Item
Charlene Harrod-Owuamana Oral History, 2022/05/19
Title (Dublin Core)
Charlene Harrod-Owuamana Oral History, 2022/05/19
Description (Dublin Core)
Self Description: "My name is Charlene Harrod-Owuamana, I have been a nurse for 19 years. I'm a pediatric nurse, actually. And I'm during COVID I've taken a travel assignment in California, that I was so excited about that I wrote a book about it for COVID vaccine with vaccine versus shots."
Some of the things we discussed include:
Growing up in poverty and transitioning into a professional class
That health, wealth, and safety depends on your zip code in the USA
Working as a nurse in Maryland, Pennsylvania, and California
Having run a Baltimore chapter of Black Nurses Rock
Early pandemic anxieties: rioting, medicine shortages, immunocompromised patients
Working in a clinic during the pandemic, and taking on emergency room overflow
Patients ongoing needs for routine procedures during the pandemic
Working in a hospital that had a stockpile of PPE
Hospitals getting information from the CDC before USA media started significant coverage
Care and safety precautions: PPE, fit-testing training, seeing patients outside
Restaurant donations to healthcare providers
Healthcare workers’ vaccine access
Comparisons between the USA’s east coast and west coast feelings about vaccination
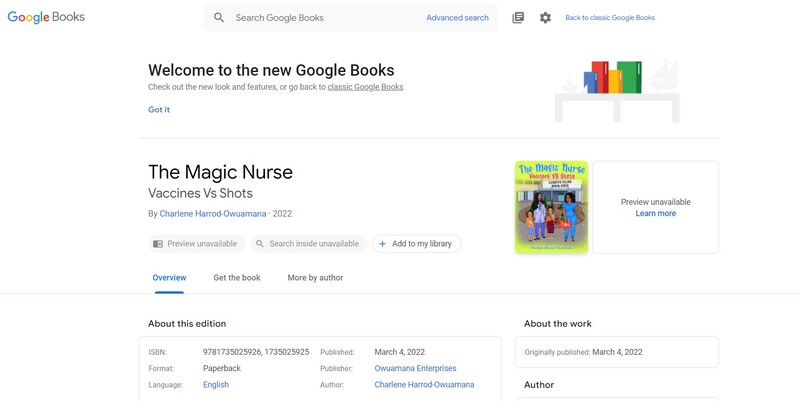
Authoring a children’s book about vaccination during the pandemic
School closures
Testing children for COVID in schools; pool-testing; training children to swab themselves
Comforting children who are afraid of needles, afraid of dying from COVID, and afraid of taking COVID home to a family member; educating children; empowering children
Nurses as the most trusted profession within the medical profession
2020: The Year of Nursing, a year of celebration cut short
Depression in nurses; it’s okay to cry/it’s okay not to be okay
Mental health and therapy-stigma among African Americans
Engaging vaccine hesitant African American patients, protecting future generations, building connections through personal experience
Respecting the personal choice of COVID vaccination
The imperfections of COVID statistics
Online socializing
Helping an immunocompromised family member
Baltimore’s murder rate
Starting a non-profit: Nursz’s Hive
Mother died when 15, and helping others grieve their mothers now
Other cultural references: Mozart, American Heart Association, the Kidney Foundation, Dunkin’ Donuts, Zoom, Tesla, Elon Musk, Facebook, Spartan, Swine flu
Growing up in poverty and transitioning into a professional class
That health, wealth, and safety depends on your zip code in the USA
Working as a nurse in Maryland, Pennsylvania, and California
Having run a Baltimore chapter of Black Nurses Rock
Early pandemic anxieties: rioting, medicine shortages, immunocompromised patients
Working in a clinic during the pandemic, and taking on emergency room overflow
Patients ongoing needs for routine procedures during the pandemic
Working in a hospital that had a stockpile of PPE
Hospitals getting information from the CDC before USA media started significant coverage
Care and safety precautions: PPE, fit-testing training, seeing patients outside
Restaurant donations to healthcare providers
Healthcare workers’ vaccine access
Comparisons between the USA’s east coast and west coast feelings about vaccination
Authoring a children’s book about vaccination during the pandemic
School closures
Testing children for COVID in schools; pool-testing; training children to swab themselves
Comforting children who are afraid of needles, afraid of dying from COVID, and afraid of taking COVID home to a family member; educating children; empowering children
Nurses as the most trusted profession within the medical profession
2020: The Year of Nursing, a year of celebration cut short
Depression in nurses; it’s okay to cry/it’s okay not to be okay
Mental health and therapy-stigma among African Americans
Engaging vaccine hesitant African American patients, protecting future generations, building connections through personal experience
Respecting the personal choice of COVID vaccination
The imperfections of COVID statistics
Online socializing
Helping an immunocompromised family member
Baltimore’s murder rate
Starting a non-profit: Nursz’s Hive
Mother died when 15, and helping others grieve their mothers now
Other cultural references: Mozart, American Heart Association, the Kidney Foundation, Dunkin’ Donuts, Zoom, Tesla, Elon Musk, Facebook, Spartan, Swine flu
Recording Date (Dublin Core)
May 19, 2022
Creator (Dublin Core)
Kit Heintzman
Charlene Harrod-Owuamana
Contributor (Dublin Core)
Kit Heintzman
Link (Bibliographic Ontology)
Controlled Vocabulary (Dublin Core)
English
Community & Community Organizations
English
Education--K12
English
Government Federal
English
Social Distance
English
Healthcare
English
Health & Wellness
English
Science
English
Social Issues
English
Religion
English
Public Health & Hospitals
English
Race & Ethnicity
Curator's Tags (Omeka Classic)
spirituality
pediatric
kindness
children
vaccinations
Contributor's Tags (a true folksonomy) (Friend of a Friend)
AIDS
Autism
diabetes
education
crying
frontline
WHO
advocacy
Baltimore
Black
California
CDC
author
children
vaccination
trust
testing
therapy
spirituality
Pfizer
myocarditis
National Guard
school
San Francisco
selfcare
prayer
police
PPE
pediatrics
nursing
nonprofit
murder
Maryland
homelessness
hesitancy
grief
empathy
Collection (Dublin Core)
Black Voices
Children
Essential Workers
Mental Health
Vaccine Stories
Date Submitted (Dublin Core)
06/29/2022
Date Modified (Dublin Core)
07/17/2022
07/18/2022
01/13/2023
03/20/2023
Date Created (Dublin Core)
05/24/2022
Interviewer (Bibliographic Ontology)
Kit Heintzman
Interviewee (Bibliographic Ontology)
Charlene Harrod-Owuamana
Location (Omeka Classic)
Baltimore
Maryland
United States of America
Format (Dublin Core)
Video
Language (Dublin Core)
English
Duration (Omeka Classic)
02:01:46
abstract (Bibliographic Ontology)
Growing up in poverty and transitioning into a professional class. That health, wealth, and safety depends on your zip code in the USA. Working as a nurse in Maryland, Pennsylvania, and California. Having run a Baltimore chapter of Black Nurses Rock. Early pandemic anxieties: rioting, medicine shortages, immunocompromised patients. Working in a clinic during the pandemic, and taking on emergency room overflow. Patients ongoing needs for routine procedures during the pandemic. Working in a hospital that had a stockpile of PPE. Hospitals getting information from the CDC before USA media started significant coverage. Care and safety precautions: PPE, fit-testing training, seeing patients outside. Restaurant donations to healthcare providers. Healthcare workers’ vaccine access. Comparisons between the USA’s east coast and west coast feelings about vaccination. Authoring a children’s book about vaccination during the pandemic. School closures. Testing children for COVID in schools; pool-testing; training children to swab themselves. Comforting children who are afraid of needles, afraid of dying from COVID, and afraid of taking COVID home to a family member; educating children; empowering children. Nurses as the most trusted profession within the medical profession. 2020: The Year of Nursing, a year of celebration cut short. Depression in nurses; it’s okay to cry/it’s okay not to be okay. Mental health and therapy-stigma among African Americans. Engaging vaccine hesitant African American patients, protecting future generations, building connections through personal experience. Respecting the personal choice of COVID vaccination. The imperfections of COVID statistics. Online socializing. Helping an immunocompromised family member. Baltimore’s murder rate. Starting a non-profit: Nursz’s Hive. Mother died when 15, and helping others grieve their mothers now.
Transcription (Omeka Classic)
Charlene Harrod-Owuamana 00:00
Hello, hello, my name is Charlene Harrod-Owuamana and I'm from Baltimore, Maryland. Today is May the 19th and it is 1:38pm.
Kit Heintzman 00:10
And you consent to having this interview recorded, digitally uploaded and publicly released under a Creative Commons license attribution noncommercial sharealike?
Charlene Harrod-Owuamana 00:20
Absolutely, absolutely.
Kit Heintzman 00:22
Could I just start by asking you to introduce yourself to anyone who might find themselves listening to this? What would you want them to know about you?
Charlene Harrod-Owuamana 00:29
Yes, my name is Charlene Harrod-Owuamana, I have been a nurse for 19 years. I'm a pediatric nurse, actually. And I'm during COVID I've taken a travel assignment in California, that I was so excited about that I wrote a book about it for COVID vaccine with vaccine versus shots.
Kit Heintzman 00:55
Would you tell me about the book?
Charlene Harrod-Owuamana 00:57
the book is for kids, you know, kids are so inquisitive, they are so immune to hearing adults and healthcare providers, talking about them coming to get shots? Well, I wrote a book to change that trajectory, changing that trajectory to having the kids think of coming to get a vaccine, and vaccines don't hurt. I explained to them, why it doesn't hurt. And they in turn, talk to me about what they think about it. And then, you know, it makes the experience so much better when it comes to get vaccines.
Kit Heintzman 01:39
What prompted you to write the book?
Charlene Harrod-Owuamana 01:43
I was in California, and a couple of kids would come in to get their vaccine. And they would always be a little hesitant. So, before I would start doing vaccines on the kids, I would start asking them questions like, what's your favorite color? Do you know why you're here? And they would tell me, and then they will say, "Well, are you gonna give me a shot?" And I say, "well, guess what? I don't give shots. I give vaccines? Would you like to try a vaccine so that you can tell your friends that it doesn't hurt, I promise you a vaccine is so thin." And then I show them the the syringe and let them hold the syringe. So, they know not to be fearful of it. And then amazing. Most of the kids love the concept of me telling them that they're getting a vaccine that they decided to call me the magic nurse. And I decided that once they told me that I was the magic nerves. I told them, "I would write a story about me and California on the West Coast because I live on the East Coast. I will write a story when I get home about it. And I did I wrote a book for them. And it's in English and Spanish.
Kit Heintzman 03:08
How have you seen people's reaction to vaccine change over time?
Charlene Harrod-Owuamana 03:13
Well, what I can say is I'm with me being a nurse on the East Coast. And when I went to work on the West Coast, I was so surprised how much education they had, how much the kids really pay attention to what's going on, and how the parents were eager to have their kids vaccinated. Whereas on the East Coast, it's totally a whole totally different atmosphere. The parents on the East Coast are so against the vaccine. And I think it's because of lack of knowledge. That's that's my take on what what's going on here.
Kit Heintzman 03:55
What you describe some of your encounters with parents who are maybe vaccine hesitant about their kids?
Charlene Harrod-Owuamana 04:03
Some of the parents that are hesitant in getting their kids vaccinated. And I've spoken to a lot of parents to figure out the reason why, you know, for me as a health care provider for over over 19 years, were 12 years have been in peds. It became a project of mines to find out why parents are so against this vaccine, one because they don't know enough to trust. And it's all about trust, believe me, it's about that trust that nothing will come it will fall to their kids. It's all about that trust that.. can we trust the government will be givin our kids something that won't be a lasting effect, or that won't cause any harm to them. Okay, so I go into a little more detail with the parents, I informed them on a dosage for kids that are five to 16, and kids that went from five to 16. And kids from 16 to adulthood. I explained to them the difference between the dosage and the reason behind the dosage. I think if the government health departments would put out other information other than just a reason to vaccinate put out in the visual reasons behind the vaccinations, you know, people are a little more educated. Now, a lot of parents are worried about autism, and they're worried about other vaccines that are already on the market. And then when it came up that COVID came on the market, you know, it made parents think differently, like, here's a new vaccine we know nothing about until the magic nurse came along, and was able to give them the inside information that I have read about, that I have done research on, and that I still currently do research on, so that my pediatric patients can assure that the information that I am giving them is coming from a reliable source.
