularity with regard to the LBGTQA+ community. I identify as queer. I am homoromatic and homosexual at this point in my life. You never know honey, it’s a spectrum. I had my first venture into artistic expression that is rooted in queer rights and queer understanding and queer theory, was my debut album, titled Queernomics, which was a documented audio-visual book about the contemporary experiences of a Black queer South African male, and that has gotten me into the positions that I express myself in, both out of passion and out of profession. Inkosi Yenkonkoni, which means “The Gay King”, in my native language which is Zulu.” Other details available here: Works produced during the pandemic: Kithi, International LGBTQ+ Rights Festival, writing on football. Some of the things we spoke about included: “What happens at the top is just politics, what happens at the bottom is real life.” Thinking about the term “pandemic” Listening to the body The pandemic exposing state corruption Having written a song called “Quarantine” in 2018 The inadequacies and privileges of Medical Aid in South Africa, having aged out of Medical Aid before COVID, the personal impact of worse-health insurance during pandemic, the importance of demonetizing health care Pre-COVID keeping busy: organizing, walking, collaborating Transit during COVID, sub/urban and outskirt disparities Canceling shows and taking dance classes and rethinking what it means to be productive Global Americanization and the impact of Trump’s pandemic denialism on South African health Moving out of disbelief about the severity of COVID after losing a loved one in the first wave Gratitude for the global influence of the Black Lives Matter movement, and sadness that tragedy in the diaspora brings neocolonialism to the fore The importance of social media for queer counter-violence and activist fractures among LGBTQA+ Feeling allyship with the #metoo movement How homophobia intersects with everyday altercations about social distancing The anxieties of hooking up during the pandemic The importance that scientists learn to speak in lay terms about climate change and vaccines Existence as resistance and creating art “Spread love not tolerance” Other cultural references include: Trans Day of Visibility, astrology, and the TV series Pose. -
2020-03
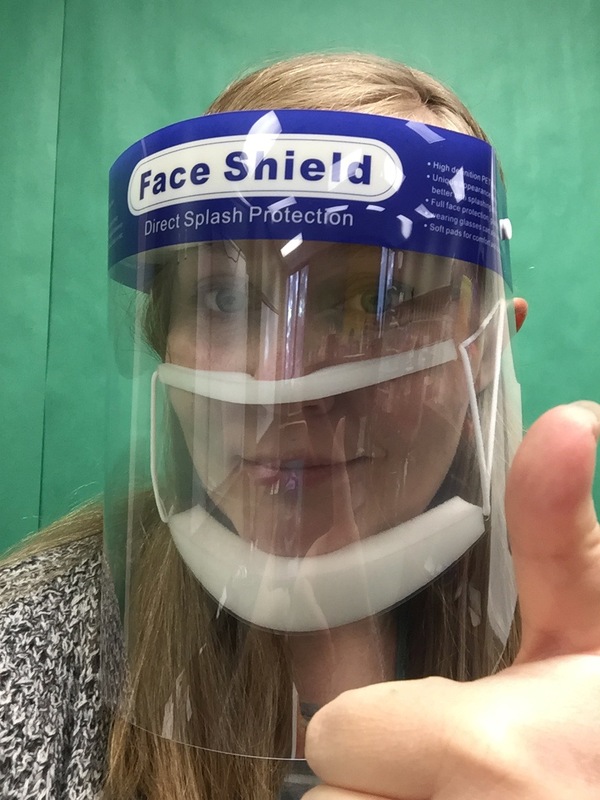
Recollections from an Oncology Nurse
My mom is an oncology nurse and has worked in the field of nursing for the past 30 years. I recently asked her to talk to me about her experience this past year as a healthcare worker. She recalled the first week in March when things were becoming intense. People were asked to wear face shields and gowns as they were working in an immune-compromised area where the patients had cancer. At the time there was no vaccine. “It was incredibly intense and scary” my mother said. “People were worried about getting Covid from other staff at the hospital and also worried about contracting Covid from the patients.” “I walked into the hospital and there was an incredible underlying anxiety, the feeling of unease was palpable. People did not talk to each other like they normally did - everyone was consumed with the thought of not using each other’s pens, putting gloves on when receiving things from the pharmacy. Things we would never have even thought of before.” She continued, “It was a feeling of both being unsettled and a blind trust you put in your coworkers to be as clean, as responsible and in isolation outside of work as you. The intensity of that feeling was there the moment you walked in. The environment had changed. People were not as happy, communicative, relaxed.” She explained how working in Covid - there was an incredible newness to it - a fear and apprehension. -
 2020-11-11
2020-11-11Holyoke Soldiers' Home Coalition Website
The Holyoke Soldiers' Home coalition created this website in response to the COVID-19 outbreak at the Holyoke Soldiers' Home in Holyoke, Massachusetts. It provides updates on the efforts to build a new facility, the motivation for constructing a new and larger facility, the need for more staffing, and the possibility of new programs. -
 2020-11-10
2020-11-10"Those who died during COVID-19 outbreak at Holyoke Soldiers' Home honored with virtual tribute"
This MassLive article reports on a coalition attempting to memorialize the veterans at the Holyoke Soldiers' Home in Holyoke, Massachusetts, who had died throughout the pandemic, most of them as a result of contracting COVID-19. -
 2020-10-06
2020-10-06"Staffing concerns predated coronavirus outbreak at Holyoke Soldiers' Home
This MassLive article reports on a pre-existing staffing shortage at the Holyoke Soldiers' Home in Holyoke, Massachusetts, that influenced the gravity of the COVID-19 outbreak in the facility. -
