Items
Tag is exactly
hospital
-
2020-08-10
Saying Goodbye during the pandemic
During the pandemic my grandmother acquired the virus and desperately needed medical attention but the Healthcare system in a third world country such as Peru was saturated. she had to wait outside the hospital in a temporary medical tent. my grandmother passed away two weeks from her diagnosis. many other families experienced the same situation. this story is very important to me in order to spread awareness of what can happen if a country's health system is not equipped with the necessary tools to handle such terrible events like the pandemic. -
 2021-02-17
2021-02-17It took my world
This is a photograph of my best friend, my mother. In December of 2020, we went to Disneyworld and came back with Covid-19. I was barely pregnant at the time, but my Covid symptom was only a cough. This cough would only hurt my uterus, so when I started to miscarry, I wasn’t too surprised. My mom, on the other hand, thought that her muscles were sore from walking around the parks for a few days. She had a cough and a bit of a fever, but was still walking around the house as we quarantined together. She was cold, which only ever happened when she was sick. One day, she didn’t leave her room because she was struggling to catch her breath if she did too much. She had me turn the heater on for her because of how cold she was under her blankets and comforter. She had been keeping her C-PAP machine on to give her the extra air support, but when we checked her oximeter, it was only at 70. So I called the paramedics like she asked me to, they came, we met them at the door, her vitals were taken, and they said that I could take her to the hospital or they could. I told her that I would drive. I had to take her to the emergency room that was not in our normal network because that’s what was open. I took her there with the expectation of getting her transferred the next day. When we called, the other hospital couldn’t take her because all of their beds were filled. So, she stayed there, and I couldn’t be with her because they were trying to keep the spread down. She was texting and FaceTiming me for the first 4 days that she was in the emergency room. On the 5th day though, she stopped responding. I called the hospital and they told me that she had spoken to her doctor and they had decided to put her on the ventilator to give her body a break for a few days. It was not a few days. On day 39 of her being on the ventilator, they lowered her sedation medication and she had no eye movement. So, I told them to let my brother go in and say his second final goodbye and to call me when they had ended her fight the next day. They called and said that she took a few seconds off of the ventilator before they called the time of her passing. I was alone now. My dad passed away in 2006 and my brother was a technical part of my family, but it was just me and my mom in the house still. Now, it was just me. A year later, I lost my home because I couldn’t get a loan approval to buy out my brother’s half of the equity. At that time, I was pregnant again with the baby girl that my mom dreamt of me having. This child that she had planned to be overly involved with, to play with, to snuggle, to kiss, and to have memories and adventures with. But now, the nursery would be someone else’s room. A stranger. Covid-19 took my baby, my mom, my house, my stability, and my will to love. I have been able to love my baby girl, but I am always comparing myself to my mother and thinking about how she could’ve been the best grandma. How she would’ve helped me. How we would’ve traveled to so many places together. And now, I struggle to pay rent on a single room. I leave my child at daycare 5 days a week and try to keep her there for each meal in case I don’t have enough to feed her. And I hide away from a lot of socializing because my mom was my favorite person to hang out with. -
 2020-02-25
2020-02-25Covid journal, 2020-2023
From the beginning, I was aware that this was a world historical event and I wanted to be very attentive to how it played out, both in the news and in my personal life. I read that diaries were scarce in the aftermath of the 1917 pandemic, so it could be useful to scholars to create one this time. I reviewed it before submission, and it reminded me of many things I had already forgotten. Once I started in February 2020, I wrote every day until mid-2021, when entries began to thin out. -
 April 19, 2020
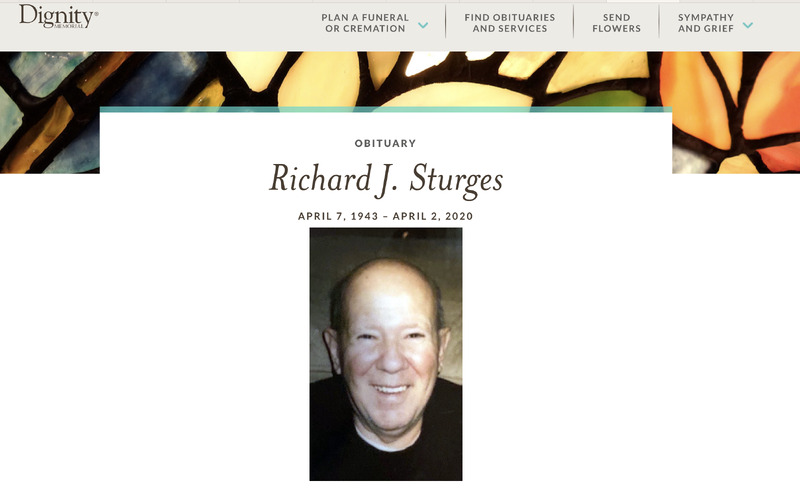
April 19, 2020In Memory of Richard Sturges
My dad passed away a week ago today after contracting COVID-19 in a SI nursing home and transferring to SIUH. When we first learned of my dad’s diagnosis in the nursing home, his doctor prescribed him hydroxychloroquin which he had been using with good results on other patients. However upon trying to fill the prescription learned that the NY Health Dept under order by the Governor, had restricted the use of this drug to hospital patients only. You can imagine our dismay to learn this and our family immediately jumped into action contacting every state legislator about this horrific restriction on the elderly and nursing homes. The two who stepped forward to answer our calls and hear our concerns were Borough President Oddo and State Senator Lanza and they made many calls on our behalf. Before long the restriction on nursing homes was lifted, hopefully before too many lives were lost, but the ban remains on any other New Yorker who tests positive and is not hospitalized. My brother and sister, along with their spouses, have now tested positive. Two of them are first responders and had a lot of difficulty getting tested. I have been staying with and caring for my mom through this time and fortunately we have managed to avoid contracting this virus, so far. My dad was buried 2 days after he died. The Navy showed up to play taps and present my mother with a flag “on behalf of the President and a grateful nation”, my dad would have liked that. The picture is attached and I think says a thousand words. Only my siblings and mother were allowed to attend the burial, a funeral is not allowed at this time. We all wore masks and stood apart from each other and afterwards drove home to our separate houses…truly heartbreaking. The fact that my dad was isolated for weeks before his passing is the hardest thing for my mom to bear. They are lifelong Staten Islanders and this is their story…. Thank you. -