Kit Heintzman 06:33
What brought you to nursing?
Charlene Harrod-Owuamana 06:36
Well, as a kid, I've always been fascinated. When I was younger, I went to this clinic. And I was just so fascinated with this lady in this all white that would always greet me in the clinic. She knew everything about me. She knew the reason why I was there. She knew when I needed to come back. So I said, You know what, one day I told her, I said, I need to know what was your title, what you do. And she said she was a nurse. And I said, "Well, when I grow up, I'm either going to be a nurse or doctor," because I was just so fascinated with someone else knowing a lot more about me than I knew about me. And that was able to keep me healthy as a child. And as I grew up, it just stuck with me that I should be a healthcare provider.
Kit Heintzman 07:29
Tell me a story about your life during the pandemic.
Charlene Harrod-Owuamana 07:34
Wow, my life through the pandemic has been a challenge. more so because working on a front line does not mean that I'm working in an emergency room, having patients shift through I think that people in the world forgot about people who work in clinics, people who see you when you come in just for an office visit. And me being a supervisor in a clinic, it was still as if I was in an emergency room. Because when the emergency room was not allowing people and the clinics were not turning people away, either. Because people needed some kind of confirmation with their signs and symptoms or even their daily and monthly routine visits. They needed that information. So being on the frontline at first was scary for me. Because one, we really didn't know a lot. For two, I am such a caring and giving person, that my focus when it first happened was being able to have the proper PPE equipment to be equipped to see these patients, because that was more important to me that they were seeing at least. And if they weren't going to be seen I didn't care if I had to see them outside, we can open up a tent outside where the air was where we could still see these patients, but they were physically coming into the clinic. And not knowing the unknown tend to worry a lot of people. But when I took on being a nurse, I knew that eventually something was going to be challenging for nurses. Not to mention that 2020 was the year of nursing. So, it was a lot to take on all at once. You know we were gearing up as nurses to start to celebrate, you know, nurses and 2020 but we weren't prepared for a pandemic.
Kit Heintzman 09:54
Were there any celebrations that were possible?
Charlene Harrod-Owuamana 09:57
Well, pretty much to celebrate operations were basically put on hold, because at this point, it was called survival, not only for nursing, and not only for nursing, you know, as far as the frontline went, it went further than healthcare. It went further than nurses. It went to people working in restaurants people working in and market supermarkets, because even still, without those workers in those markets, how was our health care? How was we gonna get fed, so that we can continue to do the work that needed to be done? So during this pandemic, it was much more than just nurses? To me, it was how was the mail gonna get through? How was the medicine gonna get shipped to the hospitals, we still needed delivery people for that, you know, so this last year and a half, I really had to take a step back on health care, and the pandemic, you know, I went to doing a travel assignment in Philadelphia. And we was given the option to talk about how we perceive COVID, when it first started, and it was this nurse who talked about her husband, who was a police officer, you know, none of us really thought like, you know, we were worried about how nursing proceed healthcare, nobody thought about how the police officers were getting along with health care. And when I heard that nurse story about when her husband came home, every day, he had to isolate himself from the family, because he was up in front of people, and could not keep that six feet distance that we as healthcare people who were in, like a semi controlled environment, police officers weren't in, you know, they were outside of that control box. So you know, being a nurse, it really makes you think not only about yourself, but to think about those other professions that were out in the trenches, as I call it with us, and providing care for everyone here in the United States and abroad.
Kit Heintzman 12:24
What was your access to PPE? Like in the beginning?
Charlene Harrod-Owuamana 12:28
In the beginning, it was like the unknown, but the hospital that I worked for, had a a shelter full of supplies, equipment, you know, although, you know, the news portrayed that the hospitals were not equipped. You know, the newspaper, you know, social media period, we're talking about hospitals not being equipped. But the hospital that I was in that was in Baltimore, Maryland, and several of the area hospitals that were in our area, all had PPE equipment, in a secret location, just in case something came up like this, which was really, really interesting. You know, you thought you thought from listening to CNN and listening to what was going on around the world that we were not equipped? Yes, it wasn't hundreds and hundreds and hundreds of P E. E equipment. available, but there were some to get you over until they could ship in more. Which I think in Baltimore at this area hospital, I was lucky to be an employee there.
Kit Heintzman 13:51
Do you remember when you first heard about the pandemic?
Charlene Harrod-Owuamana 13:56
Oh, well, I believe I heard about the pandemic before it went viral. Because the hospitals were getting information through the CDC and other avenues sooner than what the media got. So you know, we were preparing a little early. It wasn't like it was a great deal early, but it was at least a little earlier before it went viral. And before the media really got involved.
Kit Heintzman 14:35
What was your day to day looking like back then?
Charlene Harrod-Owuamana 14:39
My day to day was looking at even though I was wearing scrubs, I had to now add some additional equipment to wear on a daily basis. It was just it was not just scrubs. It was being able to now shift from being a supervisor in our ambulance. taury services to now shifting my services over to employee health. And now it was a all hands on deck to be sure that all of the employees at the hospital were fit tested to wear the PPE. So it wasn't just, you know, patients coming into the facility, full day of routine care. It was patients coming in for concerns as well. You know, it was not only patients worrying about how they were going to get their medication. We have diabetics, we are people who are COPD patients, we have people who were hypertensive who needed their medication, we have to worry about how was our pharmacies were going to be equipped to give out those medications. Was this going to cause rising pharmacies and how was elderly people going to get their medicine, they were already having trouble with getting their medicine. So some nurses was volunteering to go to pharmacies to pick up medicines to take them to senior buildings, because they were a vulnerable population. You know, we were worried about how our kids that were on home care how they were going to get their care people and kids that were on respiratory events and things of that nature, how are we going to care for them because they weren't immune compromised patients. So it was a lot going on during those times. Not to mention that, you know, nurses are the number one health care providers that people trust, were we still going to be able to provide that trust and relationship between our patients? And thankfully, we were and we still are the number one trusted profession out here.
Kit Heintzman 16:58
What were some of the ways that you had to adapt at the beginning of the pandemic?
Charlene Harrod-Owuamana 17:07
At the beginning of the pandemic, we had patients who did not have well, I'm gonna I'm gonna give you a scenario. I had this patient who could not get a COVID test before she came to the clinic to be seen this day. But she was not sure whether her glucometer was working or not. So she couldn't go into the emergency room because she was having COVID symptoms. And she couldn't come into our clinic, because she was having COVID symp Symptoms. So, I had to brainstorm what can I do for this patient? Because she was on a sliding scale for insulin. And as we know, insulin, diabetes is a medical emergency. So, what I did was I told that patient if she could come up to our facility that I would see her outside. One, I also told her that I would have to suit up and my equipment in order to provide her the care she needed. So she came up, I brought our glucometer machine to do her vitals. We checked her in as if she was checked in, I went outside to do her visit. And it was so amazing because I checked her personal machine against our machine. And it was accurate to let her know, the only thing she needed to do was change her batteries, and I changed my batteries for her and gave her a spare battery to change. A month afterwards, just in case the pandemic was still going on. And that made me feel so special that I was able to help her have a nurse visit outside of the facility, not knowing whether she was positive and negative. And I was able to do a rapid on her and got her a test right there. Because we were doing testing outside. And when her tests came back, she was negative. So I killed two birds with one stone with just doing a nurse visit outside instead of inside of our clinic.
Kit Heintzman 19:34
How accessible has testing been in Maryland?
Charlene Harrod-Owuamana 19:37
Right now testing have been wonderful. And right now in Baltimore City. I work for an agency where I test kids in school. We do pool testing first. And if they pool come back positive we do a rapid test. And if we can find the kid or teacher who's positive, then we don't have to do a PCR test and send it away. And it has been wonderful with the pool testing that we're doing in Baltimore, Maryland, to keep our young people safe.
Kit Heintzman 20:18
Would you explain what pool testing is?
Charlene Harrod-Owuamana 20:21
Okay, so pool testing in a school system is that we test the whole class, and we put them all in one tube, and we send it off to the lab, then the lab have a way to test this whole pool together, and see if it's a positive person within this pool testing. So it used to be anywhere from five to 20, test swabs and one two. And then we would have to go through and rapidly test everyone that was in that pool that came back positive. If we found the positive person or persons, then we're able to separate those people from the pool testing from the rapid exam. And now we do a PCR where this person swab is directly sent to the lab, so that this person can have confirmation of their positive. And then from there, the health health department is involved. And that's when they follow the person for two weeks where they have to call in and give what their signs and symptoms are, even if it's no signs and symptoms. And that's how our health department was regulating what was going on in the school system for our young generation.
Kit Heintzman 21:57
Have you been working in health care with the school system prior to the pandemic?
Charlene Harrod-Owuamana 22:01
Um, no, prior to the pandemic, I was a nurse supervisor in an ambulance ambulatory service clinic.
Kit Heintzman 22:10
When did you get involved in the schools?
Charlene Harrod-Owuamana 22:13
I got involved in the schools and November of a no, it was back in August of 2021. That's when I got involved because of course, previously the schools were closed and kids were doing virtual.
Kit Heintzman 22:33
What was your role in opening us helping the schools open back up?
Charlene Harrod-Owuamana 22:38
My role was to be sure that the kids were getting tested and knew how to test themselves. And if it was kids who needed to be tested, those were the only kids that we tested. So what made it so elegant was we trained, we had training, we took our training, and we trained the kids to swab themselves to give them the responsibility of placing a Q tip in a certain portion of their nose, and be sure that they turn the Q tip in a circular motion, to be sure to hit every wall around in their nose. And they did both noses. And then they stuck it into the test tube, which is now the kids are proud when we go in their room. They know what we're coming for. They swab their nose properly, they take the Q tip and they put the Q tip Q tip in inside the test tubes. And it's so amazing to even see a six year old to do this task perfectly.
Kit Heintzman 23:52
What we're sorry, can you do you have any stories about what teaching these kids look like?
Charlene Harrod-Owuamana 23:58
Wow, when we first started to teach these kids, it was hard to get them to place an object in their nose when they're already taught not to put anything in their noses. So, it was hard. I mean, it took it took time to teach them. You know when we first started most of it was us doing it. And you know repeatedly weekly, we were testing them. So, as the time went on, we would take their hand we would help them in the circular motion as to how to do it. We even would demonstrate to them with using our own nose to show them that one. It doesn't hurt to if you do it properly, it would be over and no time. And three, I'm still going to iterate nurses are the number one trusted profession out here. So, the kids really trust the nurses, one knowing What we're doing and to, they trust that we won't have them do anything that's going to harm them. And three, we made sure that they are first comfortable with us, because kids feed off of our vibes. So, when they connect with us, it's easy. And I don't know how or why, but when a kid connect and trust you, you almost can assure that they will do the task that's being asked.
Kit Heintzman 25:32
I'd love to hear about some of the ways you build those connections.
