Items
topic_interest is exactly
public health
-
 2022-06-12
2022-06-12Trip to Chania, Crete: Wedding of the Century for the Family
This was the first travel for me and my family when COVID-19 restrictions relaxed to a thoughtful degree. This is important to me because it was a time that my extended family came together and the appreciation of that was heightened by the absence of togetherness through out the more critical time of the pandemic. -
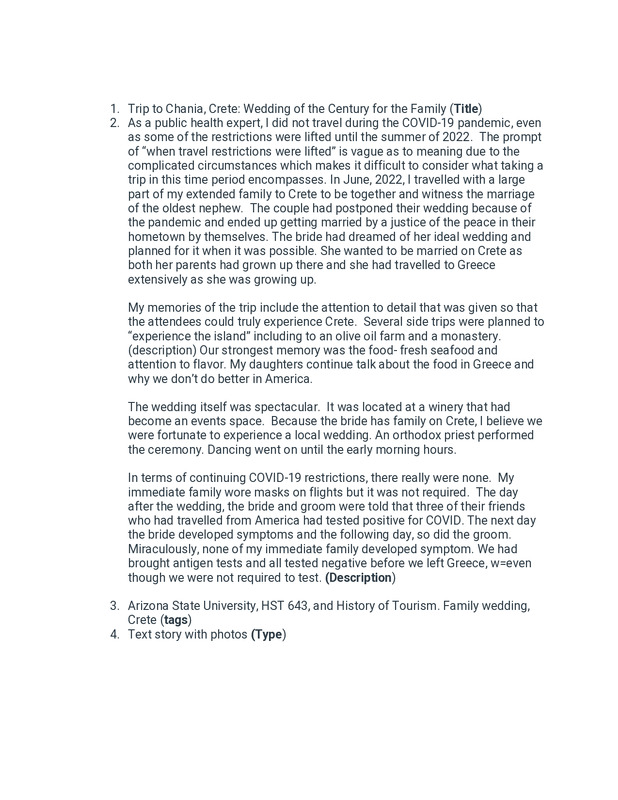
 2022-07-08
2022-07-08NYC officials recommend masks indoors due to COVID surge
This is a news story from Axios by Herb Scribner. Due to a rise in COVID cases, health officials in New York City are recommending that people wear high quality face masks indoors or in crowded areas. A CBS News report says that COVID positivity rates have risen 14%, the highest level since January. A subvariant of Omnicron, BA.5, has been responsible for 54% of total COVID cases, according to the CDC. -
 2022-06-26
2022-06-26Remember when it wasn't "your body, your choice"?
This is an Instagram post from dontfollowpatrick. This is a meme posted regarding bodily autonomy. For pandemic skeptics, "my body, my choice" has been common rhetoric with things like masks and vaccines. Dissenters claim that it is not a valid argument because the actions of one person in a public health crisis affect other people around them. With things like abortion, it is seen as an individual decision that does not affect others the way not wearing a mask would. -
 2022-05-26
2022-05-26Tucker Carlson tries to link Uvalde massacre to COVID "lockdowns" while rejecting gun restrictions
This is a news story from Salon by Meaghan Ellis. This is an opinion piece on what this author thinks about Fox News contributor Tucker Carlson and his approach to the shooting in Texas. The news story says that Carlson claims the lockdowns increased mental illness cases. Whether this is true remains to be seen, but from my own experience with lockdowns, I did have trouble adjusting. I had at least a few mental breakdowns over feeling like a prisoner in my own home. I don't think the lockdowns would trigger everyone into becoming a potential mass shooter, but I do not think they were healthy for many people either. People need human contact regularly, and being cut off from that and only having social media or very few people to see in-person would feel isolating. I think mental health is not paid attention to enough by public health officials when it comes to lockdowns. Mental health is still part of overall health. I do understand why the lockdowns happened, but I think many went on too long, which has had a bad effect on society. It is obviously not the only reason someone would have a mental illness, but for people that already did have mental issues, it made them worse. I have high functioning autism and without a good support system, I'd possibly be doing way worse. -
 2022-05-25
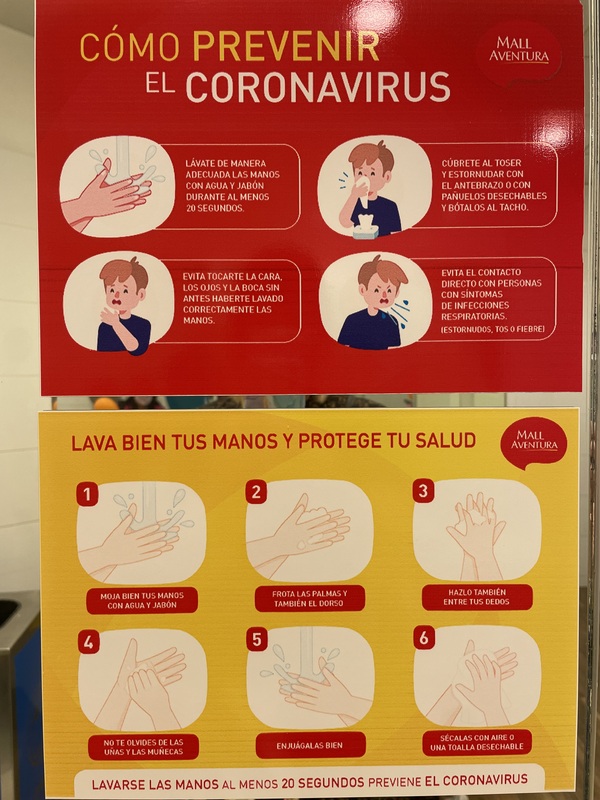
2022-05-25Vaccine check control at mall Aventura
All guests have to have 3 vaccines and an N-95 or double facemask to enter the mall. The flow of in and out of the mall are still controlled. -
 2022-05-12
2022-05-12Hygiene precautions Mall Aventura
These instructions are posted on the mirror in the kids' bathroom at Mall Aventura in Arequipa, Peru. -
 2022-05-05
2022-05-05New York City could bring back Covid mask mandate, vaccine checks if hospitals come under pressure
This is a news story from CNBC News by Spencer Kimball. New York City might bring back the mask mandate and vaccine checks if hospitals become too overwhelmed. New York City increased its COVID alert level from low to medium earlier this week as infections have kept on rising. Health Commissioner Ashwin Vasan said New York might reinstate mandatory masking and vaccine checks if the city raises its Covid alert level to high. New York's alert system is based off of CDC guidance and hospital protocols. Mayor Eric Adams ended mandatory vaccine checks at restaurants and other indoor venues in March, in addition to the mask mandate for people attending school. Masks are still required on buses, rail, and on subways in New York City. New York City, as of right now, has 80% of their population fully vaccinated. -
 2022-04-22
2022-04-22Fauci slams ‘no experience’ Florida judge who nixed mask
This is a news story from the New York Post by Yaron Steinbuch. Dr. Anthony Fauci has went against what the Florida judge has said against the mask mandate. He says that she does not know enough about health to make a decision. The judge's decision has also sparked a response from the White House. On Wednesday, the Justice Department filed a notice that it will appeal US District Judge Kathryn Kimball Mizelle’s ruling at the behest of the Centers for Disease Control and Prevention. -
 2022-04-13
2022-04-13The 11% Lunatic Fringe
This is a Twitter update by WaytowichNeil. This user is ranting on what he calls the "selfish 11% lunatic fringe." To him, this fringe group is what is causing more problems with fighting COVID. In contrast, he says that 89% did everything they were asked. His frustration is coming from the belief that it is only the fringe deciding public health policy these days. -
 2022-04-15
2022-04-15It’s time to think outside the mask mandate
This is a news story from Vox by Keren Landman. The author interviews an epidemiologist on new solutions to tackling the virus that do not require shutting things down or forcing masks. The epidemiologist, Jennifer Nuzzo, says that instead of forcing masks, make things more equitable with having rapid testing more readily available, in addition to vaccines, so that people can continue on with their lives without as much interruption. She believes that masks and lockdowns are okay short-term when not much is known about the virus, but since we know more now, and have more testing, vaccines, and treatments, that we do not need these things. Luzzo thinks we should focus on low-access places so that more people have a chance of protecting themselves. -