 April 23rd, 2020
April 23rd, 2020Hospital During Lockdown
What Hospitals were like doing during lockdown -
2020-04-08
Impressive experience
When the Covid-19 outbreak first started in New York, it was unfortunate that all of my family was positive. In March 2020, after someone in New York was diagnosed positive, my family did not want me to go out and during that time I was in high school and working part-time. My family including most relatives also started not to work and quarantined at home. One day, one of my aunts came to my house with a cold and a cough, but we didn't think much of it because she just got the flu shot so we figured it might be the aftermath of the shot. After two or three days, we started to have different symptoms. I remember I started with a sore throat, a headache, a fever, and then lost my sense of taste and smell. My relatives also showed different degrees of symptoms, and my grandma had the most severe symptoms. She first had a sore throat, a cold, and a low-grade fever, and then she kept having diarrhea and couldn't eat which caused her to lose almost 10 pounds in just one week. During that time, one of my aunts came to take care of my grandma. Throughout the duration of my grandma being ill my aunt was running on only a few hours of sleep per day since she had to keep an eye over my grandma. I remember that the hospitals in New York were full at that time, many patients died without receiving treatment, and refrigerated trucks were parked outside the hospital to store the dead bodies of patients. The TV news also showed that many people were protesting against the announcement of masks being mandatory when going out. None of them believed that Covid-19 would be serious enough to kill people, and this frustrated me, making me feel the urge to express my feelings towards how serious this virus is. I saw that my grandma's condition was getting worse and worse. We also thought about calling an ambulance to take her to the hospital, but we were afraid that we would not get treatment and we would not be able to visit the hospital. We felt very hopeless. We were on the last straw, thus we were all discussing that if grandma didn't show any signs of improvement the next day, our last resort is to have my grandma sent to the hospital. As a result, the following day, my grandma started to eat and did not continue to have a fever, and her condition began to improve. Overall, Covid-19 has brought my family a lot of distress and I am glad that Covid-19 has started to settle and everything is slowly getting back to normal again. -
 2020-03-19
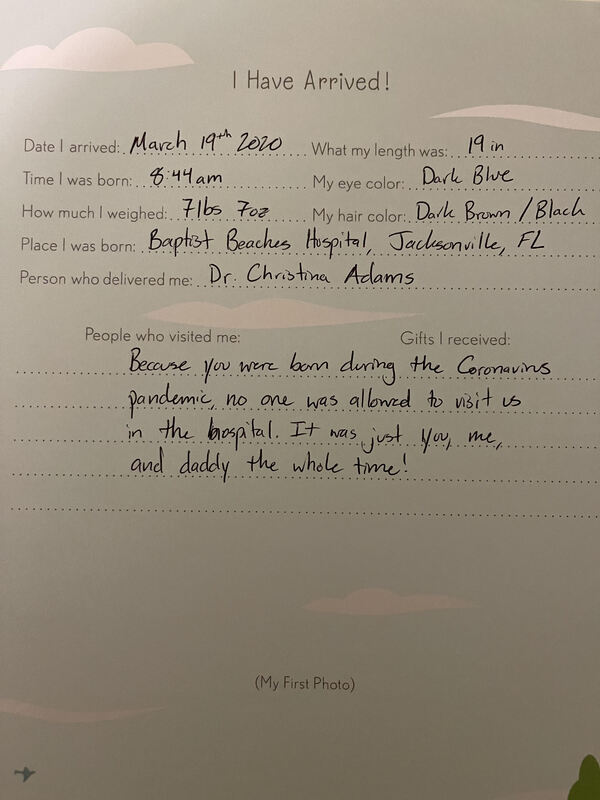
2020-03-19Silent Hospital – Giving Birth in Quarantine
The Covid-19 quarantine started on March 16th, 2020. I gave birth to my daughter four days later. Thankfully my labor was very quick and there were no complications. By 8:44 a.m. on the 19th, my daughter was in my arms. After the commotion of the nurses and doctors coming to check on my daughter and myself, there was just silence. Newborns, as a quickly discovered, slept a lot. There were long stretches of silence for the two days we were in the hospital. I would look at my husband and say, “It is eerily quiet in here.” I was only one of three mothers giving birth in my area of the hospital, there were no visitors, and we were told to stay in our rooms unless we absolutely needed to walk around. My husband would order food and have to wait at the front of the hospital for them to drop it off. Every time he left and came back, he talked about how he had barely seen anyone, and that it was completely silent in the hospital. When it was time for us to finally leave, walking out of the hospital was also silent. There were no phones ringing, no nurse pagers, no talking between nurses, nothing. The only sounds were my flip flops squeaking off of the floors. When we finally made it outside, the birds were chirping and I remembering thinking, ‘thank goodness for some background noise!’ -
 2020-03
2020-03Navigating through medical care during the beginning of the Pandemic
During the beginning of the pandemic, I was taking care of a sick family member who needed multiple surgeries and doctors appointments. The sickness started prior to the pandemic, but continued through the beginning of March 2020. I remember having to wait outside in my car while she was in the hospital getting surgery and not being able to go inside while she was admitted to a room in the hospital. The stress and anxiety I felt was like none other I had felt before. Not only did I feel the stress of not being in that room to be an advocate for my family member, but also the true fear of her contracting COVID19 while having a compromised immune system. During this time, my work offered a six week paid pandemic leave that I utilized to take care of this family member at home. This reduced a lot of stress because I was able to quarantine us while she healed and take care of her. I will always be appreciative of my job for allowing this opportunity. As the world adapted, so did we, but I do have to say the scariest times were navigating the health care systems while everyone was attempting to lower the Covid19 rates. -
 2022-07-09
2022-07-09Hospitalizations on the rise in Arkansas