Charlene Harrod-Owuamana 25:36
The way I've built connections with kids, I can tell you another scenario. In California, when the parents would come to the sites where the kids were getting their vaccines, some of the parents was already apprehensive when the kids go to the clinic, because they would tell them that they're getting a shot. So, they already come with their own set up with their own mindset of how they're going to act out. So, for me, a mom came, and she just explained to me that her son had autism, and that it would take four of us to hold him because he's not going to cooperate. So, the pharmacist came and got me. She said, "Oh, Charlene, we need your magic." So, I was like, Okay, let me see what I can do. So, she said, "Okay," um, so I came out, and I held my hand out to, to him. And he looked at me, and he looked at my hand, and he turned away. So, I put my hand back. And, you know, it's just something about our hands, and kids that have autism, that really helps them. So, I stuck my hand back out to him. And he placed his hand on my hand, and he moved it. And I put my hand back. And I looked at his mom, and I say, okay, everything is fine. And his mom looked at me like, everything's fine. And I shook my head on her again. And I said, everything is fine. So, he, I put my hands back out. And he placed his hand on my hand, and he left it there. And I said to him, "Do you know why you here?" And he shook his head. And I said, "Okay, I'm here to help you. Can I help you?" And he said, "Yes." And he took his hand away. And I looked at his mom, and said, "I'm going to offer to take him to a quiet environment, so that we can give him his injection." So, I stuck my hand back out. And I said, "we're going to go over here, when it's very quiet. I'm going to explain everything to you. And I'm going to give you and get you at your injection, would that be okay?" And he said, "Yes. "And his mother looked at me. She put her hand on her chest and said, "he has never answered a stranger." And I told his mom, "I'm not a stranger. I'm the magic nurse." And she said, "Okay," so I said, "You and him go over there." And I ran over and got everything. I took him over to that corner, I cleaned his arm, and he jumped. And he looked at me, and I stuck my hands back out, and I put everything down. And he put his hands both of his hands back on my hand. And I said, "I'm going to clean your arm with alcohol, and then I'm going to give you your injection. Is that okay?" And he shook his head. And this time, I took his hand, put a glove on one, we picked up the alcohol and I had him to rub his arm. And then afterwards, I say, "Okay, now I'm gonna give you a your injection." And I was able to give him his injection, with nobody holding him without his mother. And I just saw the tears from his mom's eyes. And I just felt that day, I felt like I was standing on top of Mount Everest. You know, the, the wolf that came upon me. And his mom was so amazing that I was able to give him his vaccine without nobody holding him. So I made it my destiny to come back for him to get his second shot and 21 days, and he did the same thing. And it was so amazing to see a kid who was so apprehensive and getting a vaccine, that when I get back here to Baltimore, I started that book. I wrote that book. And now I need to figure out how to distribute the book throughout the country. Because if that could be an impact on the kids on the West Coast and California. And not to mention a kid with autism, who mom told me that it was going to take four of us to hold him who stood there and got his injection. Without nobody holding him. It warmed my heart. And that's what made me when I came home to get a position, providing, you know, swabbing test pooling for kids and on the East Coast.
Kit Heintzman 30:36
Did you do special training at any point to work with children with autism?
Charlene Harrod-Owuamana 30:41
No, I've just been doing, um, I've just been a pediatric nurse for 12 years, and it just comes with, it just comes with the territory. Um, for instance, when I went to one school to test the kids in a classroom, they were all over the place. And when I say all over the place, the teacher was like, sit down, have a seat, we're gonna do testing, blah, blah, and the kids were still all over the place. So, I said to the teacher, "I know this is not tradition in classes. But if you turn off your lights throughout the day, when your class get an uproar such as this, and have the kids place their head on a desk, and play soft music for about five minutes, your kids will calm down and be willing to learn." And I had left my sanitizer in the room. And I had to go back in the room and show now she turned off the lights. She had music playin, they had their heads down. And when I walked back past that class later that day, the kids were actually learning. So, you know, being a nurse, and being able to provide that care not only to teachers, but just provide that care to our future generation. And just given mere simple information is just turn your lights off and put on some quiet music. I told her not that upbeat music that they're used to, but some quiet, soothing music, I don't care if you put on Mozart, you know, something that they're not used to listen to, but something that can train their mind to relax? It would be so much easier for teachers at school.
Kit Heintzman 32:32
How did you handle any of the stress associated with working with kids during the pandemic?
Charlene Harrod-Owuamana 32:39
Well, for me, I allow myself to have a therapist, you know, and, you know, to talk about a therapist and African American community, most folks in the African American community like to take lead of their own mental health. They don't like taking it outside of the house, because they feel like if I talk to a psychiatrist, I'm crazy. But me, as a health care provider have been trained in mental health, I know that that's not so. So, it's kind of hard to get the older generation to, you know, be available to talk to therapists. But I wrote a book about that, too. It's called nursing. It's called The Epidemic: Nursing and Depression, you know, because nurses get depressed as well. And I need for nurses to think of mental health as self-care. And if you can't care for yourself, how can you care for someone else? So yes, it has been challenging. It has been days when I cry. You know, it has been days when I have been happy, and has been days when I thought I was positive. And I wasn't. You know, it has been days that some of my coworkers have died from COVID, which have set me back to think about, you know, helping people with COVID, helping our kids protect themselves, helping my neighbors protect themselves and still be able to function as a nurse. Because again, we have a number one trusted profession out here. So it's hard to, you know, separate work, from depression work, from personal issues with family members having COVID Not to mention patients who you've cared for for a long time, having COVID and the amount of deaths that we have helped that we have had in our country and who have been personally connected to me. So yes, mental health has always been one of in between suits. But what I can say having a therapist really helps.
Kit Heintzman 35:08
So many follow up questions. I'll try and create some order in that. Okay. Um, I guess I'll start kind of broad and vague. Is there anything more you're willing to share about your encounters with loss over the course of the pandemic?
Charlene Harrod-Owuamana 35:25
Yes. Um, so for me, I am an advocate in my city for health care. So, I volunteer for the Kidney Foundation, I helped the American Heart Association, I help our fire department, and Baltimore City, I have partnered with the police department, the fire department, city government, I have partnered with them, you know, to get the word out about health care. And, you know, it has been challenging to get people to think about the vaccine. Now me as a health care provider, I support people who get vaccines and support people who don't want vaccines. But my main thing is education. Educating people on both sides is very important to me. But it is a choice when it comes down to making that decision to get the vaccine or not. And thinking about deaths over the past year, six of my close friends have lost their mother, some due to COVID. And some just due to their medical conditions. My friends asked me, How have I been able to cope with my mom's death, because my mom died when I was 15. So now, not only do I have to put on and take off my healthcare hat, now I have to be able to assist my friends with the death of their mom over the year, especially the ones who have died due to COVID. Um, I have put together a book that I am going to do an anthology for my friends, so that they can live a legacy about their parents, and a legacy. Because when it comes down to COVID, is not one person that's affected. It's a family. It's a community that's affected. And most of us think of just that person that has been affected with COVID. But it is a whole family that is affected from COVID. And that's what I am going to do for my sick friends and their families. I am going to do an anthology. And I have been praying to God that he brings to me that the perfect Anthology for them. And yes, I have came up with the perfect name for the book. And it's called, um, hold on one second. So, the name of that book will be My Tears Flow Upward Towards Heaven's Gate. So, I want my anthology to strictly be for any loss that anybody have had during COVID to help them release some of that pain, some of that decision making that they had to make. And to know that, leaving a legacy for our loved ones who have passed before us is so amazing out here. And it would help I did a lot of writing when my mom passed away, and it helped me to get over those painful moments. And that's what I'm hoping will help my friends get over those trying times.
Kit Heintzman 39:33
Can you say more about your relationship to spirituality?
Charlene Harrod-Owuamana 39:37
Oh, yes. So, I was baptized when I was eight years old. And I have always been a very spiritual person. And when it comes to death, when my mom died, I challenge God like why would you take my mother at 15 years? I did not think that those 15 years that I was with my mom that I was equipped to function in life, and now being 55, I have grown to know that having that spiritual connection was a blessing for me, even at eight years old, and now at 55 know that that spiritual connection helped me not only to help myself, but it helped me to connect with others who are either spiritual or not spiritual, and was able to help them understand the process of grief.
Kit Heintzman 40:48
When you're helping inform people who are deciding whether or not they'd like to be vaccinated, what does some of those conversations look like?
Charlene Harrod-Owuamana 40:57
Um, some of those conversations are, you know, as a healthcare provider, we are instructed not to, um, not to have the patient. Give them a give them what vaccine they should take. So my broad information to patients is, I tell them about Moderna. I tell them about Pfizer. And I also tell them about, oh, let me think for a minute. Is Moderna, Pfizer fan? Huh.
Kit Heintzman 41:43
Is it J&J?
Charlene Harrod-Owuamana 41:44
And J&J. So, I tell them about each vaccine. I told them in the beginning, it was Pfizer one shot. It was Maderna and J&J. I mean, it was it was J&J, one vaccine. It was Moderna and Pfizer, two steps, vaccines. I would tell them, you know, you have to make the decision on which vaccine you want. I can give you literature that tells you about each that J&J vaccine is a onetime shot. Madonna and Pfizer is mRNA vaccines. Now, the dosage, I would even go as far as telling them what the dosages are, and how many days they had in between to get vaccinated. Then once the booster came along, you know, people were more versed on the most question I got when they got the booster was well, I have to get another booster. My question to them was, I'm not sure. But what I can say, if you stick to what the CDC recommend, and stay in contact with the CDC, they have websites that can send you information when it comes out. You know, just keeping people informed was the most important piece when it came down to the vaccines. But most people would say to me, “Well, which one you think I should take?” I had to be very honest with being a healthcare provider, “I cannot tell you which one to take.” So, they would say, “Well, which one did you have?” So I would be honest, and I would say “Pfizer, but it's your choice to decide which one is better fit for you.” And that's how I would keep the lines of communication with my patient, with my honest opinion as a nurse as a health care provider, that we were not allowed to tell our patient or to tell anyone which vaccine was better than the other.
Kit Heintzman 44:08
Do patients have specific questions or concerns about the mRNA vaccine as something that was new wish?
Charlene Harrod-Owuamana 44:18
And they would you know, and the only information again that I could, you know, share with them is the literature that we were given to give them to read about. Now the people who were apprehensive about getting their vaccine, I made sure that they got that paperwork so that they can read over, go home, talk to your friends, talk to your neighbors find out you know what your neighbors are doing. But for healthcare providers, we had to be bipartisan on which vaccine that they were going to get to give them the choice of What to get, and not for them to come back to us and say, “Well, you told me to get Moderna.” And this is what happened, you know, so it had to be the choice up to the patient, the customer, the consumer, on what vaccine they were getting, and we just give them the literature for the people who could not read, I read the literature to them to be sure that they would understand what they were giving.
Kit Heintzman 45:29
I love that. Thank you for doing that.
Charlene Harrod-Owuamana 45:31
Yes.
Kit Heintzman 45:34
How did you decide on Pfizer?
Charlene Harrod-Owuamana 45:36
Um, well as being a health care provider, our facility that we worked for, received certain vaccines, and pretty much it was whatever your facility received, because I got vaccine, I got vaccinated. Two months after the vaccine hit the market. It was mandatory, it was not mandatory. But it was given to us. As you know, you are on the front line. And the only way at this point that the CDC recognize that they had some containment with it was for us to get vaccinated. People who were not getting vaccinated, there were at work at first had to do a COVID test every week, to verify whether they were positive or negative. For me, I didn't feel the need to keep swabbing my nose every week, when I could get a vaccine, and it was a one shot once every 21 days or 30 days apart. And then that was it. And if I got symptoms, then I was gonna get tested. I didn't felt the need to stick that swab way up in my nose once a week. So, for me, it was a no brainer, let me just get this vaccine. But the most part of it was the reason behind it was a reason behind why I got it. Um, me again, being an African American, most African American people were apprehensive with the vaccine. "Oh, I have allergies. Oh, I have this. What would I do if I got the vaccine? Well, I was I had a latex allergy. I'm allergic to penicillin. I'm allergic to strawberries and a fruit with fuzz on it." So, a lot of people, African American descent are allergic to the same things that I'm allergic to add some more. So I say how else can I protect my future generation? I am a generation for generations. So I have great grand nieces. You know? So how can I protect my future generation of it and me be the first in the family to get it. So if I got the vaccine, and of course, the rumors, I didn't grow three eyeballs, or I didn't get sick drastically. I didn't get the vaccine and got COVID I'm still COVID Negative. I also got blood work drawn to see if I was ever exposed to COVID. And I wasn't and why some people have gotten COVID Other people have not gotten COVID other people who have had COVID twice and three times other people who have gotten vaccinated and still gotten COVID I don't know why. But if I was going to be the one who passed away from getting the vaccine, and to teach my family not to get it, I was willing to be that person. Because I had live 53 years so I was going to be that person that show the African American community that I can get vaccinated and that I was willing to put it all on the line for my future generation to be able to survive.
Kit Heintzman 49:14
Did you have conversations with family members about it?
Charlene Harrod-Owuamana 49:18
I did and I had a good conversation with myself and God about it. And it was like just go get it because if you don't and get back to nurses being the number one trust it. If you say to your patient, I am not vaccinated and I am telling you to get vaccinated then you can trust me. You know, so for patient or customer or consumer to know that I am vaccinated and boosted I am waiting to get my second booster. You know they are more they are more trusting that they can do something that I am doing And that, you know, they see me coming to work every day. They saw me get the vaccine and work that same day, you know. So, you know, it was well worth me getting the vaccine to be very trustworthy, to my patient, my residents, my consumers, my customers, it was well worth it was well worth it for me.
Kit Heintzman 50:24
How did your body react to vaccination?