 2022-04-08
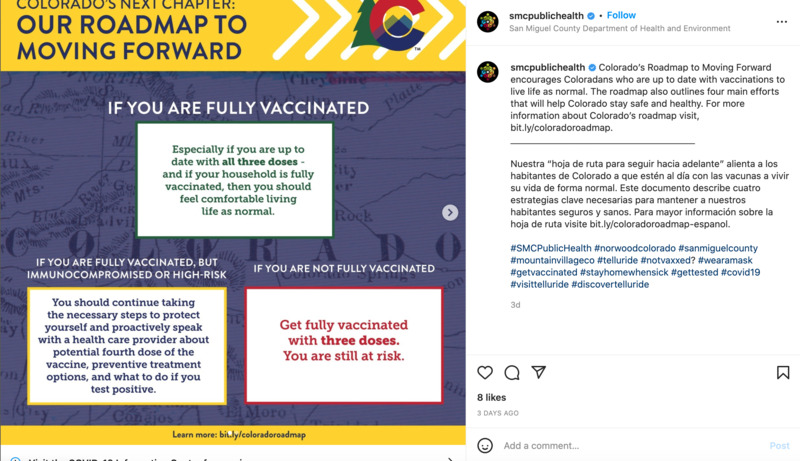
2022-04-08Our Roadmap Moving Forward
This is an Instagram post by smcpublichealth. This post is about vaccination status and the risks that they pose. Those unvaccinated are said to be highest risk. The immunocompromised are recommended to see a doctor about a fourth dose. If you are up to date on all vaccines and everyone else in the household is vaccinated, life can continue on as normal. In the hashtags below this post, it says to wear a mask, stay home when sick, and get tested. Obviously, despite it saying that those that are up to dates on vaccines and live with those also fully vaccinated are able to return to normal, culturally, I have seen some people out in public abiding by COVID restrictions. I think this is a hard habit to break, and for some, the feeling of security is worth continuing to wear a mask even if some places have already lifted mandates. My overall feeling from observing those at my own local church is that people are more lenient with mask use based on what the CDC says. A few did not wear masks despite the CDC recommendation, but once the CDC announced masks were not necessary, people at my church took them off. -
 2022-04-11
2022-04-11COVID-19 Testing
This is an Instagram post by medrite_springfieldnj. This is a PSA welcoming people to get free COVID testing. It says that no appointments necessary and walk-ins are welcome. Since the start of the pandemic, rapid testing and PCR tests have become more available and free of charge in many places. The reason many of these are free is due to state and federal governments subsidizing the costs of the tests, in addition to people volunteering to help them get done. -
 2022-04-07
2022-04-07Where the Government Requires Masks
This is an Instagram post by urbanpeaceinstitute. This post refers to places where mask mandates are still in existence. Even though mask mandates have been lifting in many places, certain places still want masks. Some of these places include: emergency and homeless shelters; public transit; healthcare settings; long-term care facilities; and correctional and detention facilities. These places are either government or healthcare associated. This post links to the County of Los Angeles Public Health for more information on the Coronavirus. -
 2022-03-14
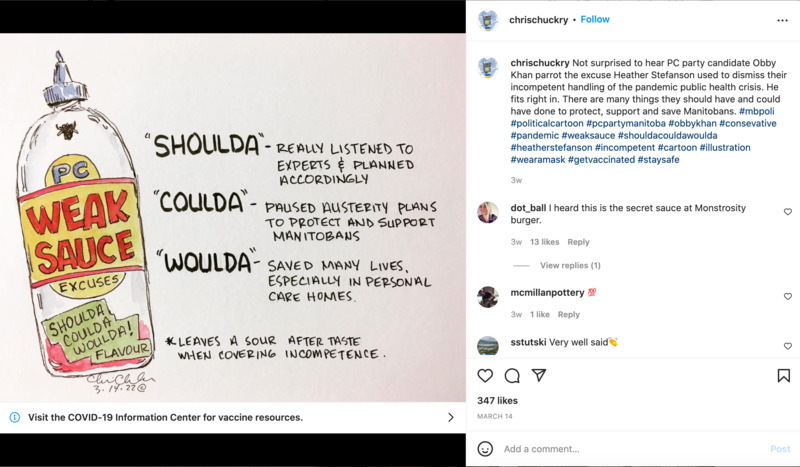
2022-03-14Weak Sauce
This is an Instagram post by chrischuckry and it is a political comic on the incompetence on part of the Canadian government and the handling of the pandemic. Obby Khan, who is referenced in this post, is a Pakistani-Canadian politician. This user is accusing him of using the same excuses as Heather Stefanson, who is the premier of Manitoba, a Canadian province. The political comic is upset about politicians in Manitoba "not listening to experts" and allowing the pandemic to become more dangerous. -
 2021-04-03
2021-04-03The whitewashing of Arab Americans impacted by Covid-19 is a catastrophic public health issue, experts say
This article brings up important points regarding the underrepresentation of Middle Eastern and North African (MENA) people and communities in U.S. This article focuses primarily on Arab Americans, but also sheds light on the fact that there are no identifiers for Middle Eastern and North African people on the U.S. Census as their only options are to choose “white” or “other”. As a result, there is a lack of Covid-19 data specific to these communities which prevents support and information being directed to those underrepresented – and often socioeconomically underprivileged – groups. This article is important in demonstrating the vulnerability of this group. Many MENA families live in multi-generational homes, have preexisting medical conditions or risk factors which may make them more vulnerable should they contract Covid, and still some do not have access to the information and support needed to prevent Covid or to receive the proper treatment if infected. Additionally, because MENA people are not able to self-identify on the U.S. Census, the information about how these communities are being affected is not accurate. The U.S. Census isn’t the only place where these identifiers do not exist. Job, scholarship, and college applications (to name only a few) do not provide accurate identifiers for MENA individuals. I think this article is important in revealing the lack of identifiers available to MENA people and how important it is that this is changed soon. -
 2022-01-19
2022-01-19Man Calls Out PM Orbán after Mother Dies from Coronavirus
This is a news story from Hungary Today by Júlia Tar. A man's mother and sister from Nagykanizsa both died from the Coronavirus. Later, this man calls out Prime Minister Viktor Orbán because he believes PM Orbán did not properly protect his family. His mother was vaccinated with Sinopharm, a Chinese vaccine. The PM himself received Sinopharm as his first two doses, with Moderna as his third dose. The man describes feeling hurt seeing his mother die in the hospital after she contracted the Coronavirus. -
 2020-06-08
2020-06-08Racism like Public Health?
Amidst Covid-19, the documentation of the police killings have been manifested into comparisons with the world-wide pandemic. These comparisons reflect the ongoing disparities between Black Americans and systemic racism. The Institute for Health Metrics and Evaluation takes to Twitter to try to support this comparison but faces a backlash from a fellow BLM support who argues that the comparison is invalid based on the different progress the BLM protest and quarantine had made. I felt like this was important for me to post because I feel like it shows an effort from BLM supporters to combat the racism within our culture by arguing that society must view and address racism as a public health issue. Yet, the tweet continues to evolve as ironic as the lack of regards Americans have for coronavirus policies and laws continues to grow everyday. Base on how events go, we might regard the validity of this statement to be false down the road. -