This is an article detailing a surge in COVID related hospitalizations in Arkansas. The article further mentions an increase in deaths due to COVID-19 and how hospitals are quickly beginning to feel the pressure of overcrowding. The July 4th holiday, doubtless, had an impact. This surge demonstrates not only the minimal precautions taken by individuals as life has seemingly returned to a sense of normalcy, but also demonstrates that many Arkansans are still unvaccinated, and the extreme toll such action is taking on hospitals. -
 2021-08-05
2021-08-05How COVID Affected My Family
COVID took a huge tole on my family. We were unable to have getting togethers for almost a year since my grandparents are older. This was hard for us because we have multiple get togethers in a year. Last August, both of my great grandparents tested positive with COVID. They both have many underlying health conditions that made their fight hard. My great grandma pulled through but my great grandpa did not. This was a very hard loss for my family because his passing was the first in our close family. The worst part about all of it was that they would not let any of us in the hospital to say goodbye. We had his funeral outside so all of my older relatives could attend and stay safe. COVID years were hard for my family and I am very glad we are finally on the other side of it. -
 2021-04-03
2021-04-03The whitewashing of Arab Americans impacted by Covid-19 is a catastrophic public health issue, experts say
This article brings up important points regarding the underrepresentation of Middle Eastern and North African (MENA) people and communities in U.S. This article focuses primarily on Arab Americans, but also sheds light on the fact that there are no identifiers for Middle Eastern and North African people on the U.S. Census as their only options are to choose “white” or “other”. As a result, there is a lack of Covid-19 data specific to these communities which prevents support and information being directed to those underrepresented – and often socioeconomically underprivileged – groups. This article is important in demonstrating the vulnerability of this group. Many MENA families live in multi-generational homes, have preexisting medical conditions or risk factors which may make them more vulnerable should they contract Covid, and still some do not have access to the information and support needed to prevent Covid or to receive the proper treatment if infected. Additionally, because MENA people are not able to self-identify on the U.S. Census, the information about how these communities are being affected is not accurate. The U.S. Census isn’t the only place where these identifiers do not exist. Job, scholarship, and college applications (to name only a few) do not provide accurate identifiers for MENA individuals. I think this article is important in revealing the lack of identifiers available to MENA people and how important it is that this is changed soon. -
 2022-03-31
2022-03-31COVID-19 and pregnancy: More new mothers dying, increasing women's fears during tense time
This is a news story from The Columbus Dispatch by Megan Henry. This story is about the rising fears of new mothers as COVID has increased their chances of dying. In 2020, motherhood mortality rate increased by 20% in the United States. There were also large disparities in who died, with Black women dying three times the rate of White women during pregnancy. Dr. Jason Melillo, an OB-GYN for OhioHealth claims that COVID is the main culprit for the rise in pregnancy related deaths. Pregnant women are more prone to complications from COVID, with things such as blood clots, stillbirth, and preeclampsia happening more often. This concern has made some couples only deciding on pregnancy until they have both been vaccinated. Dr. Melillo hopes that over time, mortality rates associated with pregnant women will go down. -
2022-03-27
Sometimes I forget my aunt died of COVID-19.
Although my aunt was not a significant part of my life since about 2007, she was still family. During the midst of the large outbreak in the summer of 2020 my dad texted me that she was in the hospital, then was released, and then was found deceased in her home a few days later. At this time, it was hard to have a body “processed” quickly, for lack of better words, through morgues and funeral homes. Additionally, having a funeral service was not advised because of either lockdown, funeral homes limiting attendance, or these homes even not performing services. On top of that, many people would have been hesitant to attend. My dad and his siblings decided to not have a service. I have heard many other similar stories. Perhaps this became a pandemic funerary custom to some; life went on and no occasion was marked. Even though we were not super close, and I was not despondent, this would have been a way to process and mark a death for me. For others, a time to process grief. To summarize, she died of COVID-19. I could not visit her in the hospital, and we did not have a funeral service or a burial. I feel that because of the pandemic my family did not go through the traditions and customs that help people process and accept death. I am not sure how my parents and sister feel. I have mistakenly wondered what my aunt was up to, temporarily forgetting her death. Even though we weren't the closest I would have had a memory marker achieved through tradition and grieving/funerary customs that would have given others the peace needed. -
 2020-12-04
2020-12-04104-Year-Old World War II Veteran Beats COVID-19
This remarkable article tells the story of how a 104-year-old World War II veteran from Alabama named Major Wooten was able to beat COVID-19 in a little under two weeks after testing positive. The article describes how Major Wooten was given an infusion of a newly approved monoclonal antibody therapy named bamlanivimab, and while this treatment physically drained him temporarily, he was able to recover 24 hours later. Wooten maintains that he is still quite drained and “mentally fuzzy” after having COVID-19, but this remarkable man was able to bounce back extremely well from the disease. This article is significant to the archival collection relating to COVID-19 survivors, as well as the collection pertaining to veterans. It truly is amazing to see someone like Major Wooten survive fighting in France during World War II, and then continue to beat the odds by defeating such a deadly disease. This article will do a great job of addressing the lack of input within the archives from elderly veterans on how the COVID-19 pandemic impacted their lives. -