Charlene Harrod-Owuamana 50:27
The first time I got vaccinated, it was challenging, I was weak, I was tired, I got a headache, I got diarrhea. You know, the diarrhea lasted for a day and a half. The headache lasted for two days. It wasn't like a migraine headache, but it was a headache that was there. So, when I took my second vaccine, I took Tylenol and a Benadryl before, I had no problems. When I got boosted, I took a Tylenol and Benadryl, I had no problem. Not that that will work for everybody, it just worked for me.
Kit Heintzman 51:12
I'd love to hear more about the place of compassion that you come from when talking with people who might choose ultimately not to be vaccinated.
Charlene Harrod-Owuamana 51:24
So, for me, for those people who are strongly against vaccinations, I have the strong sense of being that, you know, the more that I educate them, the more that the media talks about vaccination, the more we talk about people and death and dying, with or without the vaccine, I believe that the more people will come to grips that this vaccine will definitely work. Also, I believe that, you know, talking, so now, when we do test pooling in school, and the kids test pool come back positive, that's my opportunity to talk to the kid, when they come to do they have rapid to find out how they feel about COVID. And to educate them, because for me, educating a person before they become positive, and have them to understand what positive mean, helps them be able to understand what they're going through. Because not all people who are positive have symptoms. And I need for our kids to know, because in talking to these kids over the last month that I've been doing this, I find that most of the kids are upset because they think they're gonna die. Um, so for me, it's more important that I talk to them about what they feel first. Because then I can shed some light and give them some information that they're not getting, so that when they go home, they can explain to their parents, and it makes it much easier. I think that kids need to know what immune compromised means. I think that kids need to understand why is it so important to not share? Drinks, and food and chips. I even asked them. If you have a chip bag right now in your hand. And your friend asks for some, how are you going to give it to your friend? Would you let your friend dip in your chip bag? Or would you shake the chip out in your friend’s hand? Some of them say they would let their friend get their own because they don't want to touch it. Some of them will say they shake it in their hand. And I would be honest with them. I told them me when I was younger because I'm a 60s baby when I was younger, we all shared we even shared dirt. You know and we still here. I said times have changed now that we have COVID You guys aren't allowed to share and let people dip in your bag. If somebody dip in you put their hands in your bag to get chips. Them chips even now belong to them or you throw them in the trash. Plain and simple. So now the kids understand the kid don't understand. Don't Don't share your chips and don't let anybody dictate hands and your chip bag that's like opening the conversation to say hey everybody, just a Party Pack stick your hand in my chip bag. No but when I explained it to him like if somebody dip their hands and your chip bag you Then now and your chips are tainted. So now they understand that scenario. So now they're less likely to share their chips, because now they're like ill, you put your dirty hands and my chip bag now my chips dirty. So now they know the reason behind sharing those chips. So now their discussion is different, you know, they perceive this situation a whole lot different. Now they understand the whys, the house, the winds, the waves, those are not being explained to those kids earlier. It's just Oh, no, don't share. But then when I tell you why not to share, now you understand the reason behind it. And we talk about germs, germs, immune. And the reason the how, when, where and why is the best conversation to have with our future generation when you need them not to do something. And it all comes from being a pediatric nurse.
Kit Heintzman 56:09
What are some of the feelings and thoughts that kids have shared with you about the pandemic?
Charlene Harrod-Owuamana 56:15
One kid told, I said, "What do you know about COVID?" He says,"I don't want COVID to take home to my grandmother. If I'm positive, please tell me I don't want to go home. Um I'm gonna die if I get COVID? Um, my father died last week from COVID. Um, if I get COVID Will I die?" That is the most hurtful that is the most harmful question. The most complicated question that I have to answer when they asked me that, you know, because I can give them a definite answer as to whether them getting COVID. And if they're going to die? That's a question that I be honest with a kid about. I cannot tell you, if you get COVID, whether you're gonna die, what I can tell you is signs and symptoms. I can tell you what happens to a patient with an immune premise compromised. I can tell you, what happens if you have asthma, and you get COVID. But I can't tell you whether you're going to die if you get COVID. And I also tell them that I am sorry that I can't answer that question. And that question still today bothers me. Because me being an honest person to a patient and can't give them a definitive answer really bothers me. But what I do say to them is, have you had a cold before? Yes. Have you had the flu before? Yes. So, if you have had the flu before, COVID is a part of flu. So, if you have had the flu before, and you have gotten over the flu, the likelihood of you getting over COVID, it is true. I need you to do the same thing and have the same mindset you had when you had the flu. If there's somebody who said they don't they've never had the flu. Have you had a cold? Have you gotten over a cold? Yes. Then I also talked to patients and kids. Have you had a flu shot? Yes. Have you gotten over the flu? Have you had the flu this year? Since you had the flu shot? No. So why are you so apprehensive was getting the COVID vaccine, but you will take the flu shot? You know, so I compare and contrast other things that are close to COVID to present to them so that it will get them to think about you know, those other things.
Kit Heintzman 59:23
I'm curious what's it like talking to people so young about their mortality?
Charlene Harrod-Owuamana 59:29
For me as being a nurse, we are trained to talk to people no matter what their ages are. Some nurses aren't comfortable with talking to pediatric patients about that. But for me, I would rather than know, and know how I feel and give them information because for me knowledge is information and without knowledge and without information, then you don't know how to process it. And my importance of being a nurse is to help you process and to work through, you know, difficult situations.
Kit Heintzman 01:00:15
I would love a kind of rundown of how when COVID hit and you were working in the clinic, what kinds of changes happened in the sort of large-scale practice, you talked about sometimes seeing patients outside, were you at reduced capacity, what other kinds of things change?
Charlene Harrod-Owuamana 01:00:31
What change was, um, before, when patients would come into the clinic, and we would do their vitals or do their intake, we don't necessarily wear gloves. We wash our hands before the examination we wash our hands after now the COVID started, it was mandatory that we wear gloves with every patient, you know, just as with when AIDS came along, you know, things changed in health care a lot. Now, with COVID Coming along those changes, when in effect, and now are still in effect. When you do vitals blood pressure temperatures, you have to wear gloves with patience, you have to wash your hands before and after putting on gloves. You know, we have to wear masks when you're whenever you're in a healthcare facility. Yes, it's okay for you not the way of masks when you're out in the public. Yes, it's okay when you go into supermarkets now. And you don't wear masks. But no, it's not. Okay. When you come into a clinic or into a hospital, it's still mandatory that you wear a mask. So those are the changes that have changed outside of hospitals and medical institutions that inside medical institutions, you have to wear that PPE equipment, it's not up maybe or if you have to, as a health care provider, and I'm going into the schools to test them. The kids are not mandatory to wear masks. But we as healthcare professionals are mandatory to wear masks. We have just went back to win and N-95s back in schools due to the positivity rate going up. So now here in Baltimore, we do, we used to just wear the regular mask. Now we're told that we need to be fit tested. And we need to wear our N-95. And the numbers are going back up. For me, I knew the numbers never went anywhere anyway, the government sent out take home tests so people can test themselves at home. They were testing themselves at home. And if they were positive, they weren't notifying anybody. They were just positive. Whether they stayed in the house those 10 that five to 10 days or not. They were positive and they did whatever they wanted to do. And we didn't know. But for me as a healthcare provider, I've always worn my mask when outside of my home.
Kit Heintzman 01:03:03
How did you feel about the government sending out the at home tests, was it in January? It's quite recent.
Charlene Harrod-Owuamana 01:03:12
Right? For me, I was happy and still happy that the government sent those tests and instructions on how to know whether, they are positive. But what I do wish is that the government set up a way where they can confirm taking that test and finding out whether these folks were negative or positive. That's the only kickback me myself and my personal opinion about it is I wish they had something set up where they could take that test over telehealth and was able to accurately confirm what that test was and what it looked like.
Kit Heintzman 01:04:03
How did you feel about the schools reopening?
Charlene Harrod-Owuamana 01:04:07
For me, I think it was a disservice to close school. One because some of those patients, some of those kids, were not getting meals. Some of those kids homes didn't have electricity. Some of those kids, parents were not available to stay home to help them to get on a computer and work and pay bills. Some people were displaced because they couldn't not work and care for their kids to be home because the school system required parents to be available and they couldn't pay their bills. So now you had a lot of displaced people. You have people who have ran up. They have rent bills because they couldn't afford it. to stay home and educate their kids and work and pay bills, you know, and I fought the government, because over that time, while they were busy handing out all this money, they should have been handing it to these rental complexes and leasing offices to pay these people rent. So that now that it has uplifted, now, no, they are requiring these people to pay $10,000. Where are they going to get that kind of money from? Now they're displaced? Where are they going to live? We're gonna have more homeless people. Is the government worried about that about kids? Now going back to live on street because it's more and more people who can't afford to live where they are? So that part is what I'm concerned about now.
Kit Heintzman 01:05:54
What were some of the other safety precautions you took up in your day-to-day life at the beginning?
Charlene Harrod-Owuamana 01:05:59
At the beginning, you know, it was a lot of overeating, eating, because you're stressed out. It was tons and tons of patients that we had to take care of. Some of the people that were working in the ambulatory side now had to go into the hospital to help support the hospital workers with getting vital signs with helping feed patients with help passing out trays. So now, you know, you had healthcare workers, still in hospitals working, you had people who never worked now getting unemployment, and getting extra money. And here, you're still getting paid $20 an hour to do your job. And people who never worked a day in their life now average making $30 and $40 an hour, and you still out there struggling to make ends meet. And they're making ends meet and purchasing dumb stuff. Like purchasing cars and don't have license. I'm purchasing apartments and living in $2,000 month apartment and here you're living in an $800 apartment with one room, you know, so that bothered me a lot in the beginning when COVID hit, you know, certain jobs, were giving people bonuses for working. During during the um COVID. We as nurses never got paid for working. Extra bonus, thank you nothing, but we still maintain our commitment to people. It was nurses that were out there on the frontline that were dying. You know, who was getting COVID, who didn't know they had immune compromised and were dying from trying to care for someone else's family. You have negativity and people out here saying, “Well, you took on that job to be a nurse. So why are you worried?” You know, so it was the negative comments from people. It was the stress from being overworked. It was the stress just for taking care of a patient that you could not save the day. You know, you go to work, and you might have had a death, maybe once in two months. Now you have in about 10 a day. You know, where did that take our mindset? Are we still traumatized? Yes. Are we still out on the frontline? Yes. Do you think the frontline ever calm down? No. for nurses and never calm down for nurses? Yes, it's still just as detrimental as it was when it first came up. But it's the news media making that a priority? No, because now they're covering some other news. But yes, for me as a healthcare provider for me as a nurse is still evident and it still is vulnerable people are as of when it first started.
Kit Heintzman 01:08:58
Do you have coping strategies for when you lose a patient?
Charlene Harrod-Owuamana 01:09:03
Some days I lose it. Some days I go, I cry, you know, crying is nothing wrong with crying. It's nothing wrong with sharing your emotions is nothing wrong with your spiritual emotions. You know, I want people to know it's nothing wrong with crying. Whether you're male or female, you know, I am so happy that I am doing this. But what I want people to know that it is nothing wrong with crying. Please cry, please spiritually. Take care of yourself. Please know that death, grief. Emotions are something that you have to go through and your lifetime. Please don't take death is a death sentence. You know, my mom died when I was 15 not only my mom, my little brother, we had a house fire. And my mom and my younger brother died and people like, Oh, I'm so sorry. And I'm like, you know Oh, that was a journey that God placed me on. That was a journey that God has helped me to live from 15 to 55. Now, that, you know, I look at death differently than most people, you know, I look at death now as a celebration, spiritually vulnerable, I am vulnerable, you know, to when a patient of mines die, I feel the same way I felt when my mom died. And it's okay. It's okay not to be okay. It really is. And it's, it's, it's an as you can see, I light up like, you know, it is okay. And I want people to know when people say it's gonna be okay. It really truly is gonna be okay. It's just, you know, your mindset. You know, it's just spiritually, mentally emotionally talking to the right people to help you overcome this, you know, not seeking help is the worst thing that you can do during these times, or anytime when death is involved.
Kit Heintzman 01:11:09
I'd love to hear more about nurses and mental health and your sort of longer awareness of the toll that working in health care can have on nurses and then how that got ramped up during the pandemic.