 2021-05-16
2021-05-16Vaccine Hesitancy in the Black Community
This tweet reflects an ongoing controversy of the Covid-19 vaccine. The media has reported a hesitancy of the mRNA vaccine amongst the black community, but with little to no context on why there is such hesitancy. Based on the history of the U.S. public health institution, there have been reported inequalities that include a racial hierarchy within the medical system. This tweet specifies the instances of medical malpractice committed towards people of color and insists on an understanding of racial inequality through the lens of people of color that led to skeptical feelings about the vaccine. -
 2021-08-25
2021-08-25ASU vaccine promotion banner
Classes at ASU started last week, since then, this banner has been hanging over the intersection of Mill and 5th in downtown Tempe. It reads, "Welcome Sun Devils, Forks up sleeves up." This banner is meant to encourage people moving through the area to get the COVID-19 vaccine. -
 2021-08-11
2021-08-11Exposure to covid in the classroom
I came across this conversation on a neighborhood app (Nextdoor) of a grandmother pleading for masks and vaccines after learning that one of her grandchildren was exposed to the virus in the classroom. I added a bit of the thread as well to show the different opinions on the matter. -
 2020-04-20
2020-04-20Nature can boost your mental health during COVID-19 pandemic
The pandemic has negatively affected many individuals' mental health. This article describes the benefits nature can provide in improving one's mental health during this time. -
 2021-02-25
2021-02-25The Role of Community Gardens During the COVID-19 Pandemic
The pandemic has brought the issues of food insecurity and the fragility of our food system to the forefront. This article discusses how household food insecurity disproportionately affects lower-income families and Black and Hispanic communities. Community gardens are one way to address these issues, providing mental health benefits, social and emotional support, and public health benefits during the pandemic. -
 2021-07-19
2021-07-19Erie County Health Equity
This Buffalo News article discusses the racial disparities impacting the residents of Erie County during the pandemic. The article claims that the pandemic shined a light on the racial disparities as more African American community members were becoming infected and dying from COVID. -
 2021-07-16
2021-07-16Arizona governor says schools can't force unvaccinated students to quarantine if they're exposed to Covid-19
This CNN article discusses a recent letter sent out by Gov. Doug Ducey's education adviser, that said requiring unvaccinated students to quarantine after a COVID exposure is against state law because Arizona does not require students to be vaccinated or wear face masks. I am from NYS and this is drastically different than what Gov. Andrew Cuomo is requiring and/or recommending for students in public schools and state universities. It is bizarre how different states and governors are handling the COVID and vaccination situation. -
 2021-04-02
2021-04-02Strength and Innovation of Indigenous Communities During the Pandemic
This article demonstrates that despite the inequities faced by Native Americans and indigenous populations they have been innovative in combatting the pandemic and shown strength in the face of fear, illness, and uncertainty. -
 2020-10-06
2020-10-06Medical School's response to Covid-19
Medical schools have had to come up with unique ways to continue to educate future physicians during the lockdowns and pandemic restrictions. This has not been an easy process, and it remains to be seen the long term effect of those who had to go through medical school during the pandemic. However, there will certainly be long-lasting changes to the ways in which we educate medical school students forever after. This article lists 5 ways in which medical school education will be impacted by the Covid-19 pandemic. They are an emphasis on public health, real-time curriculum adaptation, potential to reevaluate graduation requirements, changes in residency selection, and new approach to crisis management. It will be interesting to see how these things impact the quality of physicians down the road. -
 2021-04-20
2021-04-20Northern Arizona's Coconino County "Face It" Mask Campaign and Online Toolbox
The Coconino County Health & Human Services department created its "Face It" campaign in 2020 to promote the use of masks and face coverings in their communities. The following webpage is for the campaign's digital "toolbox" to give the public access to official signage for display to customers, the public, and employees to address mask use issues. -
 2021-04-19
2021-04-19Navajo Department of Health Public Health Emergency Orders through 19 April 2021
These eight documents are the eight Public Health Emergency Orders issued by the Navajo Department of Health issued through 19 April 2021. -
 2021-03-05
2021-03-05News Article: Gila County's COVID-19 efforts lead more urban counties
