Items
Tag is exactly
COVID-19
-
 2020-06-12
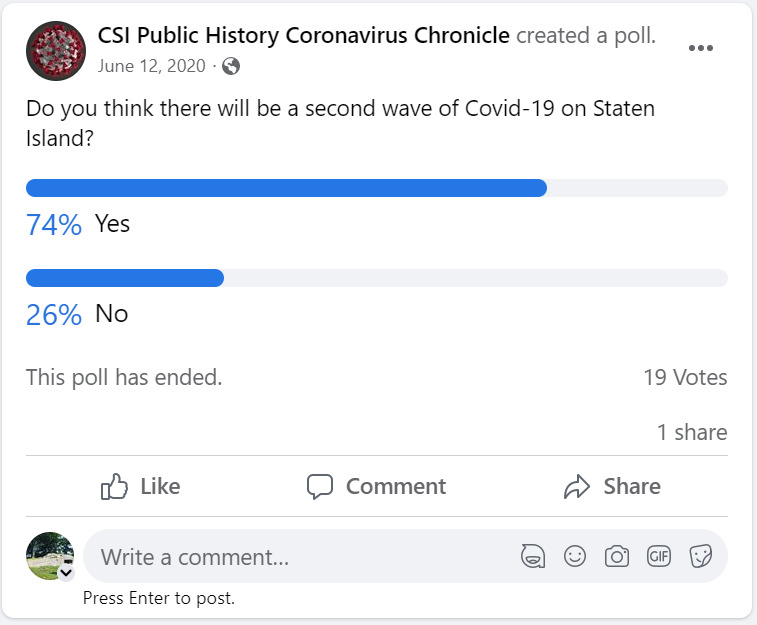
2020-06-12Do you Think there Will be a Second Wave of Covid-19 on Staten Island
Do you think there will be a second wave of Covid-19 on Staten Island? -
2022-11-21
Why?
At the beginning of the Covid-19 Pandemic, my dad was (and still is) a skeptic. He would always ask, "Why do some people get Covid, and others don't? How does the virus choose it's victims?" As the Pandemic continued to grow and spread, my step-mother and I got Covid at the same time. My dad took care of both of us, yet he still did not get Covid. We all survived. Then, the vaccine shots came out, and my dad said, "Hey, I never got it. Why should I take something, when I never got it in the first place?" He did not get the vaccine, while the rest of the family did. Then, my step-mother and I got Covid for a second time. We survived again. Dad said, "I never got the vaccine, and I never got Covid. You guys get the vaccine, and you have it twice. I don't understand at all." To this day, Dad still has not gotten Covid and still refuses to get the vaccines. -
 2022-07-24
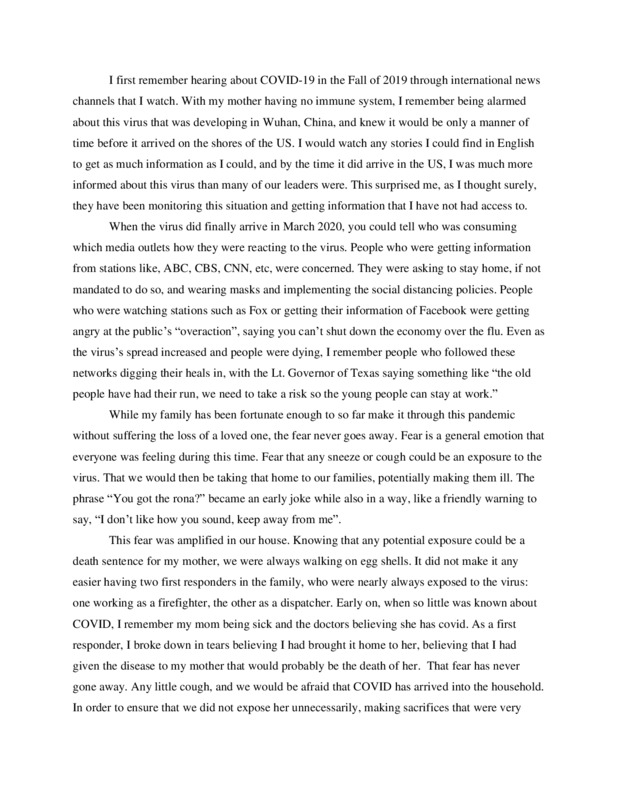
2022-07-24Fear for My Mother's Saefty
I've written a short story centered around my experience with fear of this virus, particularly focusing on how my fear is heighten with an immuno-compromised mother. I wrote about how the media the people around me consumed affected their behavior and played a role within my fear and the impact it had on my mother. This story says two things about this pandemic I think: it shows the impact that information had/has on how people approach the virus and the emotional toll the pandemic had on people living their daily lives. What I've submitted is important because it validates what Americans have experienced. Many Americans -
 2021-12-20
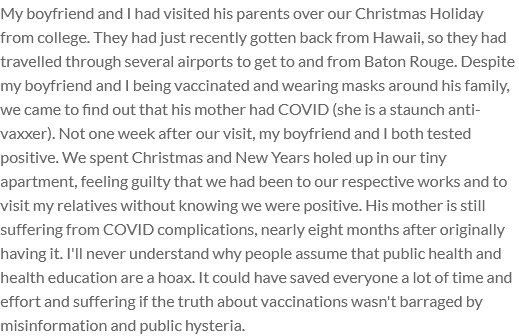
2021-12-20And a Happy New Year
My boyfriend and I had visited his parents over our Christmas Holiday from college. They had just recently gotten back from Hawaii, so they had travelled through several airports to get to and from Baton Rouge. Despite my boyfriend and I being vaccinated and wearing masks around his family, we came to find out that his mother had COVID (she is a staunch anti-vaxxer). Not one week after our visit, my boyfriend and I both tested positive. We spent Christmas and New Years holed up in our tiny apartment, feeling guilty that we had been to our respective works and to visit my relatives without knowing we were positive. His mother is still suffering from COVID complications, nearly eight months after originally having it. I'll never understand why people assume that public health and health education are a hoax. It could have saved everyone a lot of time and effort and suffering if the truth about vaccinations wasn't barraged by misinformation and public hysteria. -
 2022-06-10
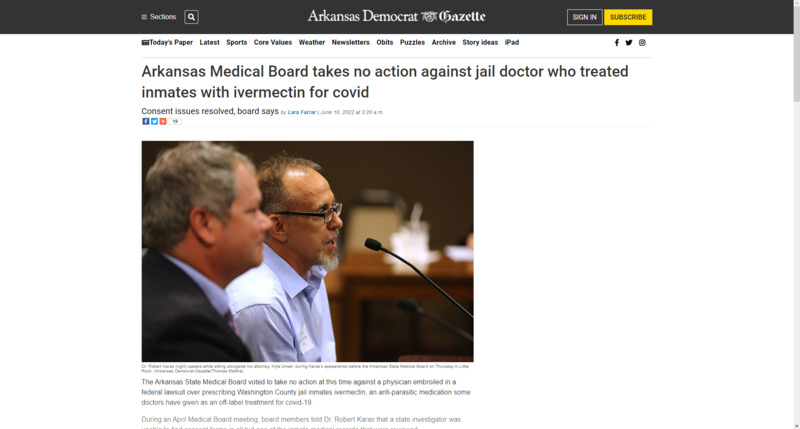
2022-06-10Arkansas prison doctors and ivermectin
This is a story detailing Arkansas' Medical Board dismissing charges against a Washington County prison doctor for treating prisoners with ivermectin. Arkansas' Medical Board has not explicitly denounced the drug as a treatment for COVID-19, and many physicians prescribe the drug. This particular physician treated several unknowing prisoners with ivermectin in order to combat rising covid cases in the Washington County Jail in April. This dismissal of charges by the Medical Board reveals a deeper skepticism of the pandemic in Arkansas and a willingness of the board to allow physicians to treat their patients as they ultimately see fit with minimal regulations. I feel it also reveals a deeper understanding of Arkansas' prison system due to the prisoners not being informed of what was given to them, and therefore without consent. -
 2022-07-09
2022-07-09Hospitalizations on the rise in Arkansas
This is an article detailing a surge in COVID related hospitalizations in Arkansas. The article further mentions an increase in deaths due to COVID-19 and how hospitals are quickly beginning to feel the pressure of overcrowding. The July 4th holiday, doubtless, had an impact. This surge demonstrates not only the minimal precautions taken by individuals as life has seemingly returned to a sense of normalcy, but also demonstrates that many Arkansans are still unvaccinated, and the extreme toll such action is taking on hospitals. -
 2022-07-11
2022-07-11COVID Cases Once Again On the Rise in Arkansas
This article details a recent surge in Arkansas COVID cases. The shocking nature of the rise is the fact that the state's active cases jumped from 197 to 15,125 in a single day. I think this primarily demonstrates the state and the world's rush to reopen, particularly keeping in mind the July 4th holiday, have allowed a sense of deep comfort. However, this comfort can be deadly when individuals who are feeling unwell fail to take precautions to assure the health and safety of themselves and others. While it is encouraging to see life return to a sense of normalcy, this shows that the pandemic is still a present part of our lives. -