Charlene Harrod-Owuamana 01:11:25
Okay, so already in place, most employers always had an employee assistance program, where you can call and you get x amount of free visits, where you can talk to, they made it accessible. Some people don't like to talk to psychiatrists and psychologists because they don't want to be perceived as crazy. A lot in healthcare, some nurses and some health care professionals don't like to work alongside someone who is depressed because they think your atomic time bomb. Now that COVID has happened, we have all experienced some type of mental depression or mental problems. So now people view it different you know, now all of that stigma about being depressed or having a mental breakdown is a new norm. You know, so now people perceive it a lot different. If I come across a person who don't perceive it, I'm comfortable. I have a conversation with them. Like, what does it look like day to day? When? If you tell me your stress, stress is a part of mental health. Let's get let's let's get it let's see it for what it is, you know, some people like, “Oh, I've never been depressed.” Have you ever been stressed out? Heard you say you were stressed yesterday? You know, that's a part of mental health. You know, how can we bring ourselves back? You know, so employers have made days like, oh, today is ice cream day, we're gonna pass out ice cream to everybody. Today is the coffee day Dunkin Donuts is coming here to provide free coffee for the staff. It's not a full cup of coffee, it's a 12 ounce cup of coffee. You know, today, we're going to do snowballs, we're going to provide snowballs for you today. You know, those little things help. When it comes down to health care providers. Over the pandemic, it was restaurants providing food for us, that made us happy, we didn't have to worry about going out to lunch. We didn't have restaurants weren't open. We had to cook food bring food in we didn't have enough food to go around the feed people at home and they have free fruits and vegetables and things like that for people. So all of that was helping, you know, it made people accountable for each other the way it used to be, you know, getting back into knowing who your neighbors are, making sure your neighbors have things that eat making sure your neighbor say making sure your your neighbor take time for self care. All of that was wonderful. You know, so for me, that is what mental health means to me to acknowledge what part of mental health you are going through pain, stress being burned out. All of that is mental health. And we need to pay attention to know that it is which means we've all had that mental breakdown at one given time in our lives.
Kit Heintzman 01:14:44
Thinking of your social life outside of work, what are some of the things that you maybe gave up because of the pandemic and maybe at this point have gone back to but??
Charlene Harrod-Owuamana 01:14:56
Right, so me and my friends we made a pact fact that once a month, we will either go to breakfast, lunch, or dinner, or we will do something together on a Saturday or something. And all of that came to a screeching halt. Everything was computer base, we would do zooms, we would do our little girls day out over zoom. You know, we weren't together. But we were together, we could see our facial expressions. If we had a bad day, we could zoom each other, we could FaceTime each other Oh, I had a rough day to day. What do you think about this? Or How are you coping with this or, and it still was that communication. It just wasn't that touchy feely communication time, and we made it through. And then when we could get together, we were so excited that we were all together, that we sat outside for lunch, still sat outside still came in with our mask on and took it down to eat. So, you know, we still think of that, you know, we still think of that time where we still have to protect ourselves, we have kids, we don't know whether one person is going around someone else, you know, I had a friend because I do a radio show. The radio show people at first everybody was contained to where they would go and what be more mindful of who they're going around. So, the people at the radio station wind up going to a family function, then their uncle got COVID, and then they got COVID. So, then we couldn't go into the station anymore. And the station had to be thoroughly cleaned and things had to be clean. And then you know, now people are back to being mindful, you will be very, very, very surprised at where your friends would say, you know, I'd be very careful about who I go around and where I go now. You know, people are more hyper vigilant with what they're doing and where they're going, and who they are being around nowadays, then, you know, before the pandemic.
Kit Heintzman 01:17:08
What do you think that vigilance does?
Charlene Harrod-Owuamana 01:17:11
What does what do I think what ?
Kit Heintzman 01:17:13
That kind of hyper vigilance is doing?
Charlene Harrod-Owuamana 01:17:16
What I think is some people are really, really taking heed to our guidelines, you know, when we were told to stay home, and you could only be out because you medical professionals, that took a great toll on a lot of people, you know, you started hearing about abuse a lot, and you started hearing about crazy things was happening in certain states and homes. And, you know, that was almost a given for health care provider to know that those things were going to be taking place. Because sometimes being out of the house was some people safe haven. And when that safe haven was taken away, it kind of took people by surprise. So, you know, having vigilance about where you're going, the people you're around the crowds that you're in it, it is really keeping a lot of us safe now.
Kit Heintzman 01:18:18
Has your relationship to touch changed over the course of the pandemic?
Charlene Harrod-Owuamana 01:18:22
Really not because me as a nurse, I still know patients, residents customers still need the the feeling of touch, you know, as being a health care provider. I wouldn't say that I feel like I'm in a different class. But I would say that my patients pin in on what's going on with them still need that touch. And you know, I still practice safely, because that's a part of my training. But the form of touch, whether it be touched with a glove on or touch with just my hand, you know, I still need to give my patient what they need and protect myself and my patient, client customer, because everybody has a different name, you know, family friends.
Kit Heintzman 01:19:21
Were you able to maintain contact with family during the pandemic?
Charlene Harrod-Owuamana 01:19:25
Absolutely. Um, I had an aunt who does have immune compromised who couldn't not go to the market. So, me and my cousins would take turns taking them groceries we would leave it out on the steps, haul them sit in a car, tell them come get the groceries carry the groceries and so we almost had to go out and buy a storage bin to put outside their house to tell them not to touch the bag. We will leave the bag open they will get the groceries out of the bin and then take the groceries in the house. So, it was a lot of you know how can we make your life safer, we will tell them go out on the back porch don't come out on the front porch, you know, because you still need that vitamin D, you still need that ray of sunshine on you. You know, just because you can't go out don't mean you can open the window when the sunshine come in, you know, things of that nature. So, we had to teach people how to get their vitamins, other ways than just eating and drinking orange juice, oranges, bananas, and things of that nature, how you just get that old, good old sun. And to explain to them that you get sun in the wintertime too. It's not those rays, that's gonna give you skin cancer, but you can still get sun during the winter months and things of that nature. So, we did a lot of education.
Kit Heintzman 01:20:48
What is the word health mean to you?
Charlene Harrod-Owuamana 01:20:51
So, the word health means not only your general health, but your emotional, spiritual, physical. It just remains it means all around health to me. It's not just your day to day function. It's everything. To me healthcare is not just what most people think is. Are you feeling good today? How's your blood pressure today? No, it's everything. It's just the whole continuum.
Kit Heintzman 01:21:25
What are some of the things that you'd like for your own health and the health of people in your life?
Charlene Harrod-Owuamana 01:21:30
Um, what I would like for health is for people to spend more time thinking about togetherness, spending more time learning about themselves and their special gift that they have been given to give to others. I have always, even as a child, my mom always taught me to give more to get more back. That's what I really enjoy given more, because I always get more back.
Kit Heintzman 01:22:02
Curious 2020, the President has had so much going on on top of the pandemic, what are some of the other big issues that have been on your mind over the last few years.
Charlene Harrod-Owuamana 01:22:15
And what's been on my mind over the last three years is our urgency for our future generation to know that we really do care about them. The urgency that I try to stress the young people that education is so important, and don't take it lightly. What I try to express to young adults is, you know, be mindful of where you're going, what you're doing and who you are around. You know, in Baltimore City, we have a murder rate that is so high, you know, not only do we have to worry about COVID pandemics and epidemics, now we have to worry about community involvement and murders. And, you know, it's just so much that we have to worry about now, that it's just not only our health that we have to worry about, we have to worry about everything and everything around us. So, for me, it's not just COVID the bigger issues such as voting, voting rights, you know, so much going on in the news is just so much all around, that we have to be, you know, mindful of, and that is concerning. So, it's just all of that to take into consideration.
Kit Heintzman 01:23:44
Sometimes when I try and think about which, like what historian is watching this and some version of the future, I like to one of them. I like to think of it as one who finds this world very weird. Because their world is so different. Explain to an alien, which is someone 50 years in the future that person's alien. What it's like to live in a city with so much murder, and how that works you.
Charlene Harrod-Owuamana 01:24:14
So, I've been in Baltimore all my life. Um, some of the murders that happen in our city I hear about and some I don't. You ride through our city, you see memorials, whether it be balloons or whether it be alcohol bottles all over the street corners and step corners, and, you know, me as a child being raised and the projects, which is a large building with a lot of people in one area. And I stress that to the kids that I meet, you know, they see me as a healthcare professional. They see me as a person that they are Sin. I grew up in a family that was wealthy, a family that did a lot. You know, I tell them, I'm just like you, I was born and raised, broke, but full of love, full of spiritual guidance full of a community building, nurturing, training me telling me what's good for me and what's not good for me. You know, that's what worked for me. That's what got me out of those areas, you know, and 2017, I started writing books. And now I'm like, at my 15th book, and I'm gonna share this with you. I wrote a chapter in the anthology called my mom's death saved my life. My family asked me, “Why would I write something like that?” I explained to them, that when I go back in my old neighborhood, and I see my friends, from when I was younger, they're either dead, strung out on drugs, and some of us are professionals. Not only healthcare professionals, lawyers, doctors, or what have you. But some of us go back in that neighborhood, and we see our friends, and I cry, you know, me and one of my best friends made a pact that we were going to be this nurse, Doctor team. And we was going to do this. And we was going to do that, and she strung out on drugs. And when she see me, she tried to avoid me. One day, I caught her. And I said to her, I said, “Please don't avoid me. But if you need help, I'm here.” You know, she started crying, I started crying, you know, it's about going back in those communities, reaching back out to your friends and your family, animals, communities, and trying to get them to work in health care facilities in those communities, because they know what they need in that community. And if you don't get yourself together to go work in your community, then your community is going to continue to go down, where I can help you get that community back up and running. Let's train you, let's send you to classes and education. And yes, college is not for everybody. And I understand that. But you can take a training course that can get you where you can go, you can actually take what you have learned throughout your life and get a job. You can be an attic, get yourself together and be a counselor who helped other people get themselves together because you've been through it. You know, what they've been through me as a nurse cannot tell an addict what they have been through because I have no experience. You as an addict can get help. And go out and start to minister start to treat, start to help your fellow worker, your fellow. Get high partner get help. And they know truly you have been through it. You know what you saw what you did? You know how you feel now you can show them the joy of how you feel now and know that it's the best now for me being born and raised in Baltimore, and went and took a contract on the West Coast and San Francisco. Not in LA Where's high crime? Right, right. Not in Oakland, where's high crime Laurie? But in San Francisco, and San Mateo, San Jose, where they are murderers, but not as much as here. The whole time that I was in San Francisco, I never saw a helicopter.
Charlene Harrod-Owuamana 01:28:40
I saw planes, but I never saw helicopter him Baltimore's like you can see helicopter 15 times a day. You know. So there is a difference in the area. And I'm quite sure in California and Oakland. I'm quite sure they have helicopters, but I was in Oakland. I never saw a helicopter when I was in Oakland. But if I was back home in Baltimore, I would have seen helicopters many times, if not heard one, you know. So I think that I am. I hate to hear that term that. You know, it's something you used to. Because when I lived in the inner city, I saw helicopter more. When I moved out to the county. I saw helicopters less. When I went to city and I saw a helicopter. I was like, What in the world is that noise? Because being out in the county, I wasn't used to hearing it. But people who are in the city are so used to hearing it, that it's a noise that they don't they don't even pay attention to. So you know, what I kind of figured out was that, you know, being in certain environments. It's not that it's a norm. It's just that your brain I mean, as you said, that norm, so it's not a norm because it's not normal, but the brain become less conscious to to extra noise.
Kit Heintzman 01:30:15
I'm curious what does safety mean to you?
Charlene Harrod-Owuamana 01:30:19
Safety means security. Safety means being informed safety mean education. Safety means safe safety means that you have someone who has your best interest or not have your best interests have a way to point you in the right direction to get it. So that's what safety means to me.
Kit Heintzman 01:30:48
You've mentioned education a few times, I'd love to hear a bit about what you think is so important about education and why you want young people especially to have it.