"By Christopher Brito, March 5, 2021, CBSnews.com While a majority of states and cities are still vaccinating higher priority groups of people, one county in Arizona is now allowing any resident over the age of 18 to receive the COVID-19 vaccine. Gila County, which is located east of Phoenix, entered Phase 2 of their vaccine prioritization late last month, opening up eligibility to the general population. Part of the the decision to open vaccine eligibility is because Gila County has one of the lowest percentages of COVID-19 vaccine doses used in Arizona. Michael O'Driscoll, director of Public Health and Emergency Management for the county, told CBS affiliate KPHO-TV that they received permission from the state last week to offer the vaccine in a drive-thru clinic last weekend. "Prior to that, we were struggling to find enough people to make appointments to that, so the state gave me permission to offer it to any resident 18 and older," he said. About 56,000 people reside in the county. According to the Arizona's Department of Health Services, more than 13,000 people – or almost one fourth of residents – have received at least one dose of the COVID-19 vaccine. "We did a survey before to get a sense of how many people in Gila County would consider getting the vaccine, and our survey came back about 50-60% of the residents would choose to get the vaccine if available," O'Driscoll said. Based on the data, over 5,600 people under the age of 65 have received the vaccine, including 73 people under the age of 20. One of the younger recipients, 18-year-old Jacob Jost, told KPHO-TV that he was "excited" to get the shot. "I have a little nephew, a little baby, so having the vaccine puts a peace of mind for that," Jost said. First published on March 5, 2021 / 12:13 PM © 2021 CBS Interactive Inc. All Rights Reserved. Christopher Brito is a social media producer and trending writer for CBS News, focusing on sports and stories that involve issues of race and culture. -
 2021-04-06
2021-04-06Gila County Health Department and COVID-19
The Gila County webpage provides clear and concise information for residents on COVID-19 updates, as well as specific data to allow residents who wish to be vaccinated to choose which manufacturer's product they receive. This is unlike any of the major Arizona county sites, or even the state's site, as they do not allow residents to differentiate between the vaccines. Additionally, the information displayed here demonstrates how far ahead rural Gila County is in achieving President Joseph R. Biden's directive to allow all adults in America access to vaccines by April 19. -
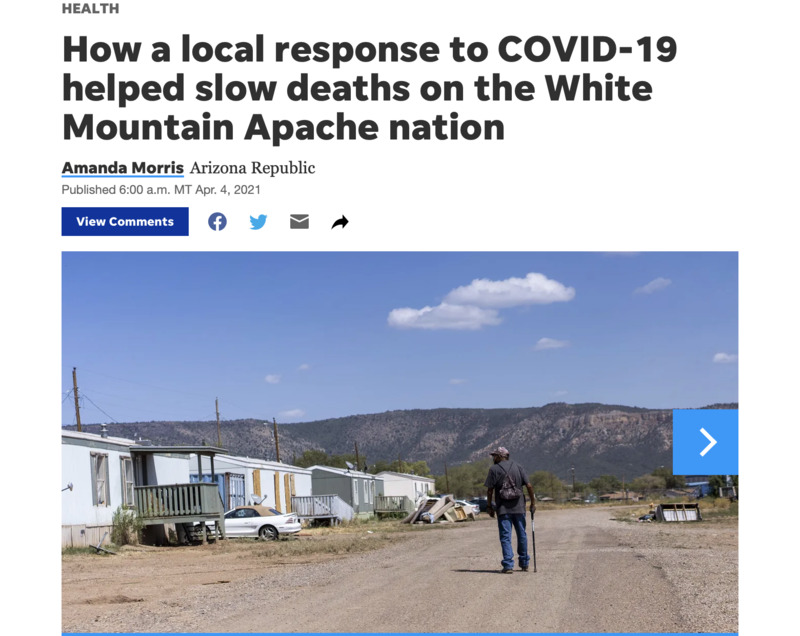 2021-04-04
2021-04-04News Article: How a local response to COVID-19 helped slow deaths on the White Mountain Apache nation
By Amanda Morris of the Arizona Republic: When someone on the Fort Apache Indian Reservation receives a confirmed diagnosis of COVID-19, health care workers from the Whiteriver Indian Hospital jump into action. They personally visit the individual's home to test other household members, perform health evaluations on everyone there and trace any other potential contacts at risk for COVID-19 exposure. Health care workers in the community say that could be one reason why, even though the rate of confirmed COVID-19 cases among White Mountain Apache tribal members is nearly triple the state's rate, the death rate is much lower and continues to fall. Over 90% of COVID-19 cases in the White Mountain community are investigated within 24 hours of testing, according to Ryan Close, the director of the Department of Preventative Medicine at the Whiteriver hospital, which is the only hospital on the 1.67 million-acre reservation. "I feel like what we did made a huge difference," Close said. "We evaluated and admitted people aggressively and early. The tribe deserves an incredible amount of credit for mobilizing staff ... to make this response possible, because at some point it would have been very difficult to maintain without their considerable help." The quick response may have also helped the tribe turn the tide against rapid community spread of the virus, which scientists say could have been fueled by a single variant found only in the White Mountain tribal communities. The variant carried a mutation in the spike protein, which scientist theorize could have made it spread more rapidly than other strains of the virus. The number of confirmed COVID-19 cases among White Mountain Apache tribal members accounts for 24% to 28% of their population, according to Close, but the cumulative death rate among known cases is only 1.2%. By comparison, the statewide rate of infection was 11.5% with a 2% death rate among known cases. And over the winter, Close said the rate for the tribe dropped even lower, to about 0.5%. In a community with a high number of individuals with underlying health conditions, the low death rate and work of the tribe has been "remarkable," said David Engelthaler, director of the Translational Genomics Research Institute's infectious disease division in Flagstaff. The death rate also stands out as unusually low when compared with death rates in other Indigenous communities. Indigenous populations have been disproportionally affected by the pandemic. CDC data shows that Indigenous people are 3.5 more likely to be diagnosed with COVID-19 and almost twice as likely to die from COVID-19 than white people. Close credits a proactive strategy to combat COVID-19 that involved rapid contact tracing, in-person health evaluations and frequent outreach to high-risk COVID-19-positive individuals as well as early treatment with monoclonal antibodies and other antiviral therapies. Volunteers and health workers from the White Mountain Apache community were on the Whiteriver hospital's contact tracing team and high-risk COVID-19 outreach team, which Close said helped the team connect better with the people and work faster. One essential part of the team are the tribe's community health representatives, or CHRs, who are members of the community that serve as a cultural bridge between patients and medical establishments. JT Nashio, director of the Community Health Representatives for the tribe, said the "visceral connection" that CHRs have to the community helps them bring cultural awareness to the way questions are asked for contact tracing, which makes the process more effective and allows officials to better distribute information. "On top of that, quite simply, they know how to get around. It’s a big reservation and not all homes are easy to find," Nashio said. "But when you’ve lived here your whole life, you know where to find people. That became invaluable during the tracing and testing push during