 2022-07-11
2022-07-11LGBTQ+ VA Healthcare in Arkansas in the wake of COVID
This is the Arkansas Veterans Affairs website listing specific resources for LGBTQ+ veterans in Arkansas. This site places a specific emphasis on Central Arkansas due to the heavy LGBTQ+ population in that area. In order to combat COVID-19, this site focuses on not only concerted vaccine rollout for LGBTQ+ vets, but also lists mental health resources in order to combat COVID-19. I think this shows a particular vulnerability to a select group and how COVID-19 can reach anyone. Indeed, it is essential that at-risk groups such as the LGBTQ+ community are not overlooked in the age of COVID, and it is encouraging to see the VA take steps to assure this is the case. -
 2022-07-10
2022-07-10Tennis Is Done With Covid-19, but the Virus Isn’t Done With Tennis
This is a news story from The New York Times by Matthew Futterman. This story chronicles the changes tennis has gone through during the pandemic. Compared to other professional sports, tennis has been one of the sports with restrictions applied the longest Novak Djokovic, one of the top tennis players in the world, is noted for his refusal of the COVID vaccine. This caused controversy in 2021 at the Australia Open, where his refusal to get vaccinated resulted in his deportation. The Australian government was worried that his refusal would embolden others. The rest of the article goes on about what other tennis players have said about the restrictions, and what they mean for the sport. Some of the tennis players expressed not paying attention to restrictions as much as they used to, and wanting to live like they used to. -
 2022-07-08
2022-07-08Covid was the US leading cause of deaths for 45 to 54 year-olds in 2021
This is a news story from Quartz by Annalisa Merelli. This news story says that within the deaths that occurred between March 2020 and October 2021, the middle-aged were disproportionately affected. In the 45 to 54 age group, COVID killed more than any other leading causes of death within that time period, including heard disease and cancer. -
 2022-07-08
2022-07-08NYC officials recommend masks indoors due to COVID surge
This is a news story from Axios by Herb Scribner. Due to a rise in COVID cases, health officials in New York City are recommending that people wear high quality face masks indoors or in crowded areas. A CBS News report says that COVID positivity rates have risen 14%, the highest level since January. A subvariant of Omnicron, BA.5, has been responsible for 54% of total COVID cases, according to the CDC. -
 2022-04
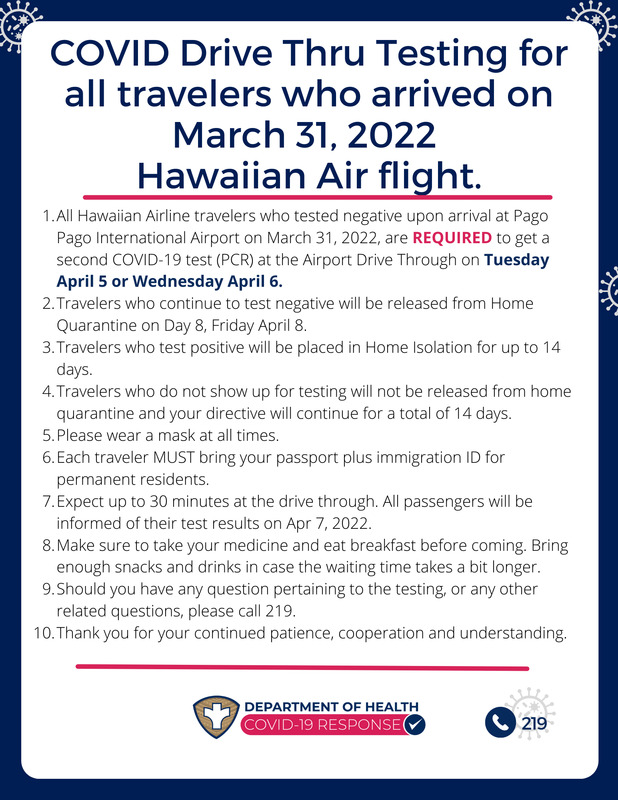
2022-04Drive Thru Test for travelers in American Samoa
Opening up the borders in American Samoa was great news for Samoans that were stuck in the states for a year and a half borders were closed in American Samoa. And just when they think going home would be easy, it wasn't. There were a lot of requirements that were set by the government for travelers to follow when entering the island. This was one of the many requirements that travelers had to follow to ensure the safety of the people of American Samoa. Even if your test came negative upon arrival, you still had to get a second test to make sure that you do not have COVID. Somehow, despite these requirements, restrictions, and quarantine, cases still emerged on the island. -
 2022-06-25
2022-06-25Learn how the government works
This is a tweet by StabbyandSpicy. This person is expressing their frustrations over their mom getting COVID, and the Supreme Court decision on Roe v. Wade being overturned. -
 2022-06-25
2022-06-25Everyone can get long COVID
This is a tweet from myrabatchelder. This person is advising other about the risks of long COVID, saying people should wear masks in indoor and crowded settings. -
 2022-06-25
2022-06-25My body, my choice...except with experimental vaccines
This is a tweet from geraldcelente. This person is expressing their anger towards Dr. Fauci and his ideas on what "my body, my choice" actually consists of. Within the vaccine skeptic communities, people like Dr. Fauci are held in contempt due to his stances on things like masks, vaccines, and lockdowns. -
 2022-06-25
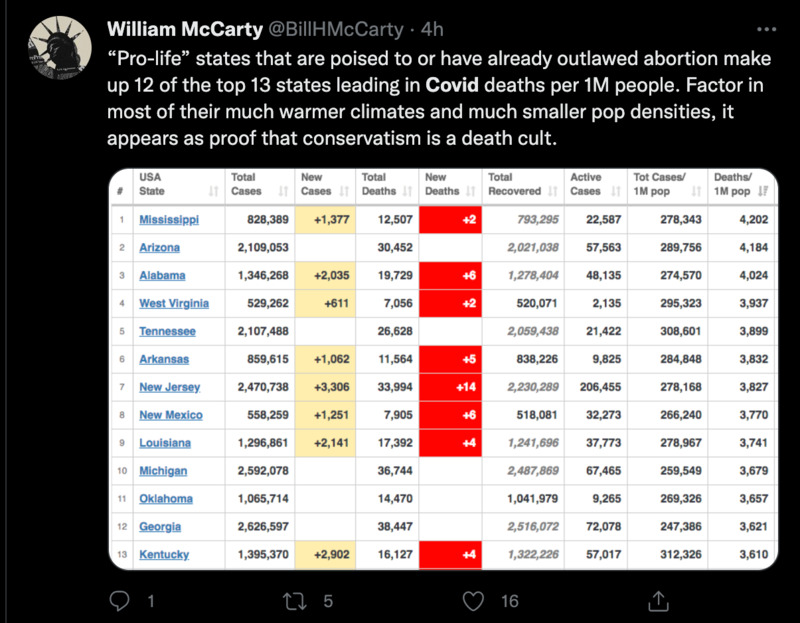
2022-06-25"Pro-life" and COVID death
This is a tweet from BillHMcCarty. This person is criticizing the amount of COVID deaths that are happening is states that are looking to outlaw or heavily restrict abortion. -
 2022-06-16
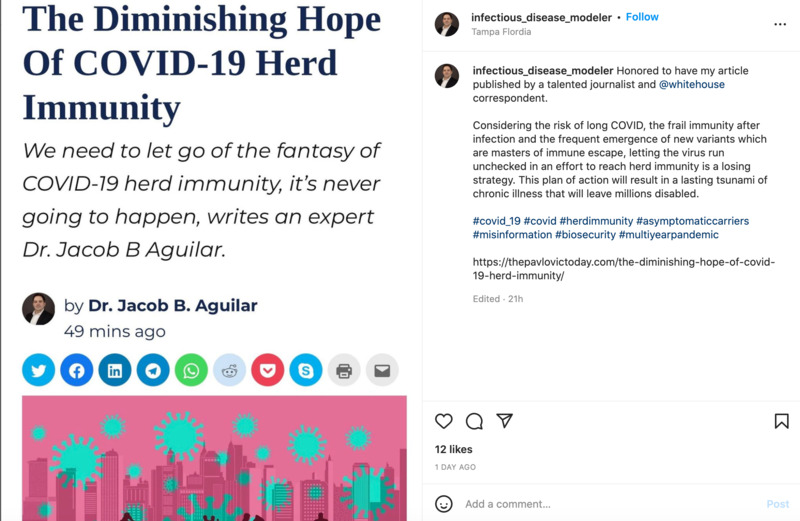
2022-06-16The Diminishing Hope of COVID-19 Herd Immunity
This is an Instagram post from infectious_disease_modeler (Dr. Jacob B. Aguilar).He wrote an article about how herd immunity doesn't work with COVID as well as it could due to new variants that keep on happening. He says that if vaccines had a 100% effectiveness rates across all situations, this would not really be an issue. Since the vaccines are not entirely effective, the solution, Dr. Aguilar proposes that the way to help mitigate the issue is mass regular testing to slow the spread of new variants. -
 2022-06-11
2022-06-11Do we have to go out again?