Charlene Harrod-Owuamana 01:30:59
So, when I was younger, and coming out of high school, a lot of people when I was younger, stressed to me that I needed to get a job, and that it was so important that I graduated from high school. So that's what was important to my generation when we were coming up. Nowadays, for the generations that are coming behind us and the millennials, a high school graduation, is not going to get them where they need to be. Not even an associate degree is going to get them where they want to be, it will get you somewhere, but it will not get you where you want to be making 90 and six and seven figures. Now, don't get me wrong, you may be lucky. And God had a plan to make you a billionaire, or had a plan to make you come up with some type of device that would help us out in America, such as the cell phones and cameras and making this able to be you know, produced. But not everybody is going to have that opportunity. Not everybody. Not everybody is going to be able to not everybody is going to be able to be rich, not everybody is going to have that opportunity. Not everybody is college material. But education is so important that our fire chief stated. I could train anybody to be a firefighter, but they have to have the willing to be educated. You know, to learn a new task doesn't take a lot, you just have to be willing to be educated. So when the fire chief said that, you know, that that gave me the hope that our city have hope that we envy other cities that have a high murder rate, that if we put Education First, we can get rid of this. But first and foremost, there are some things that need to happen first. And if it costs for us to have the national guards on our corners, then so be it, you know, but there should be nothing that could not protect us to make us safe, make us feel healthy, and make us feel like education cannot improve our environment. You know, to go a little further, what I've heard is your health, your wealth. And your safety depends on your zip code, and your city that you live in, no matter what city you live in. It's across the board, your zip code, where you live, and your health. All depends on how long you're gonna live. And it says it's studies that have been done that have proved this, you know, so that's why I stress to young people that education is so important. And when I see a kid play or I see a class that is out of control, it would behoove me to say something to that teacher and give her a little, just a little bit on how you can control your situation easily by turning off a light and let your kids sleep for 10 minutes in class.
Kit Heintzman 01:35:03
Have you had much of a chance to mentor other nurses?
Charlene Harrod-Owuamana 01:35:07
Yes, I was a part of an organization called Black Nurses Rock. I was the president, I have 52 nurses under me, which range from LPNs nursing students, all we have to nurses with PhDs that when we were in that organization, your title, your certification did not matter. But going out in the community, and advocating for health care, and given people in the community information was so important. And that's what makes me get up every day and do what I do. And I'm ever so sad that that chapter, had close. But they do have other chapters. And they do have a chapter here in Baltimore now. But I felt like I needed to do more on my own and get out and get the word out. So I started a program called Nurses Hive that go into schools and go into community after school programs that educate kids on what was taught to me to find a job. But what now I teach to them is to find a career. It is so important that our youth find careers and not a job, because going to a job and hating it every day is sad, but going to do a career that you're proud of every day, just make the light bulb shine bright on you.
Kit Heintzman 01:36:50
I would be so grateful if you shared more about credentialism and hierarchies in medicine, given what you just said about black nurses rock, not emphasizing which letters you have.
Charlene Harrod-Owuamana 01:37:05
Right. So, what happens is, what happens that I feel is when some people get education, and they get educated, they feel and it's not for all, it's just some individuals feel like if I have a master's degree, and you don't have a degree, I don't even want to be bothered with you. And you can tell me nothing because I have a master's degree. Well, I like to tell you, if you have a master's degree, and you come into my hospital sick, you don't know about medicine, you have a master's degree, and biology, all you know about pretty much is cells and how they replicate. But if you have high blood pressure, do you know that stress can take you to have a stroke? Do you know signs and symptoms of a stroke? No. But guess who do? I do? So, what I try to stress to people is if you know biology, and I am brand new, and I don't know what a cell is, yes, you would that master's degree can help me. But if you sick and you have hypertension, and you have not been trained on medication, and how I can help you and when I need to call the doctor to either get a medication to you or take a medication away from you, then you have a master's degree, me with an associate degree does not correspond because me as Associate Degree nurse can care for you in a health care facility without a master's degree. So, when people come to me about their letters behind their name, and some people really do truly have the whole alphabet behind their name. But when you come to me and you sick, and I am a LPN nurse, I do know how to care for you, how to assess you by looking at you, and how to go to the doctor and advocate for you and your healthcare and what you need and what I think you should not have. And also talk it out with that doctor to figure out why that doctor feel that you need x, y and z. So, when it comes down to having letters behind your name, I really get into it with people to let them know Yes, I am so happy that you're educated. Because when I need to know what's wrong and what's going on with a cell, I'm coming to you, but when I also need to put on my nursing hat and care for you and be sure that I'm giving you the right amount of fluids, the right medication, you know the right health care that you need, appointing you to the right doctor, the right specialist, that's going to help you come out with a good Read health score, then yes, we can communicate and not talk about letters behind your name.
Kit Heintzman 01:40:09
How do you find your relationship with doctors, by which I mean like MDs,
Charlene Harrod-Owuamana 01:40:14
With doctors, you know, each doctor, each profession, each specialty, each doctor has have a different personality. And being a nurse, you have to know your place. And you have to actually almost know your doctors you're talking to and working with. Yeah, there are some doctors who have made me mad. There are some doctors who have not listened to me. And there are some doctors who have came back to me and thanked me for my services and my decisions and my input on a patient care or diagnosis. But you know, what really, really makes it great when it comes to health care is a team that can work together. Because there's no I in team. So I do make sure I say that to a doctor or healthcare provider that's being mean or out of character. I do say there's no I in team, which means we have to care for this patient together.
Kit Heintzman 01:41:28
Would you tell me about a memory from the last two years that you think will stick with you for quite a while?
Charlene Harrod-Owuamana 01:41:38
Okay, I'm going back to California. I don't know California, California has a meaning for me. Let me tell you about this meaning. When my mom died, I was so depressed, I had to figure out a way how I could get as a child, you know, children have imagination. So, I had to figure out a way that I could deal with my mom's death. So out of the clear blue, I came up with the saying, my mom and my younger brother moved to California. And since they was in California, I couldn't see them every day. So, I was able to cope with their death a little bit. Little did I know 54 years later, I will be working in California. And when that light bulb came on that 38 years ago, I told myself this to get over my mom's death. And now I am in California. So, California really means a lot to me, because it was my safe haven until I realized that I needed to deal with death, grief, and everything. So bad. For instance, in California, a kid came to get his vaccine. And he was so petrified he laid in the floor because he did not want to get his shot. His mother's dragging him the nurse over there, they were going to make him get the shot no matter what. Because his mother said he couldn't go home if he didn't get it. So, I stopped my line. I went over there, I looked at him. I said, Now why are you laying in his floor blocking me from walking over here to the door to get some fresh air? He said he wanted me to get a shot and I don't want it. I said, “Okay, get up. Let's come walk with me. We're going out here. And we're gonna talk about this”. So, I talked to him. And what I found out was what a lot of kids, you know, think if I get COVID, I'm gonna die. Because this is what he told me. My mom said, If I don't get this vaccine, I'm going to die. Now how plants equivalent dying with vaccine? I don't know. But anyway, we went out there to have a conversation about it. So, I asked him, “Well, what is the worst part of getting a shot?” And he said, “it hurts.” I said, so if I tell you, “I'm gonna give you a vaccine and it's not going to hurt. Are you willing to go back in here and sit at my desk at my chair and take this vaccine?” He said, “Um, how about I think about it.” I said, Well, that's fine. But you only have two minutes to think about it. Because your mom says that you're gonna have to get it anyway. He said, “Well, okay, if I go back to your chair and get this vaccine, is it gonna hurt?” I say “yes, it's a possibility. But I give pediatric shots a lot. And I've been given him for 12 years. So how does that make you feel?” He said, “Well, that makes me feel a lot better.” I said, “Okay, so we're gonna walk back in here. I say you're helping school.” He said “yes, but it's not my turn.” To be a helpless Ma, my turn next month I said, “Okay, so the day is your turn to be a helper, and you have to help me. So when we get back over here and put a glove on your hand and I need you to clean your arm, so I can give you this vaccine, that's not going to hurt.” So he said, “Okay,” so we walks on and I'll give him the back. I give him the, the glove. He rubbed his arm. I say it's a clean, he said, Yeah, I said, “No, it's not clean at arm I need to clean arm to work with now so he's rubbing rubber.” I say it's a clean. He said, No, I say okay, so get the rubbing, rubbing, rubbing, rubbing. I say Okay, now we're gonna let it dry. I say, “Okay, I'm gonna give it a shot”. So, I get the needle, and I get ready to give it to him. He said, “No, no, no.” I said, “Well, we made a deal outside, that if you came back to my chair, that I was gonna give you a vaccine, this needle here. And you see is clear, right? It's not cloudy. So when it's clear, it's not gonna hurt. It's just like water.” He said, “Okay.” I said, he said no way. I say yes way. He said no way. It didn't even hurt. He said, “Mom, I got the shot. It didn't even hurt.” I say “excuse me, I didn't give you a shot, I gave you a vaccine, and it didn't hurt.” And what I did not know is that he was an autistic kid too. So that just goes to show that if you communicate with them, use kids and educate them.
Charlene Harrod-Owuamana 01:46:38
Then your job is done. You know, and I believe that that is what it's going to take for us to vaccine our country is education. And the more education that we give to our community, our friends, our family, our consumer, our customer, our Pez patients, our residents, even our enemies, then we won't be able to vaccinate our country, city, whatever, nation unless we do that. And the last thing I like to say is my kids that I talked to, I asked them if they knew who the World Health Organization was. And they told me no. I said, so who do you know, they say the CDC? I said, Okay, what I want you to do when you leave here today is I want you to look up the World Health Organization, their acronym is who look them up. And the next time you see me, tell me what you learn. You know, that means that if that kid come back to me, I educated them to go look something up. And I'm gonna see if they come back to me and tell me what, who is. And it's just the mere education that we give to people to look things up and to read things. Because when I was younger, my father used to let us read the comics and the newspaper, even though we couldn't read, we would still look at the pictures and tell what the pictures don't. So I believe if we educate our country, our community abroad, I think that we can overcome this epidemic pandemic that we're in now.
Kit Heintzman 01:48:30
How are you feeling about the immediate future?
Charlene Harrod-Owuamana 01:48:34
I feel like some little person that I have had contact with will be able to care, a lot of issues that's going on in our country and other countries, and particularly know enough about our brain so that we can use more than 2% of our brain that we're currently using right now. That is my take on this world that some little genius is going to come up with what we can use more of our brains and be able to reduce the amount of pandemics and epidemics that we go through. And like
Kit Heintzman 01:49:21
What are some of your hopes for a longer-term future?
Charlene Harrod-Owuamana 01:49:24
Some of my hopes is that my legacy live on and to the next century, to provide a lot of education and to let people know that I really truly enjoy being a nurse and being an advocate for people all over the country when it comes from the East Coast and to go work for West Coast as far as you can go. It's just amazing at what we can do in life and one person if we just add advocate for our country.
Kit Heintzman 01:50:06
I'm coming to the end of my questions and the last ones are a bit funny. I'd like to ask so you know that there's been all of this biomedical research happening because you've been teaching it. I wonder wondering what you think people in the humanities and social sciences, so people who are doing literature degrees in sociology and political science? What kinds of things should we be asking about the human side of the pandemic?
Charlene Harrod-Owuamana 01:50:35
Well, I learned today, I'm one of the kids in a school had gotten COVID probably about nine months ago. Um, yesterday, he at the school, was doing an activity that was fun for the kids at the school. He went home, he told his mom that his chest hurt. When he got home, they took him to the emergency room, and it turned out that he had myocarditis. So that's inflammation around the heart. Now, a lot of people have been hearing about people who have gotten a vaccine and have had COVID gotten a vaccine and have been diagnosed with myocarditis, which is inflammation around the heart. This child had gotten myocarditis, and that's what they diagnosed him with. But he was not vaccinated. The doctors gave him the immunoglobulin medication, and vaccinated him. And the parents were told that most people who have gotten COVID and did not get vaccinated have been coming up with myocarditis. So, me, I am going to do some more investigation and research to educate myself about that. And that's why I feel so strongly that I need to get my book out a little bit more, I'm going to send you a picture of my book cover. So that you can see what I've written about. And the other thing is, I also in the back of my book, thank a couple of organizations in California, for allowing me to vaccinate their employees as well. My thought process was to send the CEO of Tesla email to see if he could purchase some of my books to send to some of the kids in California because that's where my inspiration came from to do that, but, but I'm trying to research on who I could send an email to, and I just have not come up with it yet. But I am going to come up with it to x some of those companies like Facebook, Google Tesslar spoton, which is a part of Safeway where I was vaccinating adults in California, to see if they can purchase my book to distribute, you know, to those kids in California, who got the vaccine because that's where my inspiration came from, to write this book. And I did put them on the back of my book to thank them Fleur, what took place in California, but I haven't figured out a way to distribute it. But by the grace of God, he's going to help me figure out how to distribute that book in California.