case surges." Virus mutation may have made it more transmissible When COVID-19 hit the White Mountain Apache nation, it spread rapidly. The community's first documented case was on April 1, 2020, from someone who had likely recently visited the Phoenix area, unknowingly caught COVID-19 and returned, according to Engelthaler. Within the first few weeks, Close said the community experienced a handful of deaths. "We soon had incidence rates that were skyrocketing. Case counts were going up very, very quickly," Close said. It's unclear why the disease spread so rapidly in the community, but the initial strain of COVID-19 that hit the community carried a mutation that Engelthaler believes could have made it more transmissible. "They were seeing the virus just rip through and have an 80 to 90 to 100 percent attack rate," he said. TGen partnered with the tribe and the U.S. Indian Health Services early on to provide tests to diagnose a case of COVID-19 and provide genetic analysis of the virus from each case. It showed one strain of the virus circulating in the tribal community that wasn't present anywhere else in the state. "This virus moved much faster than anything else we were seeing in Arizona at the time," Engelthaler said. "So we actually believe that we had one of these variant strains in Arizona that was causing very large numbers of cases, but it was secluded and maintained really only in that tribal population." The mutation, called the H245Y mutation, occurred in the spike of the virus, which Englethaler said is a "very sensitive" part of the virus where mutations can have a significant impact. Because of the low death rate, Engelthaler said TGen researchers would like to investigate the mutated strain of coronavirus seen among tribal members to see if it is also associated with a lower fatality rate. He acknowledged that other strains of the virus have since entered the community and that the actions of health care workers in the community and at the Whiteriver hospital is also responsible for the lower death rates. 'The earlier you treat an illness, the better' Close's biggest concern was that an outbreak would cause a "tsunami" of sick COVID-19 patients that would run the risk of overwhelming the Whiteriver hospital, which does not have an intensive care unit. Any patients that require intensive care need to be transported to other hospitals in the state. "We're a small hospital, we cannot take a wave of all very acute patients because there aren't enough ventilators in the hospital," Close said. "There aren't enough helicopters in the state to transport people out from our facility to a higher level of care." Within the first few weeks, Close said the community experienced a handful of deaths, and patients who had the poorest outcomes were the ones who self-presented at the hospital — often meaning they waited until they felt sick enough to go to the hospital. "People don't always bring themselves in early enough," Close said. "The earlier you treat an illness, the better." In response to this phenomenon, the hospital started a high-risk outreach program the third week of April. Health care workers regularly visited the homes of anyone who tested positive for COVID-19 and was at high risk for a poor outcome. Close recalls multiple days when he evaluated patients and found their oxygen levels dangerously low, even though they felt fine. It's a condition associated with COVID-19 known as "silent hypoxia," or "happy hypoxia." "They had no sense that they were even ill. They went on to get pretty sick in the hospital, but they survived and you can't help but think to yourself, 'Yeah, that's a life saved,'" Close said. "That person, if they had stayed home another day or another two days would not have done as well. They would have ended up on a ventilator or something." The Arizona Republic previously reported that the effects of the high-risk outreach program and contact tracing led to a fatality rate among tribal members of 1.6% last June, which was less than the state's rate of 2.5% and country's at 2.7% at the time. But the effect of the outreach program became even more pronounced over the winter, as the tribe and health workers gained access to monoclonal antibody treatments, according to Close. He said the high-risk outreach team started referring patients for antibody treatment in December as part of their protocol after the therapy received emergency use approval from the Food and Drug Administration. Hospital staff at the Whiteriver hospital then administered the antibody treatment. "We give that to people who are asymptomatic or mildly ill to prevent hospitalization," Close said. "The evidence currently suggests that reduces the risk that they're going to get sicker and get hospitalized and reduces the risk that they're going to die." Though there's no data proving the antibody treatments made a difference, Close said that after health care workers started using them, the community's COVID-19 death rate fell to 0.5%. Hospital workers also gave antiviral therapies, such as remdesivir, to patients early and often. "We probably overtreated some people," he said. "But the good news is it definitely led to significant reductions in mortality." Lessons for the future Close believes the different programs were so successful because health care workers were often able to test, trace, diagnose and treat individuals all in the same day — a feat he said was only possible because of how closely integrated hospital workers and community health workers were. "There were no barriers in communication between the public health arm of our response and the clinical care arm of our response," Close said. "It's really a case for an integrated health care system." As the tribe emerges from the pandemic and tribal members get vaccinated against the virus, Close said the hospital may start exploring other health conditions where it can use the high-risk outreach team, which is already trained and experienced