I am an anxious person. Before covid it took all my energy to get up in the morning, put on decent clothes, go to school, meet with friends, go to restaurants. The lockdown was the best thing that ever happened to me. My best buddy moved in with me and my family, my classes went online, I slept more, I gamed all the time, we got takeout. Now I'm being invited places. I have to reinsert. I miss covid. -
 2020-08-06
2020-08-06Knock Knock
During the summer of 2020 I was taken from my current unit (where I work as a nurse) back to the ICU to care for the overflowing patients. The ICU is a very noisy place, but one noise that was new was the knocking. To go into a COVID patient's room you have to put on booties, a full length gown, two pairs of gloves, an N95 mask and a surgical mask along with eye protection. It is a lengthy process so once you are in the room you don't leave until all tasks are complete. So if you need something when you’re in there you would knock on the glass doors of the patient's room and one of the helper nurses would come and read what you had written on the door in a marker and get the items for you. It was so quite in the rooms, no families were allowed so it was you, the machines and the patient. It was so hot you could feel the sweat dripping down your back and pooling in the arms of your gown. It was a very isolating feeling, usually there are lots of hands and people in your rooms with you to help or just to chat but not during COVID. The knock-knock could be heard all down the hall. It reminds me of the isolation we all experienced during this time and also how resilient we are and how helpful nurses are to each other. Nursing is a team sport. It is a sound and an experience I will never forget. -
 2000-05-16
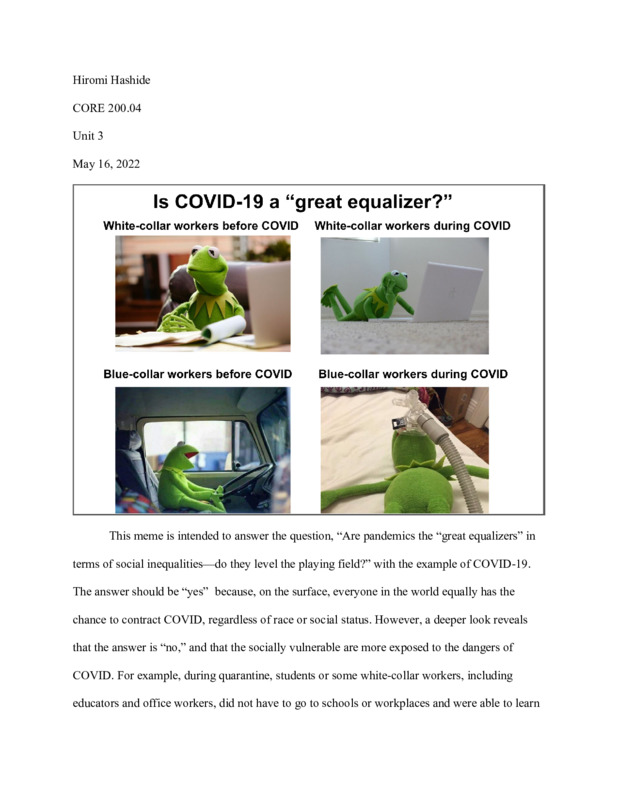
2000-05-16Is COVID-19 a "Great Equalizer?"
I made two memes. The first meme is intended to answer the question, “Are pandemics the “great equalizers” in terms of social inequalities—do they level the playing field?” with the example of COVID-19. And the meme says the answer is “no,” and that the socially vulnerable are more exposed to the dangers of COVID. The second meme is intended to answer the question, “Have you observed any patterns of human behavior with the Covid-19 pandemic?” Former President Trump called COVID the “China Virus” and fueled people’s hatred of Asians. This meme tries to remind the audience of his negative remarks but in a humorous way without offending Asian populations. It also illustrates how words can magnify feelings of racism, fear, and uncertainty, which can result in scapegoating. This meme gives the audience an opportunity to learn more about the unfair treatment of Asians during the pandemic and why it happened. -
 2022-03-09
2022-03-09The Pfizer Documents
This is a video regarding the safety of the Covid-19 Phizer vaccine reports that were recently released as of the making of both the video and this submission. It details the adverse events, the safe deliveries of the vaccine amongst an assortment of disorders, and the unhappiness of both the video creator and the viewers in the comments at the lack of transparency regarding the information surrounding the vaccine. -
 2022-05-13
2022-05-13Taking a Rapid Covid-19 Test In Public
In this phase of my life, I have more loose ends than tied down ones. I often have to arrive at places early or multitask my use of a space or transit system. During a moving process, this is exaggerated. I have so much schoolwork and shifts at my job that often I just roam the city between events. I was notified that I had been around someone with Covid, so I grabbed a test at Walgreens. When I got back onto the street, I realized that most people would be shocked or disgusted at seeing someone test themselves for the plague in a public space. I felt like I could not go to my student center as they might tell me I could not take a Covid test there, and I could not go home as I was already downtown and had class in a few hours. I decided to go to a place where many people are dealing with their own issues publicly; the downtown public library. I knew I could take this test there and not be bothered. I entered, took a few escalators, and found a secluded desk where I was able to take the test. It felt as if I were doing something wrong, or illegal. I do not think that should be the way it is, but we tend to shun the sick and demand people to leave if they are not using a space the "correct" way. I tested negative. -