 2020-10-20
2020-10-20"Bennett Walsh resigns as Holyoke Soldiers' Home superintendent; suit over firing dropped"
This MassLive article reports on Holyoke Soldiers' Home superintendent Bennett Walsh's decision to drop a law suit after Massachusetts Governor Charlie Baker had him fired in light of the facility's poor response to the pandemic. -
 2020-09-13
2020-09-13"Plight of Holyoke Soldiers' Home residents, families becomes political flashpoint in state Senate race"
This MassLive news article discusses how a state senate candidate was using the poor response to the pandemic at the Holyoke Soldiers' Home during his opponent's term in office to gain popularity for himself. -
 2020-06-25
2020-06-25"Holyoke Soldiers' Home investigation: 6 takeaways from Mark Pearlstein report on coronavirus outbreak"
This article comes from MassLive and reports on the major takeaways from a report that documents where the Holyoke Soldiers' Home in Holyoke, Massachusetts, failed in its COVID-19 response. -
 2020-04-28
2020-04-28"Coronavirus at Holyoke Soldiers' Home: 2 more veterans die in worst outbreak at health care facility nationwide
This article, published by MassLive, reports on the rising death count among residents at the Holyoke Soldiers' Home in Holyoke, Massachusetts. Nearly three-quarters of the residents had contracted COVID-19, and about one-third had died from it. The title is evocative of the scale of the tragedy. -
 2020-04-20
2020-04-20"Coronavirus at Holyoke Soldiers' Home: Flags to fly at half-staff after at least 52 veterans die of COVID-19
This article, produced by MassLive, reports on Massachusetts Governor Charlie Baker's decision to have flags flown at half-mast at the Holyoke Soldiers' Home in Holyoke, Massachusetts, to commemorate the veterans who had died at the facility from COVID-19. -
 2020-04-06
2020-04-06"Coronavirus: Holyoke Soldiers Home residents struggle with relocation as one-third of residents infected with COVID-19
This article produced by MassLive reports on the efforts to relocate residents from the Holyoke Soldiers' Home in Holyoke, Massachusetts, to Holyoke Medical Center in attempt to mitigate the spread of the virus after 76 of the 210 residents had already tested positive. The article also discusses the continued investigation into the COVID-19 situation at the home. -
 2020-04-03
2020-04-03"Coronavirus: Western Massachusetts legislators call for 2nd investigation into Holyoke Soldiers' Home COVID-19 Deaths"
This article published by MassLive reports on local legislatures' desire to issue a second investigation into the COVID-19 response at the Holyoke Soldiers' Home in Holyoke, Massachusetts, in light of the number of deaths among residents and the number of cases among residents and staff. -
 2020-03-31
2020-03-31"Coronavirus: Holyoke Soldiers' Home superintendent placed on leave, at least 5 residents die from COVID-19"
This article published by MassLive.com reports on the suspension of the superintendent of the Holyoke Soldiers' Home in Holyoke, Massachusetts, after several residents died and numerous other residents and staff members tested positive. -
 2020-03-31
2020-03-31"Coronavirus: 'We were just shocked' to learn of Holyoke Soldiers' Home deaths, Mayor Alex Morse says"
This article describes Holyoke mayor Alex Morse's reaction when he found out about the magnitude of the COVID-19 situation at the Holyoke Soldiers' Home. -
2020-03-12
"Coronavirus in Massachusetts: Soldiers' Home in Holyoke limits visiting hours, screens visitors"
This article appeared on MassLive on March 12, 2020. It discusses the safety precautions that went into effect at the Holyoke Soldiers' Home in Holyoke, Massachusetts. The article acts as context for the tragedy that would unfold at the home within the first few months of the pandemic. -
 2020-08-11
2020-08-11Nurse handover Emergency Department, St Vincent's Hospital Melbourne
This photograph was taken in August 2020, the time when daily and active cases in Victoria's second wave were at their peak with hospitals adapting services and protocols in response. The photograph shows a nurse handover in the hospital's Emergency Department. The red line on the floor marks the boundary of the "hot zone" area dedicated to the care of patients regarded as infectious. Staff wear prescribed Level 4 PPE (Personal Protective Equipment) of gowns, face protection and N95 masks. -
 2021-07-24
2021-07-24Joseph Dopkin, Oral History 2021/07/24
Ashley Tibollo sits down with Joseph John Dobkin to discuss how his life has been impacted by the COVID-19 pandemic. In this interview his discusses how his life at school as a University student has changed. He also discusses how the dynamics in his dorm room and life at home with his family were impacted. At the end of this interview Dobkin touches on political topics, his views on how the pandemic was handled by local and state governments. He also discusses his views on both anti-mask and BLM protests. -