2022-03-18
6 Ways Covid-19 Has Impacted My Daily Life
The biggest change for me since COVID-19 became a fixture in my day-to-day life is transferring permanently from a physical classroom to a virtual one. Teaching online has its own unique set of challenges in addition to the ones that it shares with classroom teaching. While I personally do not find teaching online to be as satisfying or engaging as the physical classroom, I am hesitant to return. I hear from colleagues about the behavioral issues, the lack of motivation, and the additional stresses placed on teachers by administration. While these are things I also deal with in a way in an online environment, compounding them with the potential risk of COVID when I have immunocompromised loved ones isn’t worth the risk for me at this time. Another big change in my routine is using more delivery services than I did before March 2020. I started ordering groceries through Instacart to avoid having to go the stores after experiencing the chaos more than a few times. Even though grocery stores have calmed considerably, and the shelves remain stocked with most in-demand supplies, I still use Instacart for shopping and having my groceries delivered. Some of this is convenience, but I think that the pandemic has simply changed the way I deal with groceries for the time being. At some point, I will more than likely return to the grocery store to resume shopping in person, but for now using delivery services will remain my weekly routine. Since the pandemic relegated many people to quarantining and spending more time at home, working and going to school virtually, I have noticed that I am not as social as I used to be. While I’ve never been a very sociable person, I’ve noticed that, not only do I not crave social interaction outside of my family and close friends as much as I used to, I have to “prepare” myself for social gatherings and interactions. I have more social anxiety than I ever thought I would and going to events where I may have to hold long conversations revolving around “small talk” make me anxious and tired. I hope that I am able to work through this over time as things become more open and social gatherings and events become more common, but it is another way in which the pandemic has affected me most. When I would leave the house prior to 2020, there were certain items I made sure I had: keys, sunglasses, purse, water bottle. A change to this routine now includes making sure I have a mask in my purse and masks in my car. It’s interesting to note that they have become both a physical and symbolic item in everyday life. Yet, as we all know, it’s an item that is important to have to make sure I am prepared in the event a business requires it or I’m interacting with places and people where it’s smart to wear one. To expand on the symbolism of the mask, another example of change in my life is interacting with anti-mask strangers who think they have an obligation to comment on or ask questions of people who wear one. My daughter came home a couple nights ago very upset because a customer had been rude to her because she was wearing a mask at work. My daughter is 17 and works in a grocery store. She wears a mask to protect herself and, in her words, “to protect her family”. I’ve noticed that the pandemic seems to have made some people feel like it’s okay to comment on and berate complete strangers on personal health decisions like it’s their right. Being socially distanced for months has made some people forget their manners or maybe it’s simply brought out the worst in them. Either way, the idea that a grown man might get in a teenager’s face at the grocery store over something that is none of their business and affects them in absolutely no way, is a startling shift in how people interact with one another since this all began. Lastly, COVID has not been kind to those working in the healthcare profession, and certainly it has made visiting people who are in the hospital much more restrictive. Last September my husband was hospitalized with a collapsed lung. Visiting policies essentially made it so that one person per day could visit him. Where previously I, his parents, children, and siblings might have been able to visit him, now it only made sense for me to be the one since I could bring him what he needed, talk with his doctors, and update everyone else. This most recent February, my mom was hospitalized for a serious health concern. During her entire stay, I was not able to visit her because it was most sensible for my dad to be there for her and ensure he could bring her things from home to make her comfortable. I was able to send flowers to brighten her room, but still the one visitor per day policy held firm. Last night my mom was readmitted to the hospital for health issues related to her previous issue. My dad stays with her all day, and I am not able to because of the visiting policy. It’s frustrating and heart breaking to not be able to see her and be there for her – and to also be there for my dad who needs support and time to recharge as well. The pandemic has highlighted so many privileges and everyday things that were once taken for granted – things most people (including myself) never even thought about. -
 2022-02-25
2022-02-25Pandemic Rendition