 May 24, 2021
May 24, 2021Chronicles of the Plague Years
[From the Introduction] For the students, faculty, and staff at Bronx Community College, March 2020 was a sucker punch to the gut. Our vibrant campus, a beautiful haven filled with vitality and life, became a kind of petri dish—ground zero for the COVID 19 virus to make landfall. Not only were many students and staff sickened in those early days, but the City University system was forced to close, then transition to remote learning in the space of a single week. It was a challenge, to say the least: for faculty who needed to quickly learn the tools to make it possible, and even more so for the students, who—cut off from socialization and in person learning—had to adjust to this new reality. Stranded in their homes, some students were forced to continue working frontline jobs, while others lost jobs and income, facing financial devastation. Students were confronted with their own illness as well as that of family members. Online learning was fraught in those early days. As a community, we improvised our way forward, without the proper technology and knowhow to do it. But two years on, our students have proven their resilience. In time, we adapted to remote learning, to new ways of doing things, of coping. 2020 was harder, and in 2021, the challenges continued. But, somehow, we got through. These student books provide a glimpse into the minds of the talented BCC Digital Design students who persevered, strived, and thrived. -
 2020-11-30
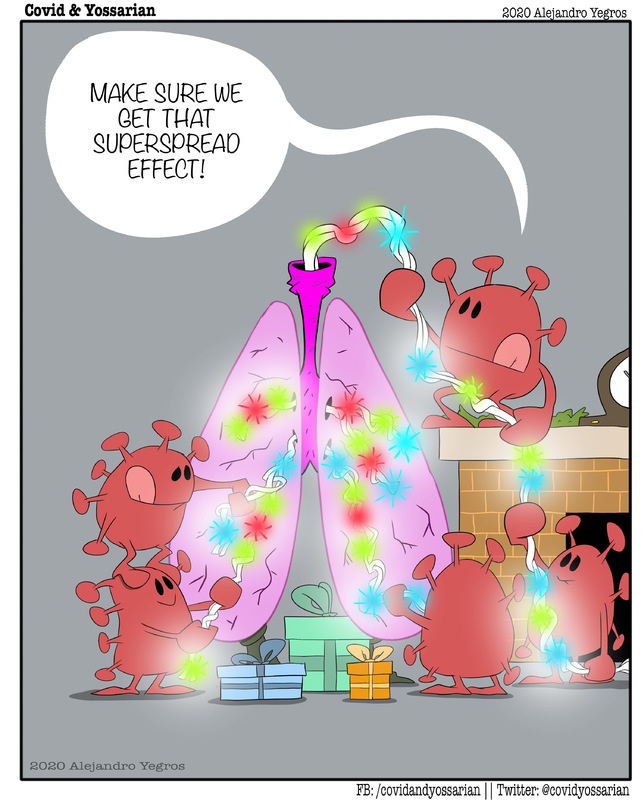
2020-11-30Tree decorations
A comic strip about Covid-19 -
 2020-10-13
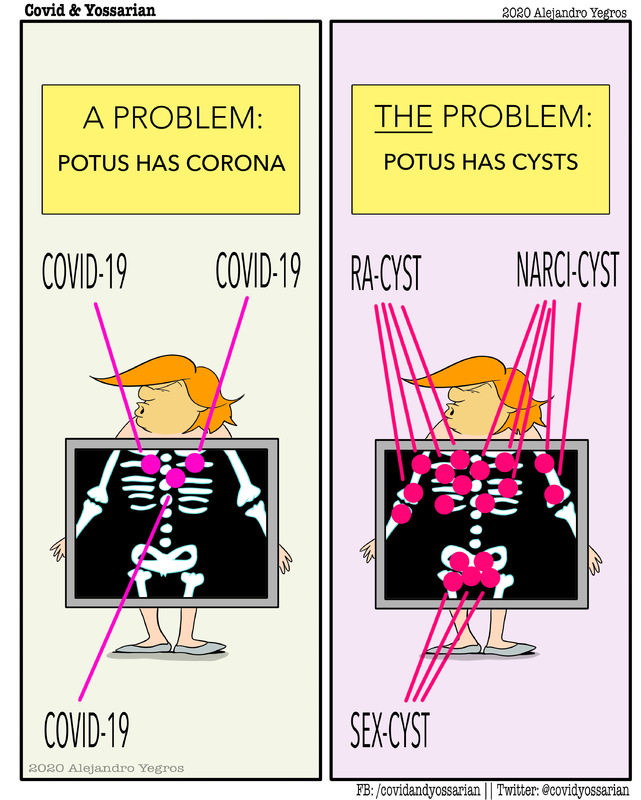
2020-10-13Cysts
A comic strip about Covid-19 -
 2020-10-10
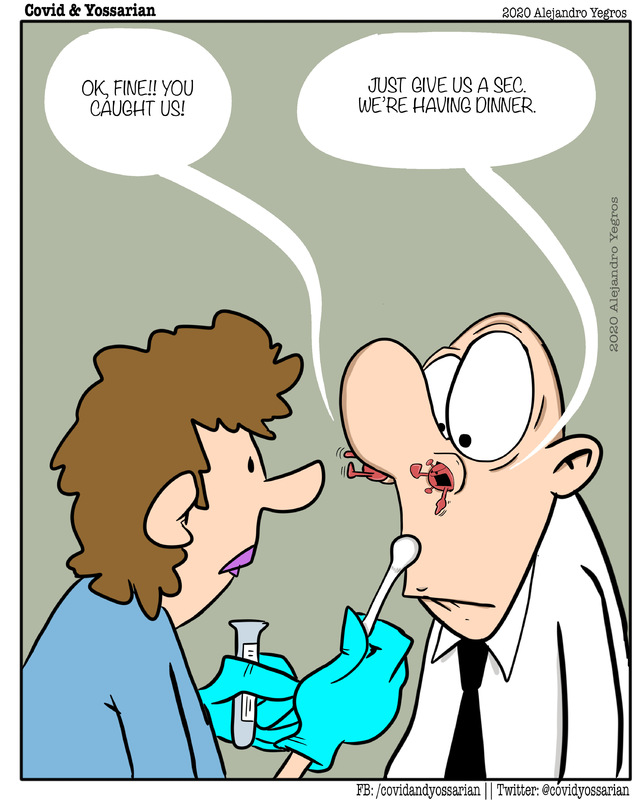
2020-10-10Just give us a minute
A comic strip about Covid-19 -
 2020-10-04
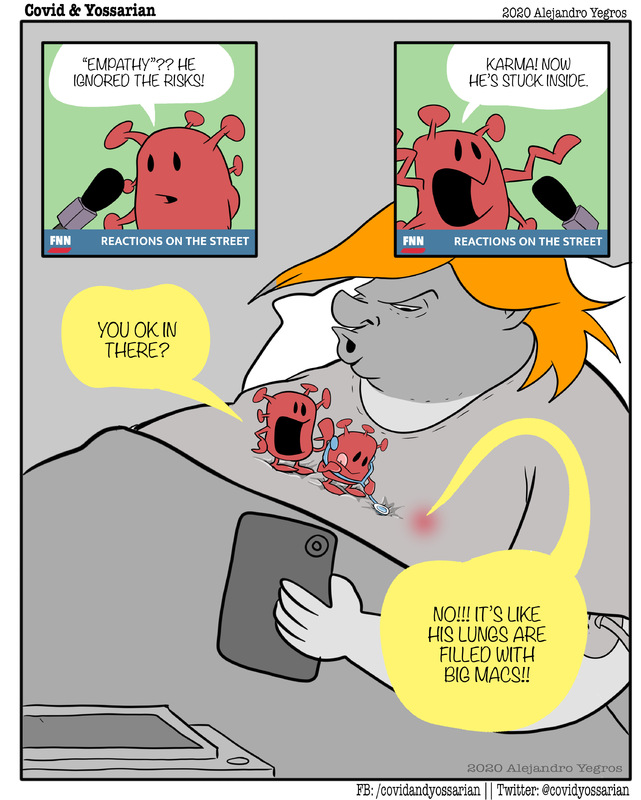
2020-10-04Ignored the risks
A comic strip about Covid-19 -
 2020-07-21
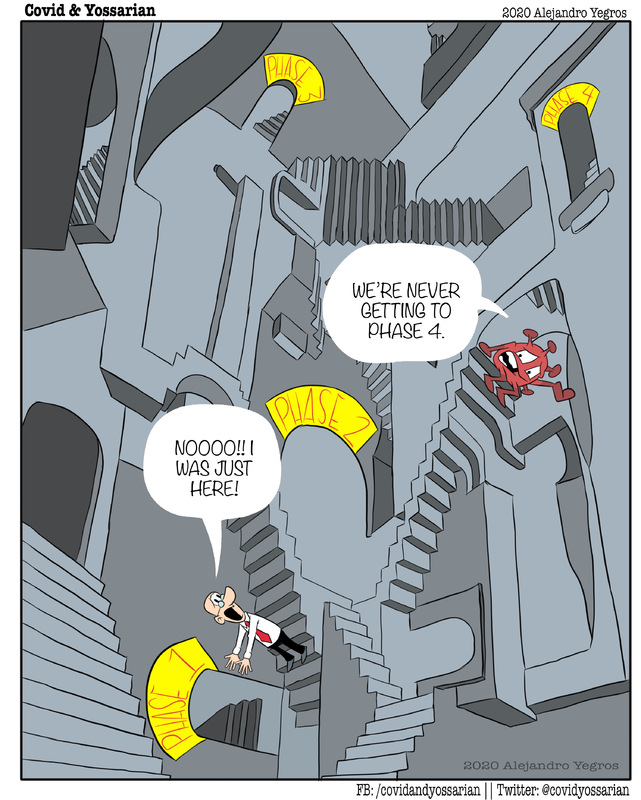
2020-07-21Infinite loops to phase 4
A comic strip about Covid-19 -
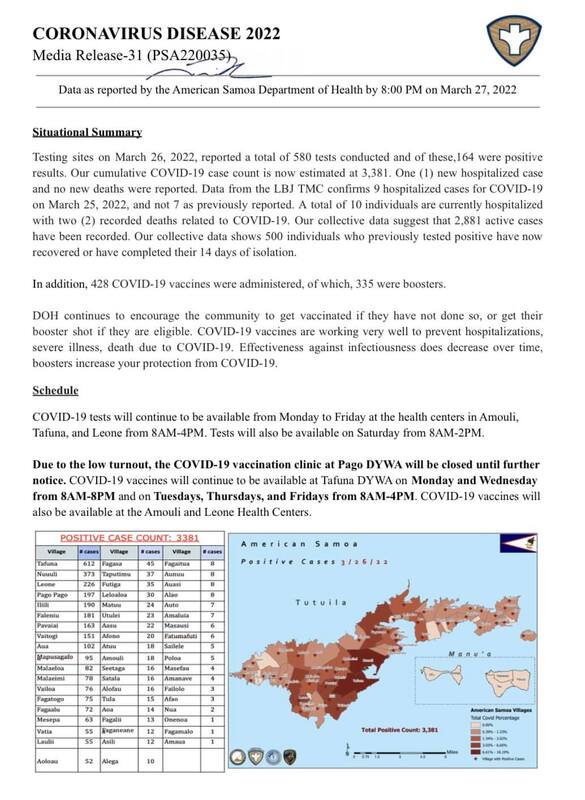 2022-03-27
2022-03-27American Samoa COVID Cases Situational Report #18
This is the eighteenth report released by the American Samoa Department of Public Health regarding the rise of covid cases in American Samoa. As of March 27, 2022, positive cases have risen to 3381 from 2953 on March 25, 2022. -
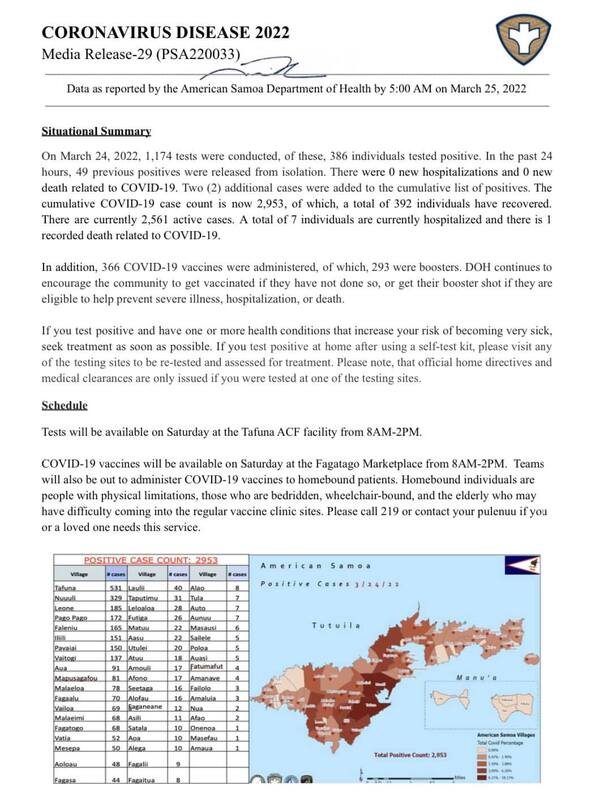 2022-03-25
2022-03-25American Samoa COVID Cases Situational Report #17
This is the seventeenth report released by the American Samoa Department of Public Health regarding the rise of covid cases in American Samoa. As of March 25, 2022, positive cases have risen to 2953 from 1932 on March 22, 2022. On this report, a number of 7 individuals are hospitalized to covid and there is 1 death related to COVID-19. -
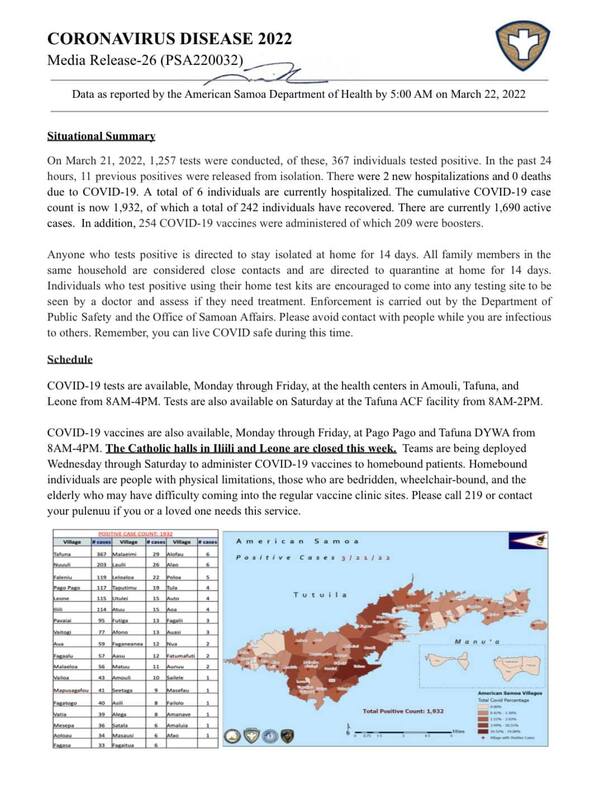 2022-03-22
2022-03-22American Samoa COVID Cases Situational Report #16
This is the sixteenth report released by the American Samoa Department of Public Health regarding the rise of covid cases in American Samoa. As of March 22, 2022, positive cases have risen to 1932 from 1565 on March 21, 2022. -
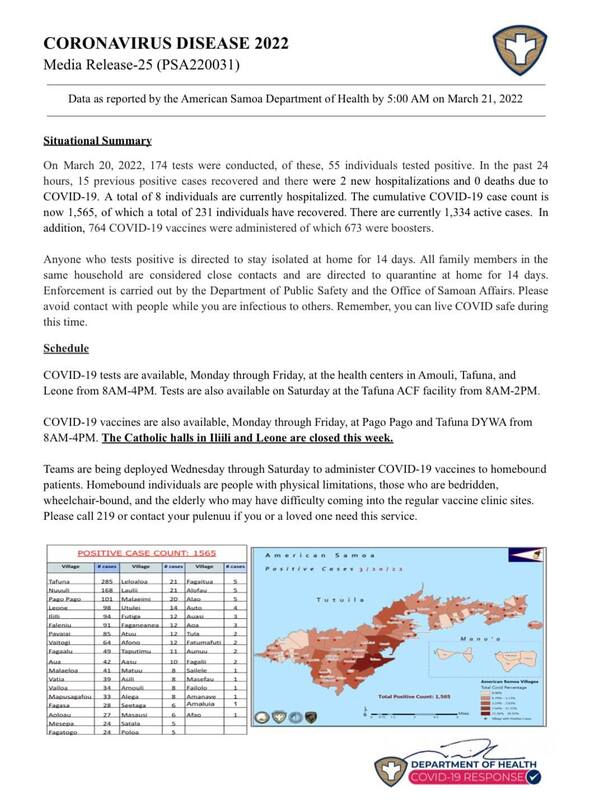 2022-03-21
2022-03-21American Samoa COVID Cases Situational Report #15