Kit Heintzman 01:54:10
How do you think historians might remember this moment?
Charlene Harrod-Owuamana 01:54:15
Well, for me, I'm hoping that historians would remember that it took a lot of folks to collaborate together to start the process of healing the country, the nation, from this pandemic, when you know, the swine flu came out. That was a pandemic as well. And the swine flu it's no careful what but it was under control. And that is the same series of thought process that I'm hoping that history Oracle will be through, talked about forever that this pandemic was a another successful. Another successful issue that came up that was contained.
Kit Heintzman 01:55:25
We see sort of over and over again, that history ends up with blind spots. If you can use this as a chance to talk to historians of the future, what do you want to tell them, can't be forgotten about this moment? Like, yeah,
Charlene Harrod-Owuamana 01:55:43
What I would tell them that I would like for historically, to be placed on a map that it takes honesty, to give people information. And it takes a better person to admit when they are wrong. And never, ever take lightly the conversation that you have with people, for people to believe in you. Honesty, trust. And being very, very, and having a lot of integrity is so important. When it comes down to health, wealth, spiritual commitment, emotionally, physically, it takes a village to raise people, it takes a country and a nation to work together to come up with a common cure, or cars, to get to the root, and just not man to make the decision on what happens in the future, to contain anything that comes upon us as humans.
Kit Heintzman 01:57:07
I want to thank you so much for the generosity of your time and the beauty of your answers. Those are all of the questions I know how to ask at the moment, but I want to open some space. So if there's anything you'd like to share that my questions haven't made room for, please take them now.
Charlene Harrod-Owuamana 01:57:27
I would just like for the CDC, the president, governors, mayors of cities, social workers, police, all government officials to know that it really takes honesty. And it really takes a big person, if you are wrong, to make it right. People in America, really enjoy hearing sympathy, people being empathetic people really truly caring and given forth. The strength the safekeeping, the right emotions, and to know it's okay to cry. It's okay to pray to whatever God or whatever person you pray to, it's okay. Because at the end of the day, we're still people. We are in the visual, we depend on you guys expertise, to help us take in the information, to relate to information to be able to equip each individual with what we need, but also take a strong government to accept criticism from people who are living out that issue with that pandemic or or epidemic that's going on. Please be mindful that people have that people have empathy and sympathy within themselves and their country. You know, it takes a lot for any individual to sustain death, stress. And for health care workers. We are grateful to be able to assist a country, a nation with health care, but please be willing to also think of us when you think of supporting, acknowledging and giving please think of us as the front But one people not to forget those police officers, manufacturers, mail people, truck drivers, distributors, who did not have the luxury of staying home and caring for their families, and had to go out and put our lives on the line for someone else life, whether they were committed to thank us for it or not, whether they felt like we took this job, that we should be doing it and that they could say whatever they wanted to say to us, and it was okay. Because it wasn't, we do what we do on a daily basis, because that's what we feel in our heart should have been done. And that's what we will always feel in our heart. That should happen. So what I like to tell them is please don't forget those people that were really on the front line, and then just not consist of doctors and nurses. And CNAs. It was radiation techs. It was it was the whole team. It took a team of us to get where we are today. I don't want the government, the CDC, our health care world people to think that it was all them who got us here. It was a team of us. And I want to think of us as us that got us here. And that's what I want to portray.
Kit Heintzman 02:01:41
Thank you so much.
Charlene Harrod-Owuamana 02:01:42
You're welcome.
Hello, hello, my name is Charlene Harrod-Owuamana and I'm from Baltimore, Maryland. Today is May the 19th and it is 1:38pm.
Kit Heintzman 00:10
And you consent to having this interview recorded, digitally uploaded and publicly released under a Creative Commons license attribution noncommercial sharealike?
Charlene Harrod-Owuamana 00:20
Absolutely, absolutely.
Kit Heintzman 00:22
Could I just start by asking you to introduce yourself to anyone who might find themselves listening to this? What would you want them to know about you?
Charlene Harrod-Owuamana 00:29
Yes, my name is Charlene Harrod-Owuamana, I have been a nurse for 19 years. I'm a pediatric nurse, actually. And I'm during COVID I've taken a travel assignment in California, that I was so excited about that I wrote a book about it for COVID vaccine with vaccine versus shots.
Kit Heintzman 00:55
Would you tell me about the book?
Charlene Harrod-Owuamana 00:57
the book is for kids, you know, kids are so inquisitive, they are so immune to hearing adults and healthcare providers, talking about them coming to get shots? Well, I wrote a book to change that trajectory, changing that trajectory to having the kids think of coming to get a vaccine, and vaccines don't hurt. I explained to them, why it doesn't hurt. And they in turn, talk to me about what they think about it. And then, you know, it makes the experience so much better when it comes to get vaccines.
Kit Heintzman 01:39
What prompted you to write the book?
Charlene Harrod-Owuamana 01:43
I was in California, and a couple of kids would come in to get their vaccine. And they would always be a little hesitant. So, before I would start doing vaccines on the kids, I would start asking them questions like, what's your favorite color? Do you know why you're here? And they would tell me, and then they will say, "Well, are you gonna give me a shot?" And I say, "well, guess what? I don't give shots. I give vaccines? Would you like to try a vaccine so that you can tell your friends that it doesn't hurt, I promise you a vaccine is so thin." And then I show them the the syringe and let them hold the syringe. So, they know not to be fearful of it. And then amazing. Most of the kids love the concept of me telling them that they're getting a vaccine that they decided to call me the magic nurse. And I decided that once they told me that I was the magic nerves. I told them, "I would write a story about me and California on the West Coast because I live on the East Coast. I will write a story when I get home about it. And I did I wrote a book for them. And it's in English and Spanish.
Kit Heintzman 03:08
How have you seen people's reaction to vaccine change over time?
Charlene Harrod-Owuamana 03:13
Well, what I can say is I'm with me being a nurse on the East Coast. And when I went to work on the West Coast, I was so surprised how much education they had, how much the kids really pay attention to what's going on, and how the parents were eager to have their kids vaccinated. Whereas on the East Coast, it's totally a whole totally different atmosphere. The parents on the East Coast are so against the vaccine. And I think it's because of lack of knowledge. That's that's my take on what what's going on here.
Kit Heintzman 03:55
What you describe some of your encounters with parents who are maybe vaccine hesitant about their kids?
Charlene Harrod-Owuamana 04:03
Some of the parents that are hesitant in getting their kids vaccinated. And I've spoken to a lot of parents to figure out the reason why, you know, for me as a health care provider for over over 19 years, were 12 years have been in peds. It became a project of mines to find out why parents are so against this vaccine, one because they don't know enough to trust. And it's all about trust, believe me, it's about that trust that nothing will come it will fall to their kids. It's all about that trust that.. can we trust the government will be givin our kids something that won't be a lasting effect, or that won't cause any harm to them. Okay, so I go into a little more detail with the parents, I informed them on a dosage for kids that are five to 16, and kids that went from five to 16. And kids from 16 to adulthood. I explained to them the difference between the dosage and the reason behind the dosage. I think if the government health departments would put out other information other than just a reason to vaccinate put out in the visual reasons behind the vaccinations, you know, people are a little more educated. Now, a lot of parents are worried about autism, and they're worried about other vaccines that are already on the market. And then when it came up that COVID came on the market, you know, it made parents think differently, like, here's a new vaccine we know nothing about until the magic nurse came along, and was able to give them the inside information that I have read about, that I have done research on, and that I still currently do research on, so that my pediatric patients can assure that the information that I am giving them is coming from a reliable source.
Kit Heintzman 06:33
What brought you to nursing?
Charlene Harrod-Owuamana 06:36
Well, as a kid, I've always been fascinated. When I was younger, I went to this clinic. And I was just so fascinated with this lady in this all white that would always greet me in the clinic. She knew everything about me. She knew the reason why I was there. She knew when I needed to come back. So I said, You know what, one day I told her, I said, I need to know what was your title, what you do. And she said she was a nurse. And I said, "Well, when I grow up, I'm either going to be a nurse or doctor," because I was just so fascinated with someone else knowing a lot more about me than I knew about me. And that was able to keep me healthy as a child. And as I grew up, it just stuck with me that I should be a healthcare provider.
Kit Heintzman 07:29
Tell me a story about your life during the pandemic.
Charlene Harrod-Owuamana 07:34
Wow, my life through the pandemic has been a challenge. more so because working on a front line does not mean that I'm working in an emergency room, having patients shift through I think that people in the world forgot about people who work in clinics, people who see you when you come in just for an office visit. And me being a supervisor in a clinic, it was still as if I was in an emergency room. Because when the emergency room was not allowing people and the clinics were not turning people away, either. Because people needed some kind of confirmation with their signs and symptoms or even their daily and monthly routine visits. They needed that information. So being on the frontline at first was scary for me. Because one, we really didn't know a lot. For two, I am such a caring and giving person, that my focus when it first happened was being able to have the proper PPE equipment to be equipped to see these patients, because that was more important to me that they were seeing at least. And if they weren't going to be seen I didn't care if I had to see them outside, we can open up a tent outside where the air was where we could still see these patients, but they were physically coming into the clinic. And not knowing the unknown tend to worry a lot of people. But when I took on being a nurse, I knew that eventually something was going to be challenging for nurses. Not to mention that 2020 was the year of nursing. So, it was a lot to take on all at once. You know we were gearing up as nurses to start to celebrate, you know, nurses and 2020 but we weren't prepared for a pandemic.
Kit Heintzman 09:54
Were there any celebrations that were possible?
Charlene Harrod-Owuamana 09:57
Well, pretty much to celebrate operations were basically put on hold, because at this point, it was called survival, not only for nursing, and not only for nursing, you know, as far as the frontline went, it went further than healthcare. It went further than nurses. It went to people working in restaurants people working in and market supermarkets, because even still, without those workers in those markets, how was our health care? How was we gonna get fed, so that we can continue to do the work that needed to be done? So during this pandemic, it was much more than just nurses? To me, it was how was the mail gonna get through? How was the medicine gonna get shipped to the hospitals, we still needed delivery people for that, you know, so this last year and a half, I really had to take a step back on health care, and the pandemic, you know, I went to doing a travel assignment in Philadelphia. And we was given the option to talk about how we perceive COVID, when it first started, and it was this nurse who talked about her husband, who was a police officer, you know, none of us really thought like, you know, we were worried about how nursing proceed healthcare, nobody thought about how the police officers were getting along with health care. And when I heard that nurse story about when her husband came home, every day, he had to isolate himself from the family, because he was up in front of people, and could not keep that six feet distance that we as healthcare people who were in, like a semi controlled environment, police officers weren't in, you know, they were outside of that control box. So you know, being a nurse, it really makes you think not only about yourself, but to think about those other professions that were out in the trenches, as I call it with us, and providing care for everyone here in the United States and abroad.
Kit Heintzman 12:24
What was your access to PPE? Like in the beginning?
Charlene Harrod-Owuamana 12:28
In the beginning, it was like the unknown, but the hospital that I worked for, had a a shelter full of supplies, equipment, you know, although, you know, the news portrayed that the hospitals were not equipped. You know, the newspaper, you know, social media period, we're talking about hospitals not being equipped. But the hospital that I was in that was in Baltimore, Maryland, and several of the area hospitals that were in our area, all had PPE equipment, in a secret location, just in case something came up like this, which was really, really interesting. You know, you thought you thought from listening to CNN and listening to what was going on around the world that we were not equipped? Yes, it wasn't hundreds and hundreds and hundreds of P E. E equipment. available, but there were some to get you over until they could ship in more. Which I think in Baltimore at this area hospital, I was lucky to be an employee there.
Kit Heintzman 13:51
Do you remember when you first heard about the pandemic?
Charlene Harrod-Owuamana 13:56
Oh, well, I believe I heard about the pandemic before it went viral. Because the hospitals were getting information through the CDC and other avenues sooner than what the media got. So you know, we were preparing a little early. It wasn't like it was a great deal early, but it was at least a little earlier before it went viral. And before the media really got involved.
Kit Heintzman 14:35
What was your day to day looking like back then?