The pattern of small, blue, unorganized, squares reminded me of a hospital or a doctor’s office, the first place I would go when I am sick. During this time, it seemed as if everyone was sick, there were no appointments available to meet with a doctor nor beds for individuals who were experiencing peak Covid symptoms. Words that describe a hospital: white walls, clean floors, sterile rooms, and order, or at least it was before the pandemic. The background is far from orderly, red is also present amongst the blue squares. This is to represent our health care professionals doing their best with the knowledge we had about this novel virus, but still witnessing many deaths. There are also green rings hovering around the two individuals. Green is often connected with germs or sickness. In the beginning cleaning products were flying off the shelves, people wanted to clean all surfaces as a preventative measure. This meant that consumers were buying several jugs of bleach, rubbing alcohol, hand sanitizer, disinfectant wipes, and many other products in surplus (creating many shortages). The air around the two individuals is filled with images of the Covid-19 virus under a microscope. Masks became a way to protect oneself from catching the virus, ultimately leading to mask mandates. The two individuals facing one another represent the mass separation we experienced during lockdown and with social distancing. -
 2020-04-15
2020-04-15An Unacceptable Wall of Sound
I live in Austin, Texas, in a neighborhood that is both in the approach flight pattern for Austin-Bergstrom International Airport and contains a hospital with a Level 1 Trauma Center and a helipad. During the first wave of the COVID-19 pandemic, the soundscape of neighborhood abruptly changed. The first thing I noticed, in the early days of a city-wide “stay-at-home” order was that I could hear more birds in the trees outside my second story apartment. It took a few days for me to realize that it was because the birdsong was not being drowned out by the sound of airplanes landing at the nearby runway. At the time I remember thinking that, perhaps, the sound of the birds was something I could look forward to every morning as I navigated suddenly having to find a new job due to the pandemic. Soon, the sound of landing airplanes was replaced with a sound that much harder to ignore. Ambulance sirens. It became noticeable after the first week, with ambulances arriving at the hospital several times an hour. By week three, it was a near constant drone broken up only by helicopters bringing even more critical patients into the city for care. By week eight, I stopped even noticing the sound of ambulances at all. The sound of the pandemic became so commonplace that my brain learned to filter out the wall of sirens as background noise. I often wonder how many ambulances carried patients who never left the hospital and how much suffering, fear, and sadness became “background noise” for us all. Given that we are entering into year three of the pandemic, and the United States has registered nearly one million COVID-19 deaths, it pains me to realize to know that number is far higher than any of us should have accepted. -
 08/21/2020
08/21/2020Caroline Birks Brown Oral History, 2020/05/31
In this interview conducted by Christina Lefebvre, Dr Caroline Birks Brown describes the drastic changes she saw while working in a hospital. She discusses patient care, the hospitals rapid response to converting floors to ICUs, and the way the hospital delt with staffing enough nurses to provide sufficient care to patients. She discusses how Spanish speaking doctors and nurses were asked to volunteer to work to avoid depersonalization and how other branches, like social workers, stepped up to provide the best care possible under the circumstances. Dr Caroline also touches on the possibility of young people getting covid and her thoughts on the patterns of the groups of people getting sick. She reenforces her appreciation of nurses and also discusses the politicization of the virus. The interview ends with her thoughts on what could have been done differently, politically and socially, to control the spread of the virus. As a mother, she talks about distanced learning and its effects on children and the importance of socialization. The last topic is about lessons she hopes we have learned. -
 08/04/2020
08/04/2020Anonymous Oral History, 2020/08/04
Anonymous oral history of Dr who is treating patients and a Massachusetts hospital. He talks about working with residents and students and how work life has changed because of the Covid-19 pandemic. He discusses one such patient who is an employee at his hospital who contracted Covid-109 and was dealing with the implications of it. He mentions that the patient is of Salvadoran decent and had to learn how to take steps and even talk after being on a ventilator. The doctor interviewed is optimistic about what this is teaching medical students and residents about their job profession and finishes the interview with his opinions about how the government response was complicated and lacking. However, at a societal level the interviewee states, the nation is handling the pandemic, well. -
 05/26/2020
05/26/2020Dr. Basil Darras Oral History, 2020/05/26
Associate Neurologist-in-Chief at Boston Children’s Hospital, Dr. Basil Darras, talks about the many changes that have come along with the COVID-19 pandemic and how it has affected healthcare workers. Dr. Darras talks about the difficulties surrounding telehealth visits and not being able to properly diagnose his patients experiencing neurological issues due to social distancing. -
 12/07/2020
12/07/2020Anonymous Oral History, 2020/12/07
The contributor of this item did not include verbal or written consent. We attempted to contact contributor (or interviewee if possible) to get consent, but got no response or had incomplete contact information. We can not allow this interview to be listened to without consent but felt the metadata is important. The recording and transcript are retained by the archive and not public. Should you wish to listen to audio file reach out to the archive and we will attempt to get consent. -