This is the fifteenth report released by the American Samoa Department of Public Health regarding the rise of covid cases in American Samoa. As of March 21, 2022, positive cases have risen to 1565 from 1188 on March 17, 2022. -
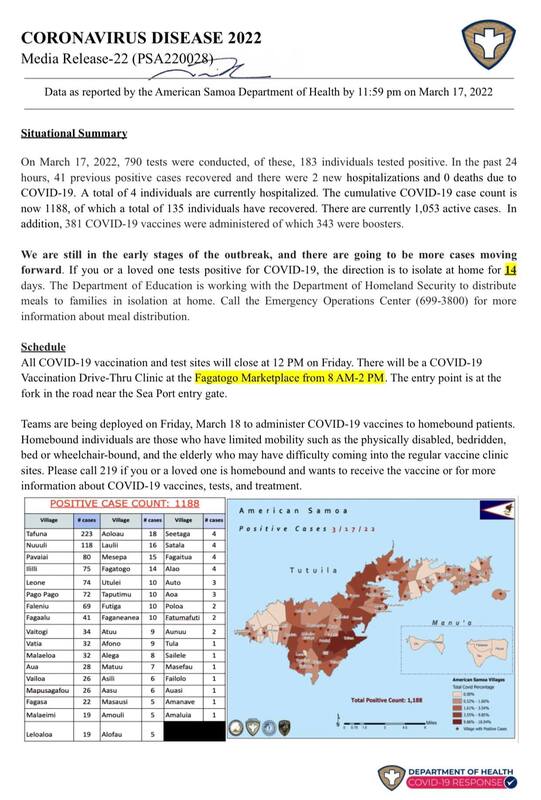 2022-03-17
2022-03-17American Samoa COVID Cases Situational Report #14
This is the fourteenth report released by the American Samoa Department of Public Health regarding the rise of covid cases in American Samoa. As of March 17, 2022, positive cases have risen to 1188 from 433 on March 10, 2022. -
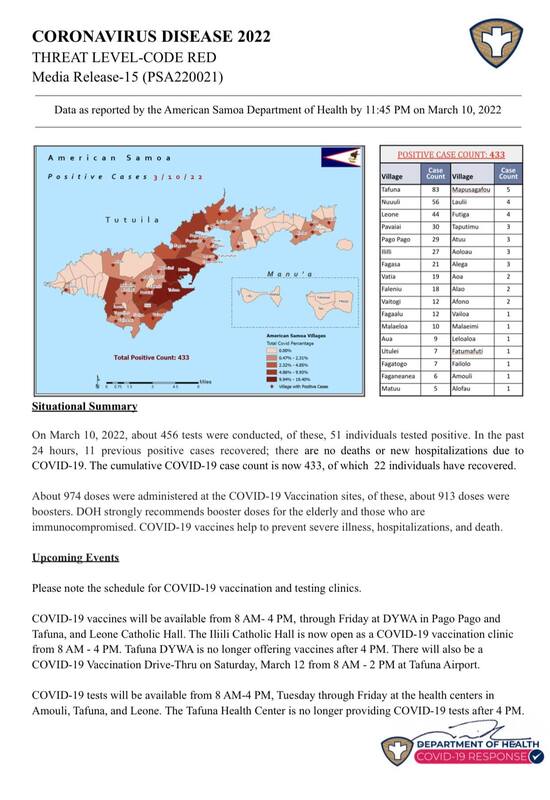 2022-03-10
2022-03-10American Samoa COVID Cases Situational Report #13
This is the thirteenth report released by the American Samoa Department of Public Health regarding the rise of covid cases in American Samoa. As of March 10, 2022, positive cases have risen to 433 from 343 on March 9, 2022. The DOH advised that elders are strongly recommended to get the booster shot. -
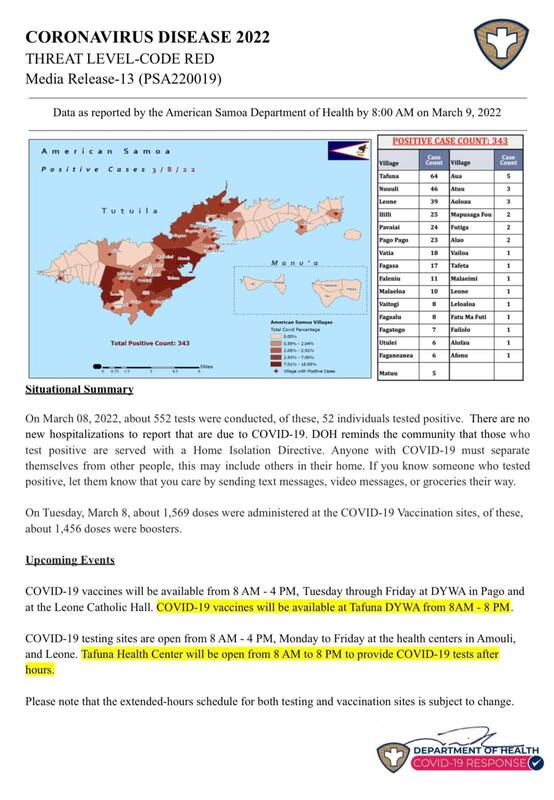 2022-03-09
2022-03-09American Samoa COVID Cases Situational Report #12
This is the twelfth report released by the American Samoa Department of Public Health regarding the rise of covid cases in American Samoa. As of March 9, 2022, positive cases have risen to 343 from 291 on March 7, 2022. The people of American Samoa are still advised to get their vaccine shots and booster shot. The numbers jumped by 52 cases after two days. The report also shows how many doses of vaccine and booster were administered. -
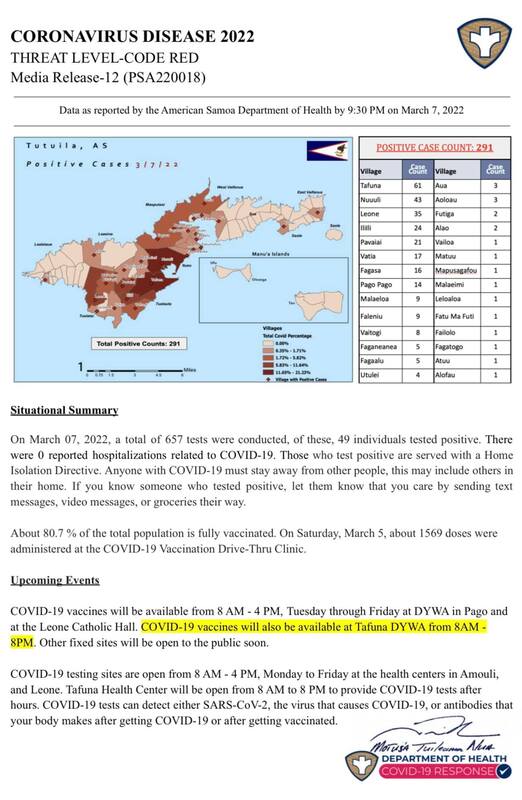 2022-03-07
2022-03-07American Samoa COVID Cases Situational Report #11
This is the eleventh report released by the American Samoa Department of Public Health regarding the rise of covid cases in American Samoa. As of March 7, 2022, positive cases have risen to 291 from 243 on March 6, 2022. The people of American Samoa are still advised to get their vaccine shots and booster shot. It is also heartwarming that within these reports that are released to the public, the DOH encourages people to send text messages, video messages, or groceries to someone who tested positive. -
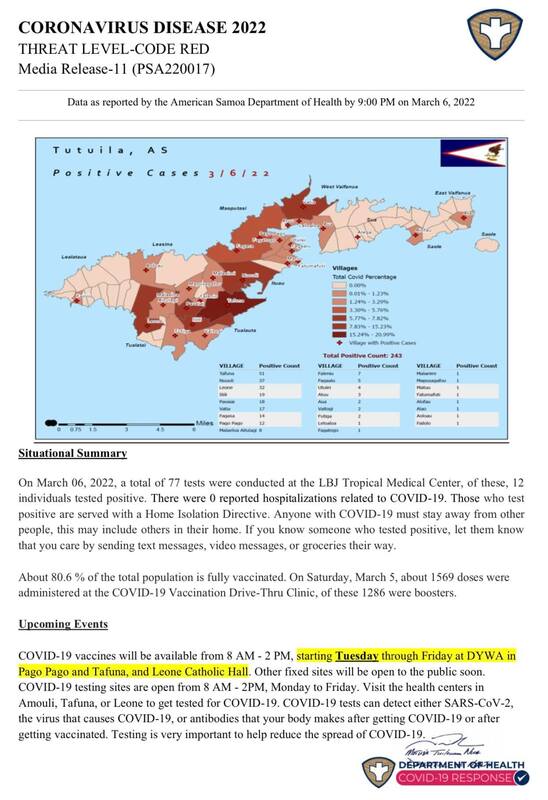 2022-03-06
2022-03-06American Samoa COVID Cases Situational Report #10
This is the tenth report released by the American Samoa Department of Public Health regarding the rise of covid cases in American Samoa. As of March 6, 2022, positive cases have risen to 243 from 229 on March 5, 2022. The people of American Samoa are still advised to get their vaccine shots and booster shot. And if they are to get tested, there are clinics on the East and West of the island to get tested if people are positive. The DOH released these reports daily or weekly to inform the public about the number of cases on the island. -
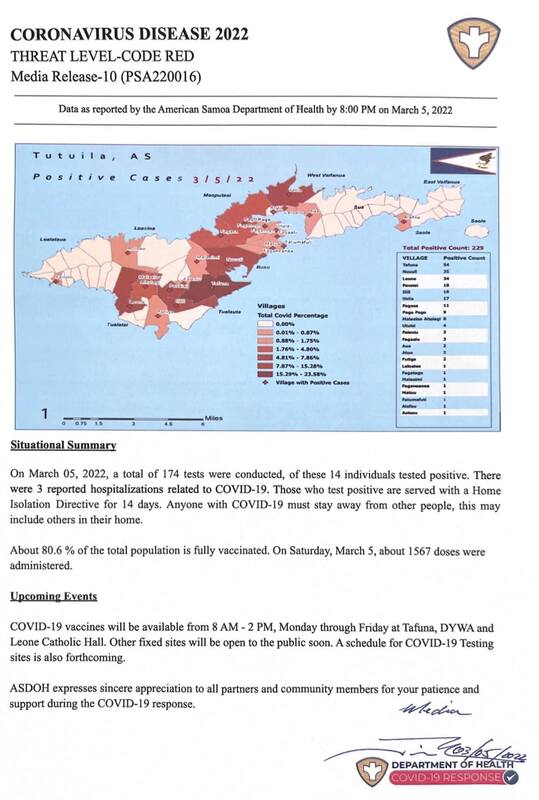 2022-03-05
2022-03-05American Samoa COVID Cases Situational Report #9
This is the ninth report released by the American Samoa Department of Public Health in regards to the rise of covid cases in American Samoa. As of March 5, 2022, positive cases have risen to 229 from 215 on March 4, 2022. -
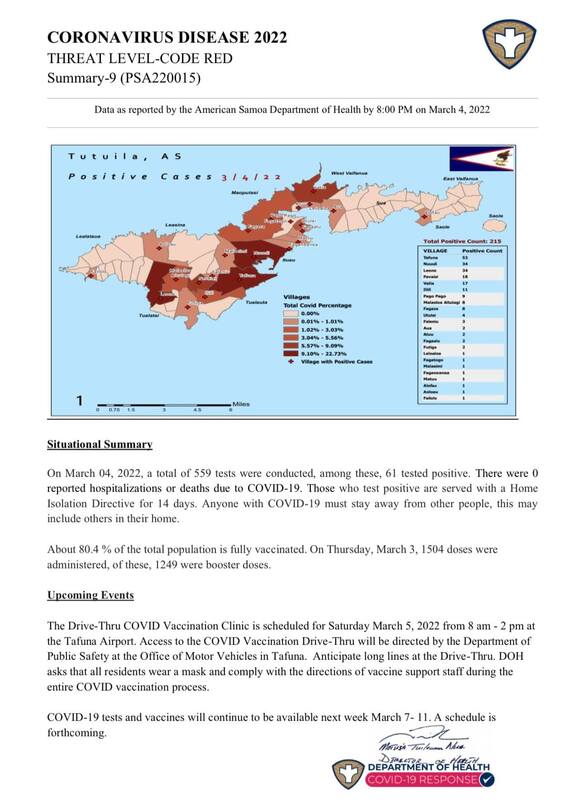 2022-03-04
2022-03-04American Samoa COVID Cases Situational Report #8
This is the eighth report released by the American Samoa Department of Public Health in regards to the rise of covid cases in American Samoa. As of March 4, 2022, positive cases have risen to 215 from 154 on March 3, 2022. The DOH also changed the look of the Situational Report to show the map of American Samoa and color-coded villages with their number of cases. -
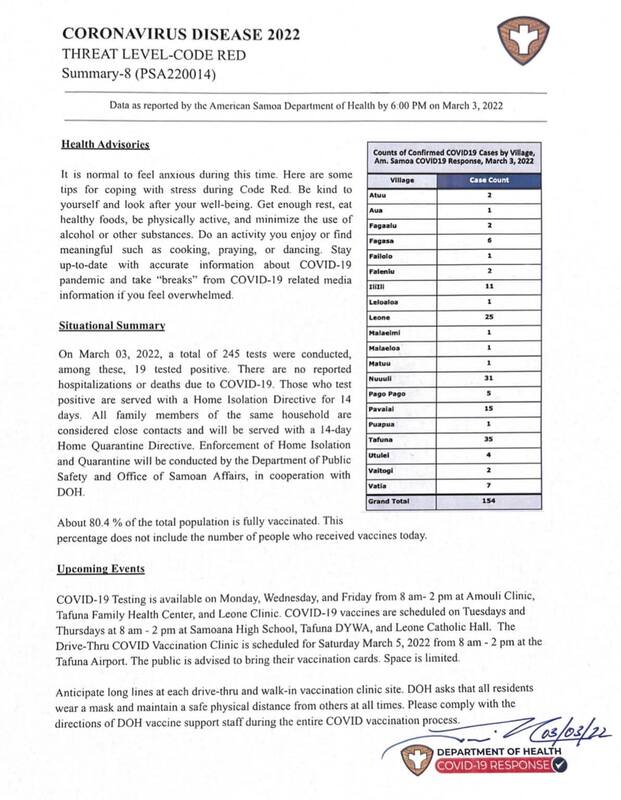 2022-03-03
2022-03-03American Samoa COVID Cases Situational Report #7
This is the seventh report released by the American Samoa Department of Public Health in regards to the rise of covid cases in American Samoa. As of March 3, 2022, positive cases have risen to 154 from 135 on March 2, 2022. -
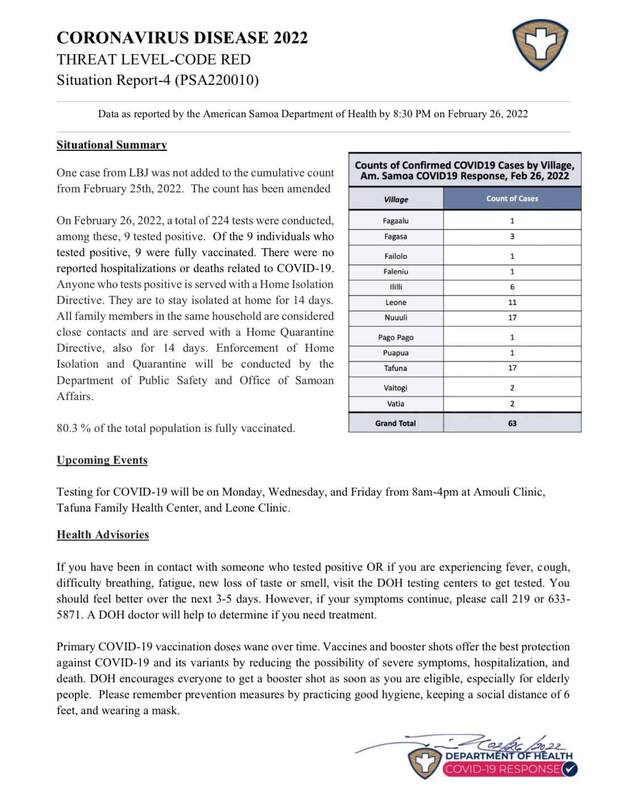 2022-02-25
2022-02-25American Samoa COVID Cases Situational Report #3