 2020-12-22
2020-12-22The Virus Is Showing Black People What They Knew All Along
In this article, author Patrice Peck discusses how black Americans are dying of COVID-19 at 1.7 times the rate of whites. In her words "19,000 Black people would still be alive if not for systemic racism." -
 2020-04-16
2020-04-16Infographic: 8 Big Ways Coronavirus Impacts Latinos
This infographic and the accompanying articles discuss the disproportionate impact that coronavirus has on Latino communities. -
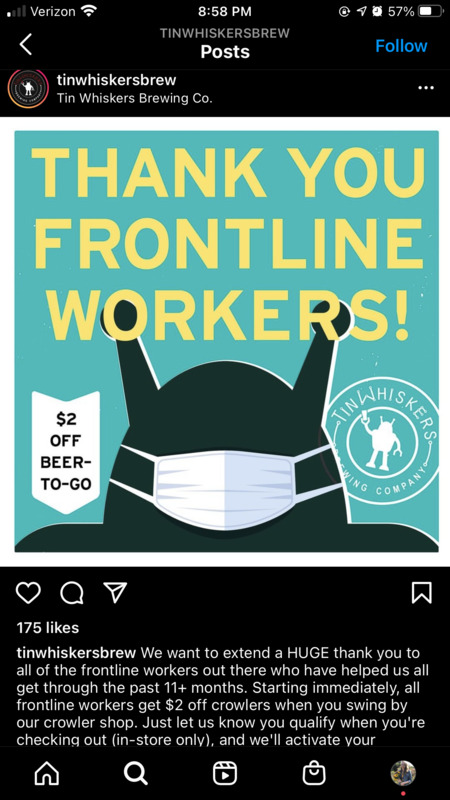 2021-02-03
2021-02-03Tin Whiskers Brew Offered Frontline Workers Discount on Beer
To thank those risking their health for the benefit of others, Tin Whiskers Brewing Co. in Saint Paul, Minnesota showed their appreciation by offering a discount on take-out beer to frontline workers. They included health care workers, educators, first responders, service industry workers, postal workers, and public transit workers in their list, and were open to suggestions to add to that list. While a discount on beer doesn't make up for all the work these individuals do, it is a nice gesture to show appreciation during this challenging time. Given that those working in this brewery are also service industry workers, they recognize the risks and difficulties that frontline workers have been experiencing, and wanted to make it clear how much these people do for society. Instagram caption: @tinwhiskersbrew We want to extend a HUGE thank you to all of the frontline workers out there who have helped us all get through the past 11+ months. Starting immediately, all frontline workers get $2 off crowlers when you swing by our crowler shop. Just let us know you qualify when you're checking out (in-store only), and we'll activate your discount. What constitutes a frontline worker? --Health Care Workers --Educators --First Responders --Grocery/Retail/Pharmacy/Liquor Store Employees --Bar/Brewery/Restaurant Service Industry --Postal Service/Delivery --Public Transit Workers If we missed a field, let us know! We definitely want to thank you too. -
 2021-04-18
2021-04-18What made California’s vaccine rollout so difficult?
The Golden state only recently received news that “50% of all eligible Californians have received at least one dose of the COVID-19 vaccine." It’s progress and it’s most certainly hope. What gives people even more hope is how they expanded vaccination eligibility to 16 and over as of April 15. Schools are already reopening, but this is good news for those who are still hesitant to return — and for good reason. What made California’s vaccine rollout so difficult? One of the most obvious answers is the size of the state. Its population was recorded to be over 39 million in 2020. Even with an increase in vaccines, with roughly 2.4 million doses in the first week of April alone, it was not enough to accommodate even the 50-64 age group — a population of roughly 7.2 million. Santa Clara County Executive Officer, Jeff Smith, was also quoted to have cited the state's governor for perpetuating the pandemic — that his pandemic approach was “disorganized and petulant.” Although affordable healthcare services is a nationwide pandemic in and of itself, California also deals with fragmented healthcare responsibilities. Distribution is “split up among 58 county governments.” Issues in communication, planning and transportation of vaccines are all major factors impacted by the overwhelming lack of unified leadership. https://twitter.com/CAgovernor/status/1383132361148100609 https://www.gov.ca.gov/2021/04/01/as-california-expands-covid-19-vaccine-eligibility-to-all-californians-50-governor-newsom-receives-vaccine-in-los-angeles/ -
 2021-04-11
2021-04-11Indirect acute effects on physical and mental health
This academic article is in the Lancet, a medical journal. I chose this because it is public, unlike some academic articles, and it is, as of right now, a pretty unique research article. Although it is done in the UK, it reviewed medical records, both physical and mental, from 2017 to 2020. The changes are a little surprising, as the largest reductions in health care at the start of the restrictions were diabetic emergencies, depression, and self-harm. This is something I have seen a lot in my research into the unintended consequences of the COVID-19 pandemic. Mental illness is the last thing to be cared for in a pandemic, or even in other natural disasters. The consequences on human health from this pandemic are only just now coming to light. This journal entry covers in-depth research and I highly suggest it.