 05/12/2020
05/12/2020Kasie Meyers Oral History, 2020/05/12
Interview with Kasie Meyers by Jack Halls. In this interview, Kasie Meyers discusses how COVID has impacted her role as a nurse and the changes she and her colleagues face. She also discusses her journey as a student and how covid has impacted her studies, she touches on her role as a mother and the difficulties that have been heightened because of the pandemic. She expresses how her relationships with friends and family have changed and also discusses her view on the government and its handling of the pandemic. -
 05/21/2020
05/21/2020Rodrigo Hernández Montero Oral History, 2020/05/21
En esta entrevista Rodrigro Hernandez Montero es entrevistado por Carmen Kordick Coury concerniente al covid-19 en Costa Rica. Rodrigo trabaja en odontología tiene 40 años y vive en Heredia. Trabaja en un hospital donde empezó a escuchar del virus por primera vez. Habla sobre el cambio que ocurrió en su trabajo y del protocoló de la cirugía oral. Describe los cambios de su rutina diario, reacciones de sus pacientes y el cambio de protección que empezó a usar, como la máscara N95. Rodrigo habla de cambios de la economía y como la pandemia afecto el negocio de su papá. Habla sobre su familia y las preacauciones que ha tomado al llegar del trabajo para proteger a sus ser queridos. Rodrigo habla del cambio del dinámico familiar y los sentimientos de aislado que siente en no poder ver a su familia y sus amigos. Habla de los fuentes principales de información donde el se mantiene informado. Para terminar, Rodrigo habla del gobierno, de la xenofobia y el miedo que existe en Costa Rica. -
 2020-08-21
2020-08-21Michael Chow Oral History, 2020/08/21
C19OH -
 2021-09-09
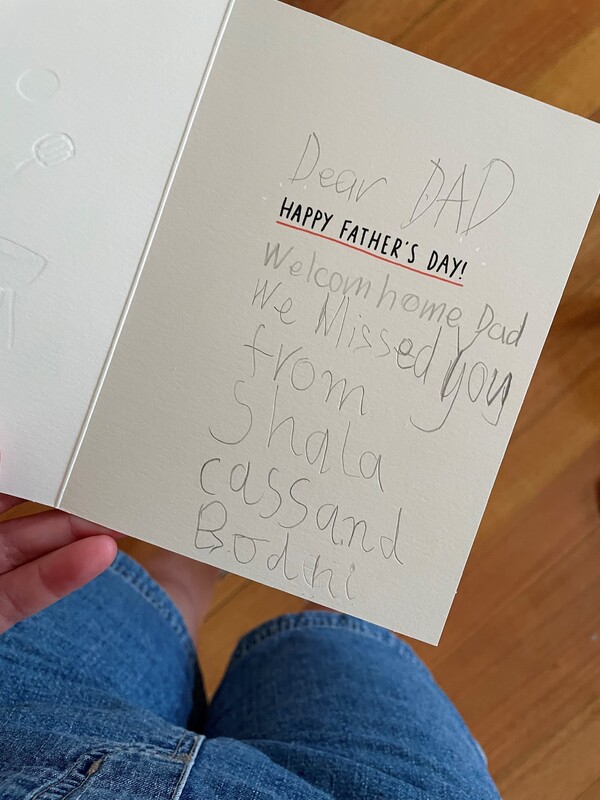
2021-09-09HIST30060 Father's Day
This is a card my siblings and I wrote for our dad. In September my father was sent into emergency as he had to have a quadruple bypass. It was rather scary as no one could visit him whilst he was recovering. We are extremely lucky that his surgery got pushed forward by his cardiologist as now our public healthcare system is now struggling and surgeries like what my dad had are being postponed. His surgery was even postponed as another cardiology ward in a nearby hospital had a covid outbreak so the nurses and doctors at his hospital had to work over there. My dad came home a couple days after Father’s Day (it was the first Father’s Day we didn’t spend with him in our lives) and is now feeling so much better. The first thing he told me when he came home was that he “never wants to get covid” because he was on a ventilator, and it was “the worst part” of the whole experience. I genuinely thought he was on the ventilator for a day or multiple days as he didn’t stop complaining about how bad it was - turns out he was only conscious with the ventilator in him for just under an hour. -
 2021-10-06
2021-10-06Covid Hospitalizations Drop Nationwide
As of September 1st, Covid-19 cases are dropping nationwide. Even though there are still hot spots across the United States, cases have dropped nearly fifty percent. -
 2021
2021Another Hospital
My mother worked at several hospitals throughout the beginning of the pandemic, as there were nurse shortages. At this particular location, she working in several units including the ICU, outpatient surgery, and distributing vaccines. This is important to me because seeing my mom dressed like this and hearing about how she worked in multiple places any given day put into perspective how dire the situation was and continues to be. -
 2021-10-08
2021-10-08Idaho and the Overrun Hospitals
Idaho hospitals are so overrun with Covid patients and so understaffed that they are drowning. Idaho has one of the lowest vaccination rates in the nation and many people are getting sick. Many hospitals on the border Idaho shares with Washington are choosing to send their sick patients to Washington. This in turn is adding to the burden carried in Eastern Washington. Many healthcare workers in Idaho are burnt out and they are helpless because of the divisiveness caused by politics and Covid. -
 2020-12-01
2020-12-01Jeff Stutler II Oral History, 2020/12/01
This is an audio recording about my family's challenges in being with my father when he had a stroke in December of 2020. Forced distancing during family emergencies can be quite a scary experience. -
 2021-10-06
2021-10-06The Fifth Wave and it's Strain on a Small Costal Town
The coastal town of Elma, Washington has been hit hard by Covid. The smaller-sized hospitals are overrun with Covid patients and the burden being put on healthcare infrastructure in the area is massive. People are having to wait hours for care at local hospitals and chances are if you call an ambulance, it will not be able to take you to a local hospital. The extra driving is eating up the EMS system's time and causing issues with getting care from emergency services. -
 2021-10-08
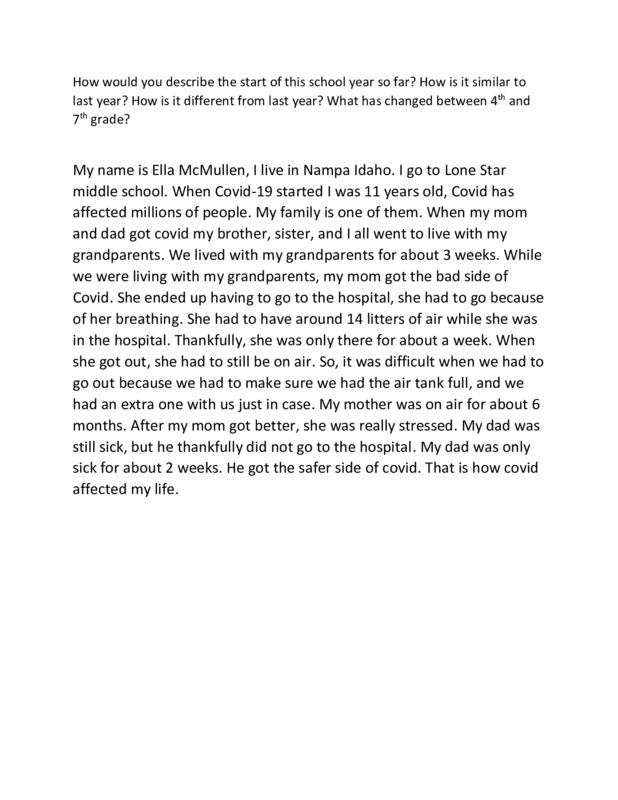
2021-10-08My covied-19 experience: Ella McMullen
My name is Ella McMullen, I live in Nampa Idaho. I go to Lone Star middle school. When Covied-19 started I was 11 years old, Covied has affected millions of people. My family is one of them. When my mom and dad got covied my brother, sister, and I all went to live with my grandparents. We lived with my grandparents for about 3 weeks. While we were living with my grandparents, my mom got the bad side of Covied. She ended up having to go to the hospital, she had to go because of her breathing. She had to have around 14 litters of air while she was in the hospital. Thankfully, she was only there for about a week. When she got out, she had to still be on air. So, it was difficult when we had to go out because we had to make sure we had the air tank full, and we had an extra one with us just in case. My mother was on air for about 6 months. After my mom got better, she was really stressed. My dad was still sick, but he thankfully did not go to the hospital. My dad was only sick for about 2 weeks. He got the safer side of covied. That is how covied affected my life. -