This is the third report on the COVID cases in American Samoa. The public is informed to get their vaccination and booster shots and to practice good hygiene social distance and wear masks. The number of cases is now 63. -
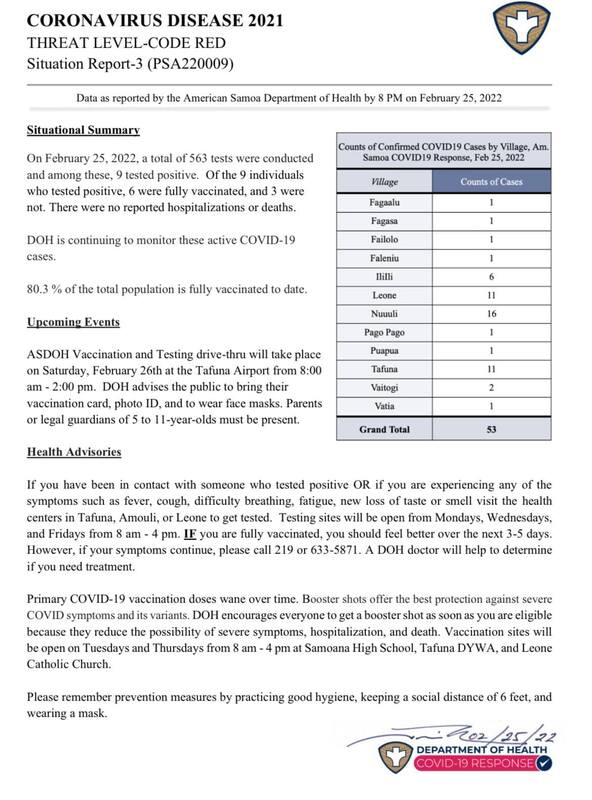 2022-02-25
2022-02-25American Samoa COVID Cases Situational Report #2
This is the second report from the American Samoa Department of Public Health in regards to reporting the number of cases in American Samoa. After a day, the number of cases jumped from 22 to 53. -
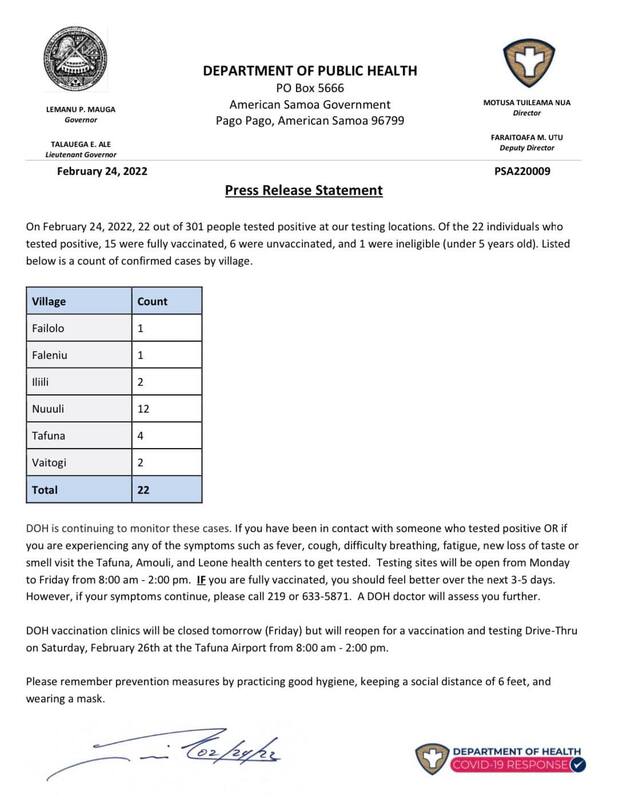 2022-02-24
2022-02-24American Samoa COVID Cases Situational Report #1
This is a report from the American Samoa Department of Public Health in regards to reporting the number of cases American Samoa has with COVID reaching the island. Ever since cases began to rise on the island, the American Samoa Department of Public Health has been releasing these situational reports on COVID cases publicly and weekly. The importance of these reports was to keep the public inform and we could see just how fast the disease spread in a significantly high amount weekly or even in a couple of days. -
 2022-04-12
2022-04-12Vacuna contra COVID19
This is an Instagram post by eldiariodetlaxcala. This is written in Spanish and is about information for people to get the AstraZeneca vaccine. This event will be held for two days. In the picture, we see volunteers working to help administer the vaccine. Only people 18 and above are eligible for this vaccine, and it is being held in Ocotlán, Tlaxcala. -
 2021-01-05
2021-01-05The Covid Pandemic as a Senior in Highschool
The website that I am linking describes what happened to students all over the world in March of 2020 when all students in schools and universities had to go on lockdown and switch abruptly to complete online learning. This is an important covid-19 related topic to me because I was a senior in high school during that time, and I really struggled with my mental health, academic achievements, responsibilities, body image, and just overall my whole life. This article isn't as personal as it could get, but it gives a good historical and general idea of what student experience during the pandemic was like. -
 2022-04-10
2022-04-10My Expirence with Covid-19
I had Covid twice and my symptoms both times were just cold like symptoms. -
 2022-04-09
2022-04-09Covid sped up my great grandmothers death
My great grandmother was diagnosed with dementia and was living in a nursing home for a few years, she started to get worse when the pandemic started so but we weren't able to visit her due to covid-19. She began to become very depressed due to the lack of visits and her son (my grandfather) had been diagnosed with stage 4 lung cancer in June and was given up to 6 months to live. My grand father died on October 19th of 2020, my great grandmother caught covid while in her nursing home and on November 20th 2020 my great grandmother died from covid-19. Even though she was dying of dementia, covid sped up the process and caused her to die alone in a nursing home. I couldn't even burry her like she would have wanted because the nursing home had her cremated for contamination purposes. I would give anything to be able to hold her hand as she passed and give her a proper funeral that she would have wanted but covid compromised this. -
 2022-03-26
2022-03-26Coping with the Pandemic--A Personal Look at Mental Health and COVID-19