in clinical evaluations. "The goal is to take what we've learned from COVID and now apply it to things that are not COVID-related," Close said. Another valuable lesson Close hopes to carry forward is how much of a difference visiting residents in their homes can make and how important building trusting relationships with the community is. Nashio said going door to door to trace and monitor COVID-19 cases was a natural step for CHRs, who had already gone door to door in the past for other community health campaigns. "We know firsthand how difficult it can be to not only connect with patients over the phone but communicate effectively over the phone," Nashio said. "When the community sees their CHRs coming to their door, it helps decrease the stigma of the disease." In addition to performing checkup evaluations and providing information, Nashio said CHRs can also provide food, medical supplies, cleaning supplies or services like grocery shopping and running basic errands. Not every tribal member has reliable internet or phone service, nor access to transportation, so Close said going door to door can be a good way to reach, and help, everyone. "Meeting patients where they are is invaluable," Close said. Amanda Morris covers all things bioscience, which includes health care, technology, new research and the environment. Send her tips, story ideas, or dog memes at amorris@gannett.com and follow her on Twitter @amandamomorris for the latest bioscience updates. Independent coverage of bioscience in Arizona is supported by a grant from the Flinn Foundation. -
 2021-04-05
2021-04-05Greenlee County (AZ) Health Department's Daily COVID-19 Updates through April 5, 2021
The Greenlee County Health Department uses its Facebook page to disseminate daily information related to the COVID-19 pandemic to its residents. The daily COVID-19 statistics are displayed as an image on the daily Facebook post, which allows examination of the department's content and messaging before and after the pandemic. Governor Doug Ducey declared a state of emergency in Arizona on March 11, 2020, which seems inconsistent with GCHD's daily posts from that period. Language on the GCHD posts consistently advised residents to stay home if they felt ill, rather than being consistent with Governor Ducey's voluntary Stay Home orders. For example, the March 30, 2021, press release to update a new active COVID-19 infection in Greenlee County reads as follows: "For Immediate Release, Tuesday, March 30, 2021, Greenlee County, Arizona. Public Information Contact: Steve Rutherford (928) 865-2601 NEW RELEASE - COVID-19 Positive Test in Greenlee County The Greenlee County Health Department is investigating one (1) new confirmed case of COVID-19. The case will put our current total at five hundred and sixty-nine (569) confirmed Greenlee County COVID-19 cases... We would like to remind the community to use masks appropriately when outside of the home, practice social distancing, wash your hands frequently, and do not go into the public when you are feeling sick, unless you are seeking medical attention." These updates demonstrate a significant dichotomy between the rural and urban experiences during this pandemic. -
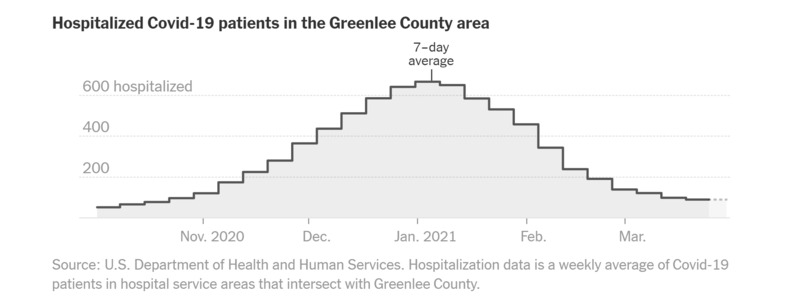 2021-03-30
2021-03-30A Tale of Two Arizonas: COVID-19 Data from Maricopa and Greenlee Counties Through March 30, 2021
This daily tracker displayed on the New York Times site displays and explains public data provided by the Arizona Department of Health Services. The attached graphs illustrate the disparate COVID-19 experience between Arizona residents in Maricopa County and Greenlee County. Arizona is the sixth largest of the United States with a population of more than seven million residents within its 113,594.08 square miles. 61% of Arizonans reside in Maricopa County, which translates to a population density of approximately 481.3 people per square mile, or 57,959.3 square feet per resident. In contrast, southeastern Arizona’s Greenlee County claims only 0.14% of the state’s residents for a population density of 5.7, or approximately 4.8M square feet per person. -
 2021-03-31
2021-03-31News Article: Douglas rescinds requirement for face coverings in public
This news story relays a decision by municipal leadership in Douglas, Arizona, to rescind their mask mandates following Governor Ducey's similar order on 25-March-2021. -
 2021-03-30
2021-03-30News Article: Pima County keeps mask mandate in defiance of Gov. Ducey
This article from the Associated Press relays the arguments Pima County officials have made in keeping mask mandates in place despite recent orders from Governor Doug Ducey on 25-March-2021 that prohibit new mask requirements and phase out current restrictions previously issued by local governments across Arizona. -
 2021-03-25
2021-03-25News Article: Gov. Ducey relaxes COVID-19 guidelines in Arizona; bars can open, cities cannot require masks
This news article from Laura Lollman of 3TV/CBS5 in Phoenix, Arizona, relays updated COVID-19 guidelines that Gov. Doug Ducey signed into place on March 25, 2021. These included a statewide phase-out of municipal and county mask mandates and prohibitions on new mask mandates; businesses may continue to require patrons and employees to use masks or face coverings; gatherings of more than 50 people no longer require permission from local governments; bars may fully open and choose to require patrons and employees to wear masks and social distance -
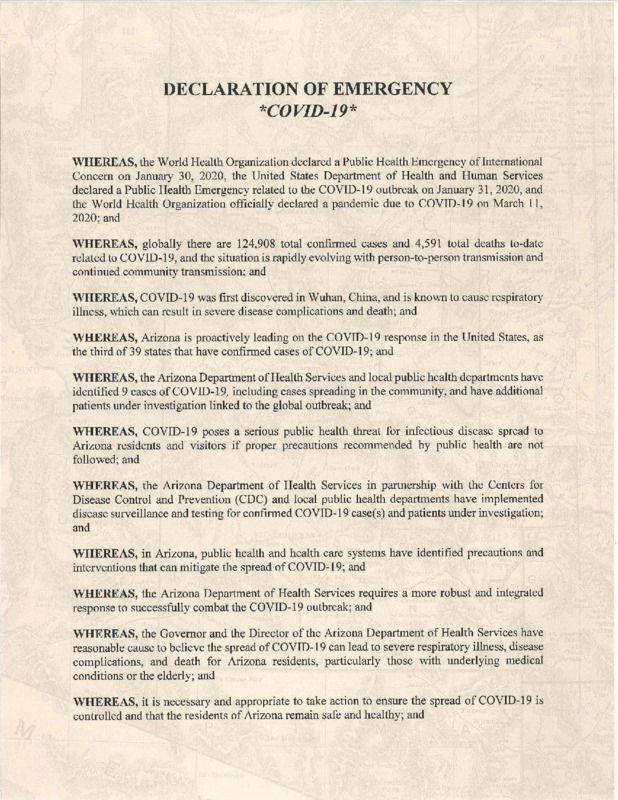 2020-03-11
2020-03-11March 11, 2020: Arizona Declaration of Emergency by Gov Doug Ducey