 2021-09-07
2021-09-07Alabama Nurses Protest Wages, COVID Working Conditions: 'We Don't Feel Appreciated'
Nurses in Birmingham, Alabama protested unequal compensation and poor working conditions at UAB Hospital by refusing to clock-in for the night shift. -
 2021-10-03T16:30
2021-10-03T16:30Ryan Nordstrom Oral History, 2021/10/03
I was interviewing the life of a lab pack chemist in Massachusetts during the midst of the Pandemic, from daily routine to personal feelings. -
 2021-10-21
2021-10-216 muertas y hay 154 hospitalizaciones
Lamentablemente, estas personas en Puerto Rico y en todo el mundo continúan muriendo y enfermando gravemente por Covid-19. Estas son las cifras del 21 de octubre de 2021: El Departamento de Salud registró en su actualización para hoy, viernes, seis muertes y 78 casos confirmados adicionales de Covid-19 en Puerto Rico. Los decesos reportados fueron en las regiones de Bayamón, Fajardo, Mayagüez y la zona Metropolitana, entre las edades de 38 a 85 años. Se informó que cuatro de los seis fallecidos no estaban vacunados, mientras que los otros dos tenían condiciones de salud preexistentes. Hay 137 adultos y 17 pacientes pediátricos hospitalizados por el virus. De estos, 47 adultos están en unidad de intensivo. -
 2020-05-01
2020-05-01The start of a pandemic that shock the medical field to its core
I have worked as a NYC paramedic for several years before the pandemic Covid-19 hit the world. As a paramedic, we were trained to deal with most situations that would happen on an emergency basis. We dealt with any situation as simple as a cut on the arm, to as complex as running a mega code on a cardiac arrest patient. When Covid-19 hit NYC, I was unaware of how bad it was going to get. At first, we thought it was a virus that was weaker than influenza, which is something we deal with on a regular basis. At this time, we would get one call a day that was related to Covid-19. I thought that everyone was over exaggerating. Over time, Covid-19 patients became more frequent, and in the matter of a month, it was the only type of call we would get. It was as if every other medical problem that people had went away. But this was because everyone that wasn't infected with Covid-19 was too afraid to go to the hospital. In the month of May 2020, things started to take a turn for the worst. People were starting to get critical on each call, where my partner and I would need to resort to extreme measures like endotracheal Intubation to help them breath. Sometimes, even intubation wouldn’t be enough, and the patient would go into cardiac arrest from the lack of oxygen in the body. It was a very difficult time for me because I felt powerless to stop people from dying to his terrible disease. In June 2020, it got so bad that the hospitals did not have capacity to accept anymore patients that came in. People were put in hallways, next to nursing stations, and hospitals had to dedicate entire floors to Covid-19 patients as they came in. Then another problem started to rear its head. My Co-workers and friends started to get sick. Those of us with families had to also make a choice, either quit their job to protect their families or live apart from them until this was all over. We did not have enough EMT’s and Paramedics to staff the ambulances we had running on any given day. Those of us who were not sick picked up anywhere from 60-90 hours a week. This struggle continues now as well. All over the world, there are not enough emergency services personal to cope with the amount of call volume that we are given each day. Over time we got adjusted to the madness and medicine advanced enough to be able to treat patients so that most did not become critical. Also, the vaccine was made available to the public and things started to get better. I shared my story to show a side of the pandemic most don’t get to experience. It shows how unprepared we were, and how we were able to prevail overtime. I will also include a video to show some insight on the pandemic that was taken with one of the companies I work with. -
2020-03
Recollections from an Oncology Nurse
My mom is an oncology nurse and has worked in the field of nursing for the past 30 years. I recently asked her to talk to me about her experience this past year as a healthcare worker. She recalled the first week in March when things were becoming intense. People were asked to wear face shields and gowns as they were working in an immune-compromised area where the patients had cancer. At the time there was no vaccine. “It was incredibly intense and scary” my mother said. “People were worried about getting Covid from other staff at the hospital and also worried about contracting Covid from the patients.” “I walked into the hospital and there was an incredible underlying anxiety, the feeling of unease was palpable. People did not talk to each other like they normally did - everyone was consumed with the thought of not using each other’s pens, putting gloves on when receiving things from the pharmacy. Things we would never have even thought of before.” She continued, “It was a feeling of both being unsettled and a blind trust you put in your coworkers to be as clean, as responsible and in isolation outside of work as you. The intensity of that feeling was there the moment you walked in. The environment had changed. People were not as happy, communicative, relaxed.” She explained how working in Covid - there was an incredible newness to it - a fear and apprehension. -
 2020-04-19
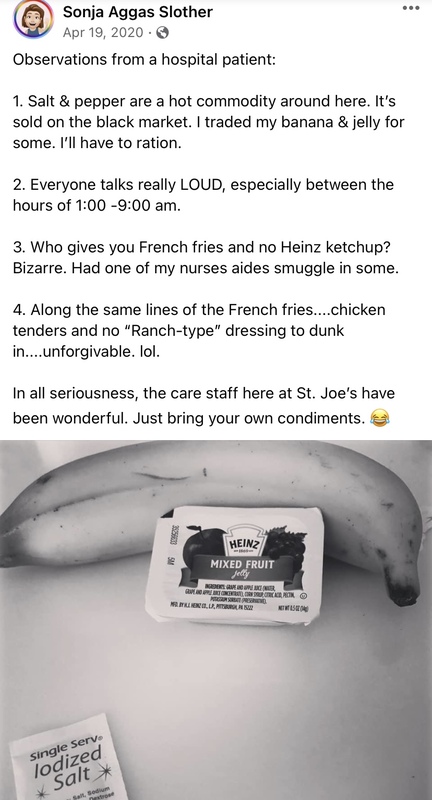
2020-04-19St. Joesph's Patient Observations
This is a post that my Mom shared on Facebook while she was in St. Joseph's in Cheektowaga for Covid 19 care. My mom discusses her observations as a Covid patient in a Covid hospital in April of 2020. -