According to the Center of Disease Control, in June of 2022, US adults reported considerably elevated adverse mental health conditions associated with COVID-19. Out of a survey they did on 5,412 people, 40.9 percent of respondents reported at least one adverse mental or behavioral health conditions, including symptoms of anxiety and depressive disorder which were around 31 percent. One of the causes of this is due to increase sedentary behaviors and low levels of physical activity due to quarantines and lack of business operation. Over the past two years, government mandated quarantine, work from home, and online schooling has caused me to stay at home for longer periods of time than what I use to. Because of this sedentary behavior, I had dealt with the negative effects of isolation, stress, and anxiety on both my mental and physical health. According to the World Health Organization, 150 minutes of moderate exercise or physical activity is usually recommended per week, however, with working a full-time job and being in school, the question that remains is how that is possible? I have learned to accommodate these physical needs indoors, by taking active breaks during the day and exercising at home. While this does not necessarily help with isolation and loneliness sometimes, I have learned to take these matters one day at a time and not shun myself for feelings them. CDC argues that from a recent comprehensive review that the impact of COVID-19 on mental health particularly seems to affect more young women disproportionally than any other group. Therefore, I recommend any young adult or women facing severe mental health to take advantage of online support or mental health services through telehealth such as ZocDoc. It is important to highlight COVID-19's impact on mental health in the United States and my personal life because it shows how the pandemic changed the means and the ways we received mental health services in the past. As the pandemic ventures on, people like myself will continue to have to find ways to cope and receive services for our problems. Thanks to the pandemic, much of our mental health problems have come more to the forefront due to us having ample amounts of time now to navigate and deal these issues unlike never before. -
 2022-03-20
2022-03-20A Day in the Life of a Delivery Driver in the South
I deliver copier toner to various clients across Northwest Arkansas, so I am able to see the various ways COVID-19 has impacted businesses, both large and small. Particularly, I am able to see the various protocols of businesses relating to admission into their facilities. From the time I began delivering in March of 2021 to today, it is interesting to see the adjustments made by the community as cases would fluctuate. It is further interesting to see a southern perspective, as the south has been notorious for having a lackluster approach to the pandemic. I will detail six varying instances of businesses across NWA and how they have changed or not changed from a year ago. 1. Banks were an interesting study. My company supplies three major banks across NWA, and all three had very stringent protocol in March 2021, and as cases have declined, they have removed these protocols entirely. In early 2021, bank lobbies were closed to outside visitors with zero exceptions. In order to make my deliveries, I was required to call the bank and meet a staff member at the front door, and both myself and the staff member were required to wear facemasks and social distance. Now, in 2022, these protocols have vanished entirely. Bank lobbies are now open entirely, and masks and social distancing are a thing of the past. This directly correlates with a dramatic fall in COVID cases and deaths, as well as a rise in vaccinations across Arkansas. 2. Chicken plants and food processing plants are an essential part of the economy of Northwest Arkansas, being the home of Tyson, George's, and Cobb-Vantress foods, as well as many others. The protocol for processing plants were stringent in 2021, and they continue to be so in 2022. It is standard practice to not only wear masks and social distance, but also to take temperatures and answer a health questionnaire by security guards. The only change I have seen is a vaccination requirement. Nobody is allowed on the premises of many of these chicken plants without having had both dosses of the COVID-19 vaccine, and vaccination proof must be available whenever requested. Food safety is essential in preserving the health of workers and the community at large, so it is no surprise that these stricter protocols have remained in place. 