Declaration of Emergency - COVID-19 WHEREAS, the World Health Organization declared a Public Health Emergency of International Concern on January 30, 2020, the United States Department of Health and Human Services declared a Public Health Emergency related to the COVID-19 outbreak on January 31, 2020, and the World Health Organization officially declared a pandemic due to COVID-19 on March 11, 2020; and WHEREAS, globally there are 124,908 total confirmed cases and 4,591 total deaths to-date related to COVID-19, and the situation is rapidly evolving with person-to-person transmission and continued community transmission; and WHEREAS, COVID-19 was first discovered in Wuhan, China, and is known to cause respiratory illness, which can result in severe disease complications and death; and WHEREAS, Arizona is proactively leading on the COVID-19 response in the United States, as the third of 39 states that have confirmed cases of COVID-19; and WHEREAS, the Arizona Department of Health Services and local public health departments have identified 9 cases of CO VID-19, including cases spreading in the community, and have additional patients under investigation linked to the global outbreak; and WHEREAS, COVID-19 poses a serious public health threat for infectious disease spread to Arizona residents and visitors if proper precautions recommended by public health are not followed; and WHEREAS, the Arizona Department of Health Services in partnership with the Centers for Disease Control and Prevention (CDC) and local public health departments have implemented disease surveillance and testing for confirmed COVID-19 case(s) and patients under investigation; and WHEREAS, in Arizona, public health and health care systems have identified precautions and interventions that can mitigate the spread of COVID-19; and WHEREAS, the Arizona Department of Health Services requires a more robust and integrated response to successfully combat the COVID-19 outbreak; and WHEREAS, the Governor and the Director of the Arizona Department of Health Services have reasonable cause to believe the spread of COVID-19 can lead to severe respiratory illness, disease complications, and death for Arizona residents, particularly those with underlying medical conditions or the elderly; and WHEREAS, it is necessary and appropriate to take action to ensure the spread of COVID-19 is controlled and that the residents of Arizona remain safe and healthy; and WHEREAS, the Governor is authorized to declare an emergency pursuant to A.R.S. § 26-303(D) and in accordance with A.R.S. § 26-301(15). WHEREAS, pursuant to A.R.S. § 26-307(A), a state agency, when designated by the Governor, may make, amend and rescind orders, rules and regulations necessary for emergency functions; WHEREAS, pursuant to A.R.S. § 36-787(A), during a state of emergency declared by the Governor as a result of an occurrence or imminent threat of illness or health condition caused by an epidemic that poses a substantial risk of a significant number of human fatalities or incidents of permanent or long-term disability, the Arizona Department of Health Services shall coordinate all matters pertaining to the public health emergency response of the State; and WHEREAS, pursuant to A.R.S. § 36-787(B) and (C), during a state of emergency declared by the Governor, the Governor, in consultation with the Director of the Arizona Department of Health Services, may issue orders pertaining to the public health emergency response of the State; and WHEREAS, pursuant A.R.S. § § 36-788 and 36-789, during a state of emergency declared by the Governor, the Arizona Department of Health Services, to protect the public health, may establish and maintain places of isolation and quarantine and require the isolation or quarantine of any person who has contracted or been exposed to a highly contagious and fatal disease; WHEREAS, the Legislature has authorized the expenditure of funds in an event of an emergency pursuant to A.R.S. § 35-192; and WHEREAS, Executive Order 2017-06 establishes the Arizona Emergency Response and Recovery Plan to assist in responding to emergencies including public health emergencies; and NOW, THEREFORE I, Douglas A. Ducey, Governor of the State of Arizona, by virtue of the authority vested in me by the Constitution and Laws of the State, do hereby determine that the COVID-19 outbreak presents conditions in Arizona, which are or are likely to be beyond the control of the services, personnel, equipment, and facilities of any single county, city or town, and which require the combined efforts of the State and the political subdivision, and thus justifies a declaration of a State of Emergency; accordingly, pursuant to A.R.S. §§ 26-303(0) and 36-787, I do hereby: a. Declare that a State of Emergency exists in Arizona due to the COVID-19 outbreak, effective March 11, 2020; and b. Direct that the State of Arizona Emergency Response and Recovery Plan be used, and the Division of Emergency Management to be engaged, as necessary or requested, to assist the Arizona Department of Health Services' coordination of the public health emergency response and authorize the use of state assets as necessary; and c. Authorize the Director of the Arizona Department of Health Services to coordinate all matters pertaining to the public health emergency response of the State in accordance with A.R.S. Title 36, Chapter 6, Article 9; This Emergency Declaration will be eligible for termination upon the resolution of the outbreak as determined by the Arizona Department of Health Services. IN WITNESS WHEREOF, I have hereunto set my hand and caused to be affixed the Great Seal. of the State of Arizona. ATTEST: GOVERNOR (Douglas Ducey) DONE at the Capitol in Phoenix on this 11th day of March in the Year Two Thousand Twenty and of the Independence of the United States of America the Year Two Hundred and Forty-Fourth. ATTEST: Secretary of State (Katie Hobbs) -
 2021-02-15
2021-02-15One of my COVID-19 Case Investigations Experiences