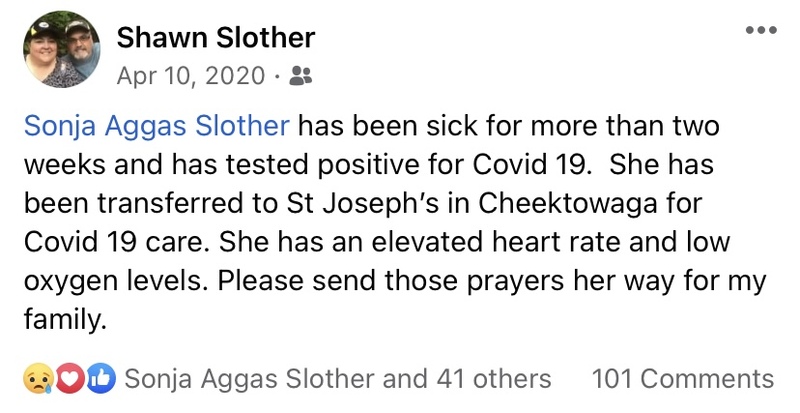 2020-04-10
2020-04-10A prayer for my mom
My mom had been sick for more than 2 weeks at my house at the end of March-early April. One morning she woke up and could barely catch her breath or breathe. My dad took both her and my brother who has similar symptoms to the emergency room. They transferred my mom to St. Joseph's for low oxygen levels and an elevated heart rate. My brother was sent home as his symptoms and current levels weren't enough to get him admitted due to the over crowding in the hospitals at this time. -
 2020-06-25
2020-06-25"Holyoke Soldiers' Home investigation: 6 takeaways from Mark Pearlstein report on coronavirus outbreak"
This article comes from MassLive and reports on the major takeaways from a report that documents where the Holyoke Soldiers' Home in Holyoke, Massachusetts, failed in its COVID-19 response. -
2021-08-25T13:03
Going to the doctor during the pandemic
Me and my mother drove down to Dell Children's hospital as we always do for our PT. Wednesday are busy days for them, so we parked on the second floor of the parking garage. My knees were feeling bad that day so we took the elevator. A family of three were also taking the elevator, and since the max capacity was four people we had to wait. We walked into the medical center (fully masked of course) but before we could leave the entryway we had to have our temperatures taken (mine was 97.1, like always) and answer a few questions "Have you had any symptoms? Fever? Headache? Coughing? Sore throat? Is anybody in your house being currently tested for COVID?" and since all the answers "no" we could enter. I've had a few days where I felt fine enough to go but because I had a headache I couldn't. The waiting room wasn't packed by any sense of the word, but since we had to make sure to keep our distance from other people we couldn't sit down anywhere. My PT (Physical Therapist) called me in, and we exercised for an hour, fully masked, which makes it a lot more uncomfortable, also making sure to keep our distance from everybody else. I went out afterwards and my mom and I went in our car, put some hand sanitizer on, and left to repeat the process next week. -
 2021-08-16
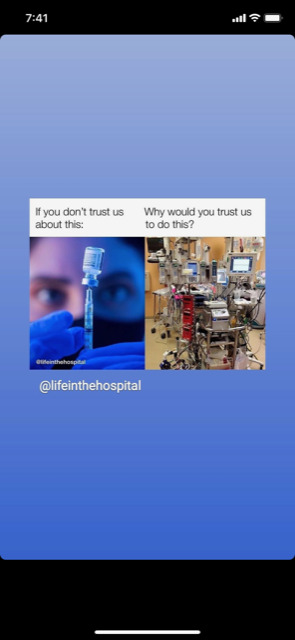
2021-08-16Truth
a nurse friend of mine posted this on her Instagram story. It's hard to understand the logic of the anti-mask, anti-vax community. -
 2020-05-28
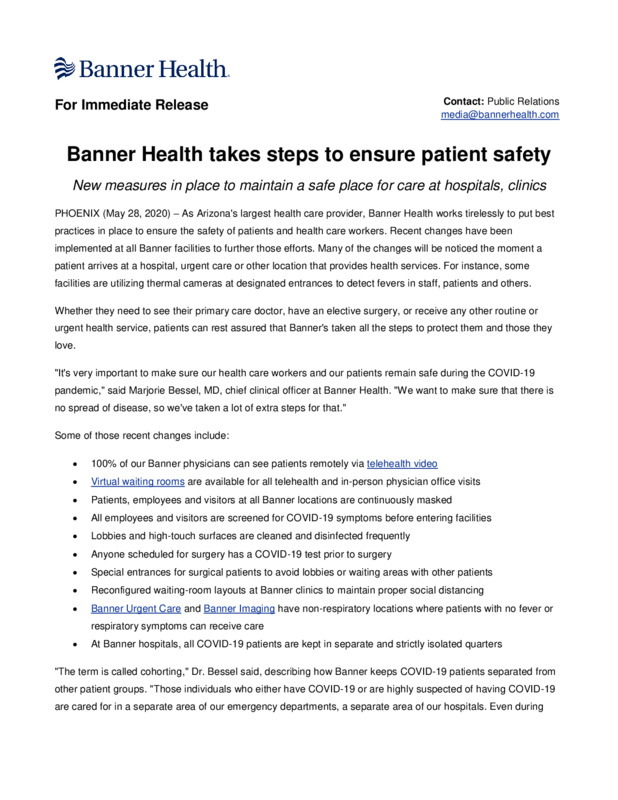
2020-05-28Banner Health takes steps to ensure patient safety
A press release describing the new measures in place to maintain a safe place for care at hospitals, clinics -
 2020-06-03
2020-06-03Banner Health launches telehealth in all hospital COVID-19 units
A press release from Banner Health announcing that hospitalists and specialists at all 28 Banner Health hospitals now can conduct virtual patient visits on COVID-19 units. This greatly preserves personal protective equipment (PPE) and allows for greater efficiency and patient and staff safety in these busy patient care units.The next phase of this telehealth technology rollout is underway at Banner Health Emergency Rooms. -
 2020-06-25
2020-06-25Banner Health Provides COVID-19 Update June 25, 2020
A press release from Banner Health providing an update on COVID 19 on June 25, 2020 -
 2020-08-11
2020-08-11Nurse handover Emergency Department, St Vincent's Hospital Melbourne
This photograph was taken in August 2020, the time when daily and active cases in Victoria's second wave were at their peak with hospitals adapting services and protocols in response. The photograph shows a nurse handover in the hospital's Emergency Department. The red line on the floor marks the boundary of the "hot zone" area dedicated to the care of patients regarded as infectious. Staff wear prescribed Level 4 PPE (Personal Protective Equipment) of gowns, face protection and N95 masks. -
 2020-03-14
2020-03-14The son of a Paramedic
It was around the time the Pandemic started and it was even worse in New York, My Father, Who was (and still is) a paramedic, Was told by his supervisor that he needed volunteers to help the hospitals in New York City. My dad decided to go, despite protest from the rest of our family. He stayed there for about two months before returning home, the time he spent there did a toll on him. Recently he was diagnosed with PTSD. he will always be an unheard hero. -
 2020-12-01
2020-12-01St Vincent's Hospital Melbourne newsletter 2020 review issue focussed on the response to the year's two COVID waves
The stories illustrate both swift adaptation of clinical practice (e.g. in the shift to telehealth consultations), the enormous efforts put in, and the outpouring of community support which helped sustain patients and staff in the difficult conditions of lockdown. -
 2021-07-29
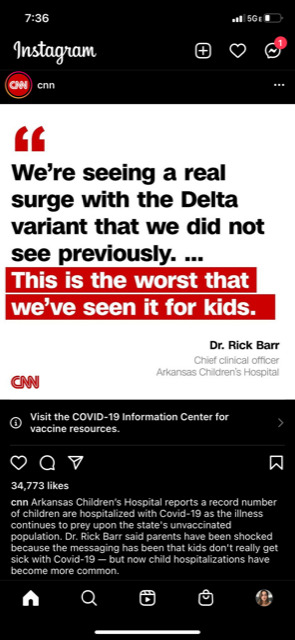
2021-07-29Delta Surge
"CNN Arkansas Children's Hospital reports a record number of children are hospitalized with Covid-19 as the illness continues to prey upon the state's unvaccinated population. Dr. Rick Barr said parents have been shocked because the messaging has been that kids don't really get sick with Covid-19 - but now child hospitalizations have become more common." -
 2020-11-20
2020-11-20Banner Health reinstates no visitor policy at all Arizona locations.
A press release detailing Banner Health reinstating no visitor policy at all Arizona locations, going into effect at 6 p.m. on Nov. 22 -
 2020-11-20
2020-11-20Banner Health joins Mayo Clinic, Dignity Health and others to spread "Mask Up" message Wearing a face mask is best way to slow down surging COVID-19 pandemic
Banner Health is pleased to join local health organizations Mayo Clinic and Dignity Health (CommonSpirit Health), as well as other top U.S. health systems, in a "Mask Up" promotion campaign designed to encourage everyone to wear a mask as protection for themselves and others against COVID-19.