3. Schools are similar to banks in that COVID protocols greatly shifted from 2021 to 2022. Many schools in 2021 had masks mandates for both students and staff and encouraged social distancing. Now, in 2022, masks and social distancing are no longer required, and school is entirely like it was pre-pandemic. Student's are free to wear masks if they so choose, but any protocol has vanished. This is particularly prevalent in smaller school districts. Depending on the district, many smaller ones had zero protocols to begin with, so things haven't changed in that sense. 4. Manufacturing plants are common in NWA, and many of them have maintained pandemic protocols in 2022. Temperature checks, masks, and social distancing are the norm. There are even a few plants that require appointments to enter their facilities in order to maintain security and prevent the spread of COVID. This is largely attributed to maintaining the health of the workers and preventing outbreaks in facilities that would limit production capabilities in a time when goods are so scarce. 5. Transportation is another major business in NWA, and interestingly, protocols have been minimal. Many transport companies had no original mask requirement, social distancing requirement, or a temperature check. This attitude has continued in 2022, despite the extensive traveling many truck drivers engage in. There were many concerns in the COVID conscious sectors of the community about the possibility of interstate infection, but no changes to trucking protocol were made. It is further interesting the extensive COVID regulations placed on truckers from other states, compared to states like Arkansas. 6. Hospitals and medical clinics, like many across the nation, have made minimal changes to COVID protocol. Washington Regional Medical Center, Northwest Medical Center, and Mercy Hospital all have bared the brunt of COVID in NWA, and masks, temperature checks, social distancing, and exposure questionnaires are the new norm, and medical administration has been unmoving in their insistence on these protocols. Indeed, medical facilities are the locations in which there is the greatest risk of exposure and many medical clinics are still closed to walk-in visitors. The only change really seen from 2021 to 2022 is the allowance of visitors. Previously, no outside visitors were permitted in the hospitals without special permission. As cases declined and vaccine rates grew, the hospitals lifted this restriction and now visitors are common place. It will be interesting to see when and if some of these protocols will change as the pandemic advances. Indeed, it is also interesting to see how and if protocols become a new essential part to admission to various facilities across NWA beyond the pandemic. -
2020-09-20
Discovering You Have COVID19
It was September of 2020, and I was babysitting at the time. The kids I was babysitting for were sick, but I did not think much of it, babies are sick all the time right? So, I continue going to work throughout the week. I am changing the diaper of the child, and may I add that this is a dirty, poopy diaper. I am thinking in my head, "Wow it is kind of crazy that this does not smell bad, it ALWAYS does." Suddenly it clicks in my head, I cannot smell. I go smell a candle, smells like nothing, an onion, nothing, perfume, nothing, and I am instantly in a panic. I am then wondering if I can taste anything, I try every food in the pantry, again... nothing. I immediately tell the mom I babysit for (she works from home), and she tries smelling her candle, and she smells nothing either. We go together and get tested, and we all had COVID19. We all ended up being okay and quarantine for 10 days, so its okay to laugh at the situation now. That was my most memorable moment of COVID19.