I work as a COVID-19 medical investigator for the Arizona county in which I live. I recently called on a monolingual Spanish speaker who turned out to be a retirement-age mother of adult children and infant grandchildren. The first time we spoke, she very politely agreed to complete our medical interview by phone, and I began working through the initial demographics section. As she answered my questions, she began asking questions of her own regarding her potential experience and that of her family, all of whom were ill by that time or presumed to be positive due to extended close contact. The pace and tone of her speech evolved as her volume increased, and her intense emotional distress required no common language to comprehend. The primary source of her concern was her adult daughter who lived at another location with her two children. Our case feared her daughter had to have immediate help to even dial a phone, much less to care for herself and her children. The case wanted to break isolation at her home to travel to her daughter' home to aid her child and grandchildren, but, with the interpreter's help, we worked through her fears, established an action plan that allowed the case and her husband to stay home, and connected her daughter with medcal professionals to evaluate her circumstances and need for urgent intervention. The case and I agreed those needs superseded the interview as she was both aware and isolated, and we agreed to speak the following day. On callback, her emotions had completely turned around in that day, her daughter had been evaluated over the phone, acquired the information and guidance she needed, and the case believed her child and grandchildren were now safe and well. Throughout the roughly 90-minute translated interview, she repeatedly expressed her gratitude for our having called and helped her family and information and guidance. Despite the number of times our patients/cases have expressed anger, outrage, suspicion, or worse at our medical investigation and contact tracing efforts, this series of calls made them worthwhile. -
 2020-04-22
2020-04-22Understanding the Corona Virus Through the Lens of Racial and Social Justice
The Institute for Research on Race and Public Policy and the Social Justice Initiative host a conversation on the Coronavirus Pandemic through the Lens of Racial and Social Justice. Moderated by Barbara Ransby from the Social Justice Initiative, panelists include Dr. Linda Rae Murray, Aislinn Pulley from Chicago Torture Project, Ald. Rossana Rodriguez, Ald. Jeanette Taylor, Detention Watch Network's Gaby Viera and Reyna Wences from Organized Communities Against Deportations. This program was edited by CAN TV -
 2020
2020The Systemic Implications of Asthma During Covid-19
Coping with pandemic anxiety as an asthmatic residing in the Bronx. -
 2020-06-09
2020-06-09Why Social Justice Is Central to Treating COVID-19
From article: Racism and classism create conditions where people of color, those living in poverty, and other marginalized groups have limited access to resources that affect health -
 2021-02-15
2021-02-15COVID-19: We're doing this for this
Video created by the Government of Canada urging the public to wear a mask so "one day we can go back to" travelling, getting together with friends and family, and eating at restaurants. -
 2020-03-27
2020-03-27Social Distancing and Quarantine Were Used in Medieval Times to Fight the Black Death
A medieval Italian legislation document, dating from 1377, reveals that social distancing and quarantine measures were practiced during the bubonic plague. The article describes what measures seaport towns took to screen and isolate ships before their goods and crews could enter these populations Also, it discusses the advent of plague hospitals, how the word quarantine came to be, and 14th century public health structure. As far as medicine and technology has advanced over the centuries, we are still using some of the same practices that were used seven centuries ago. It illustrates how much we can still learn from the past. -
 2020-12-14
2020-12-14Public Health Systems Tension with the Government during COVID-19 Pandemic
Public Health Systems Tension with the Government during COVID-19 Pandemic -
 12/07/2020
12/07/2020Opposition questions Yukon vaccine plan, after learning territory left out of 1st batch
The first batch of COVID vaccine of nearly 250,000 doses will be available before the end of the year, but none will go to the territories. The North lacks the freezers required to store the Pfizer vaccine, which the company says requires a freezer at –80 C to –60 C or in a thermal container at –90 C to –60 C. -
 06/02/2020
06/02/2020Canada's Nunavut: A vast territory with few people - and no coronavirus
Nunavut remains the only state-level jurisdiction in North America not to record a single case of the virus that has sickened millions and killed more than 375,000 people worldwide. Every other Canadian province and territory and every U.S. and Mexican state has reported at least a few. -
 12/08/2020
12/08/2020Northwest Territories (N.W.T) public health emergency extended for 19th time
N.W.T. Health and Social Services Minister Julie Green extends the territory-wide public health emergency until Dec. 22 on the advice of the Chief Public Health Officer. -
 12/10/2020
12/10/2020Moderna vaccine to be available to 75% of 'eligible population' in N.W.T in early 2021
The Northwest Territories government expects the Moderna vaccine for COVID-19 to be available to 75 per cent of the territory's "eligible population" in "early 2021," according to a media advisory issued Thursday afternoon. -
 2020-12-13
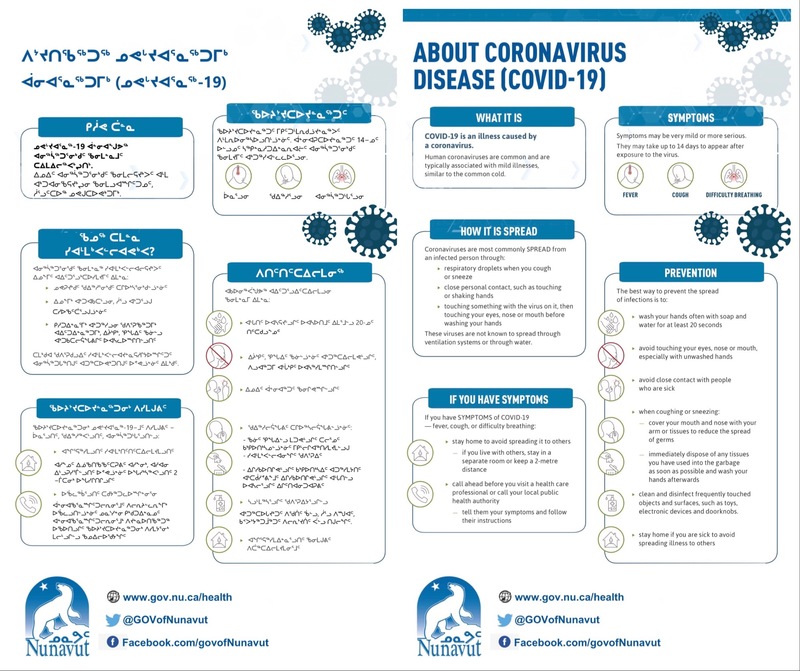
2020-12-13About Coronavirus Disease (COVID-19)
Infographic created by the Government of Nunavut to inform citizens on what COVID-19 is, symptoms, and prevention. Written in English and Inuktitut. -
 2020-11-19
2020-11-19How Nunavut's COVID-19 outbreak is highlighting long-standing health inequities in Canada's North
Chief Public Health Officer Dr. Michael Patterson said in a press conference on Wednesday that Nunavut is reaching its limit in terms of what it can handle. Three contact-tracing teams are racing to reach out to people in the four communities which have cases of the virus: Arviat, Rankin Inlet, Whale Cove and Sanikiluaq.