Charlene Harrod-Owuamana 14:39
My day to day was looking at even though I was wearing scrubs, I had to now add some additional equipment to wear on a daily basis. It was just it was not just scrubs. It was being able to now shift from being a supervisor in our ambulance. taury services to now shifting my services over to employee health. And now it was a all hands on deck to be sure that all of the employees at the hospital were fit tested to wear the PPE. So it wasn't just, you know, patients coming into the facility, full day of routine care. It was patients coming in for concerns as well. You know, it was not only patients worrying about how they were going to get their medication. We have diabetics, we are people who are COPD patients, we have people who were hypertensive who needed their medication, we have to worry about how was our pharmacies were going to be equipped to give out those medications. Was this going to cause rising pharmacies and how was elderly people going to get their medicine, they were already having trouble with getting their medicine. So some nurses was volunteering to go to pharmacies to pick up medicines to take them to senior buildings, because they were a vulnerable population. You know, we were worried about how our kids that were on home care how they were going to get their care people and kids that were on respiratory events and things of that nature, how are we going to care for them because they weren't immune compromised patients. So it was a lot going on during those times. Not to mention that, you know, nurses are the number one health care providers that people trust, were we still going to be able to provide that trust and relationship between our patients? And thankfully, we were and we still are the number one trusted profession out here.
Kit Heintzman 16:58
What were some of the ways that you had to adapt at the beginning of the pandemic?
Charlene Harrod-Owuamana 17:07
At the beginning of the pandemic, we had patients who did not have well, I'm gonna I'm gonna give you a scenario. I had this patient who could not get a COVID test before she came to the clinic to be seen this day. But she was not sure whether her glucometer was working or not. So she couldn't go into the emergency room because she was having COVID symptoms. And she couldn't come into our clinic, because she was having COVID symp Symptoms. So, I had to brainstorm what can I do for this patient? Because she was on a sliding scale for insulin. And as we know, insulin, diabetes is a medical emergency. So, what I did was I told that patient if she could come up to our facility that I would see her outside. One, I also told her that I would have to suit up and my equipment in order to provide her the care she needed. So she came up, I brought our glucometer machine to do her vitals. We checked her in as if she was checked in, I went outside to do her visit. And it was so amazing because I checked her personal machine against our machine. And it was accurate to let her know, the only thing she needed to do was change her batteries, and I changed my batteries for her and gave her a spare battery to change. A month afterwards, just in case the pandemic was still going on. And that made me feel so special that I was able to help her have a nurse visit outside of the facility, not knowing whether she was positive and negative. And I was able to do a rapid on her and got her a test right there. Because we were doing testing outside. And when her tests came back, she was negative. So I killed two birds with one stone with just doing a nurse visit outside instead of inside of our clinic.
Kit Heintzman 19:34
How accessible has testing been in Maryland?
Charlene Harrod-Owuamana 19:37
Right now testing have been wonderful. And right now in Baltimore City. I work for an agency where I test kids in school. We do pool testing first. And if they pool come back positive we do a rapid test. And if we can find the kid or teacher who's positive, then we don't have to do a PCR test and send it away. And it has been wonderful with the pool testing that we're doing in Baltimore, Maryland, to keep our young people safe.
Kit Heintzman 20:18
Would you explain what pool testing is?
Charlene Harrod-Owuamana 20:21
Okay, so pool testing in a school system is that we test the whole class, and we put them all in one tube, and we send it off to the lab, then the lab have a way to test this whole pool together, and see if it's a positive person within this pool testing. So it used to be anywhere from five to 20, test swabs and one two. And then we would have to go through and rapidly test everyone that was in that pool that came back positive. If we found the positive person or persons, then we're able to separate those people from the pool testing from the rapid exam. And now we do a PCR where this person swab is directly sent to the lab, so that this person can have confirmation of their positive. And then from there, the health health department is involved. And that's when they follow the person for two weeks where they have to call in and give what their signs and symptoms are, even if it's no signs and symptoms. And that's how our health department was regulating what was going on in the school system for our young generation.
Kit Heintzman 21:57
Have you been working in health care with the school system prior to the pandemic?
Charlene Harrod-Owuamana 22:01
Um, no, prior to the pandemic, I was a nurse supervisor in an ambulance ambulatory service clinic.
Kit Heintzman 22:10
When did you get involved in the schools?
Charlene Harrod-Owuamana 22:13
I got involved in the schools and November of a no, it was back in August of 2021. That's when I got involved because of course, previously the schools were closed and kids were doing virtual.
Kit Heintzman 22:33
What was your role in opening us helping the schools open back up?
Charlene Harrod-Owuamana 22:38
My role was to be sure that the kids were getting tested and knew how to test themselves. And if it was kids who needed to be tested, those were the only kids that we tested. So what made it so elegant was we trained, we had training, we took our training, and we trained the kids to swab themselves to give them the responsibility of placing a Q tip in a certain portion of their nose, and be sure that they turn the Q tip in a circular motion, to be sure to hit every wall around in their nose. And they did both noses. And then they stuck it into the test tube, which is now the kids are proud when we go in their room. They know what we're coming for. They swab their nose properly, they take the Q tip and they put the Q tip Q tip in inside the test tubes. And it's so amazing to even see a six year old to do this task perfectly.
Kit Heintzman 23:52
What we're sorry, can you do you have any stories about what teaching these kids look like?
Charlene Harrod-Owuamana 23:58
Wow, when we first started to teach these kids, it was hard to get them to place an object in their nose when they're already taught not to put anything in their noses. So, it was hard. I mean, it took it took time to teach them. You know when we first started most of it was us doing it. And you know repeatedly weekly, we were testing them. So, as the time went on, we would take their hand we would help them in the circular motion as to how to do it. We even would demonstrate to them with using our own nose to show them that one. It doesn't hurt to if you do it properly, it would be over and no time. And three, I'm still going to iterate nurses are the number one trusted profession out here. So, the kids really trust the nurses, one knowing What we're doing and to, they trust that we won't have them do anything that's going to harm them. And three, we made sure that they are first comfortable with us, because kids feed off of our vibes. So, when they connect with us, it's easy. And I don't know how or why, but when a kid connect and trust you, you almost can assure that they will do the task that's being asked.
Kit Heintzman 25:32
I'd love to hear about some of the ways you build those connections.
Charlene Harrod-Owuamana 25:36
The way I've built connections with kids, I can tell you another scenario. In California, when the parents would come to the sites where the kids were getting their vaccines, some of the parents was already apprehensive when the kids go to the clinic, because they would tell them that they're getting a shot. So, they already come with their own set up with their own mindset of how they're going to act out. So, for me, a mom came, and she just explained to me that her son had autism, and that it would take four of us to hold him because he's not going to cooperate. So, the pharmacist came and got me. She said, "Oh, Charlene, we need your magic." So, I was like, Okay, let me see what I can do. So, she said, "Okay," um, so I came out, and I held my hand out to, to him. And he looked at me, and he looked at my hand, and he turned away. So, I put my hand back. And, you know, it's just something about our hands, and kids that have autism, that really helps them. So, I stuck my hand back out to him. And he placed his hand on my hand, and he moved it. And I put my hand back. And I looked at his mom, and I say, okay, everything is fine. And his mom looked at me like, everything's fine. And I shook my head on her again. And I said, everything is fine. So, he, I put my hands back out. And he placed his hand on my hand, and he left it there. And I said to him, "Do you know why you here?" And he shook his head. And I said, "Okay, I'm here to help you. Can I help you?" And he said, "Yes." And he took his hand away. And I looked at his mom, and said, "I'm going to offer to take him to a quiet environment, so that we can give him his injection." So, I stuck my hand back out. And I said, "we're going to go over here, when it's very quiet. I'm going to explain everything to you. And I'm going to give you and get you at your injection, would that be okay?" And he said, "Yes. "And his mother looked at me. She put her hand on her chest and said, "he has never answered a stranger." And I told his mom, "I'm not a stranger. I'm the magic nurse." And she said, "Okay," so I said, "You and him go over there." And I ran over and got everything. I took him over to that corner, I cleaned his arm, and he jumped. And he looked at me, and I stuck my hands back out, and I put everything down. And he put his hands both of his hands back on my hand. And I said, "I'm going to clean your arm with alcohol, and then I'm going to give you your injection. Is that okay?" And he shook his head. And this time, I took his hand, put a glove on one, we picked up the alcohol and I had him to rub his arm. And then afterwards, I say, "Okay, now I'm gonna give you a your injection." And I was able to give him his injection, with nobody holding him without his mother. And I just saw the tears from his mom's eyes. And I just felt that day, I felt like I was standing on top of Mount Everest. You know, the, the wolf that came upon me. And his mom was so amazing that I was able to give him his vaccine without nobody holding him. So I made it my destiny to come back for him to get his second shot and 21 days, and he did the same thing. And it was so amazing to see a kid who was so apprehensive and getting a vaccine, that when I get back here to Baltimore, I started that book. I wrote that book. And now I need to figure out how to distribute the book throughout the country. Because if that could be an impact on the kids on the West Coast and California. And not to mention a kid with autism, who mom told me that it was going to take four of us to hold him who stood there and got his injection. Without nobody holding him. It warmed my heart. And that's what made me when I came home to get a position, providing, you know, swabbing test pooling for kids and on the East Coast.
Kit Heintzman 30:36
Did you do special training at any point to work with children with autism?
Charlene Harrod-Owuamana 30:41
No, I've just been doing, um, I've just been a pediatric nurse for 12 years, and it just comes with, it just comes with the territory. Um, for instance, when I went to one school to test the kids in a classroom, they were all over the place. And when I say all over the place, the teacher was like, sit down, have a seat, we're gonna do testing, blah, blah, and the kids were still all over the place. So, I said to the teacher, "I know this is not tradition in classes. But if you turn off your lights throughout the day, when your class get an uproar such as this, and have the kids place their head on a desk, and play soft music for about five minutes, your kids will calm down and be willing to learn." And I had left my sanitizer in the room. And I had to go back in the room and show now she turned off the lights. She had music playin, they had their heads down. And when I walked back past that class later that day, the kids were actually learning. So, you know, being a nurse, and being able to provide that care not only to teachers, but just provide that care to our future generation. And just given mere simple information is just turn your lights off and put on some quiet music. I told her not that upbeat music that they're used to, but some quiet, soothing music, I don't care if you put on Mozart, you know, something that they're not used to listen to, but something that can train their mind to relax? It would be so much easier for teachers at school.
Kit Heintzman 32:32
How did you handle any of the stress associated with working with kids during the pandemic?
Charlene Harrod-Owuamana 32:39
Well, for me, I allow myself to have a therapist, you know, and, you know, to talk about a therapist and African American community, most folks in the African American community like to take lead of their own mental health. They don't like taking it outside of the house, because they feel like if I talk to a psychiatrist, I'm crazy. But me, as a health care provider have been trained in mental health, I know that that's not so. So, it's kind of hard to get the older generation to, you know, be available to talk to therapists. But I wrote a book about that, too. It's called nursing. It's called The Epidemic: Nursing and Depression, you know, because nurses get depressed as well. And I need for nurses to think of mental health as self-care. And if you can't care for yourself, how can you care for someone else? So yes, it has been challenging. It has been days when I cry. You know, it has been days when I have been happy, and has been days when I thought I was positive. And I wasn't. You know, it has been days that some of my coworkers have died from COVID, which have set me back to think about, you know, helping people with COVID, helping our kids protect themselves, helping my neighbors protect themselves and still be able to function as a nurse. Because again, we have a number one trusted profession out here. So it's hard to, you know, separate work, from depression work, from personal issues with family members having COVID Not to mention patients who you've cared for for a long time, having COVID and the amount of deaths that we have helped that we have had in our country and who have been personally connected to me. So yes, mental health has always been one of in between suits. But what I can say having a therapist really helps.
Kit Heintzman 35:08
So many follow up questions. I'll try and create some order in that. Okay. Um, I guess I'll start kind of broad and vague. Is there anything more you're willing to share about your encounters with loss over the course of the pandemic?
Charlene Harrod-Owuamana 35:25
Yes. Um, so for me, I am an advocate in my city for health care. So, I volunteer for the Kidney Foundation, I helped the American Heart Association, I help our fire department, and Baltimore City, I have partnered with the police department, the fire department, city government, I have partnered with them, you know, to get the word out about health care. And, you know, it has been challenging to get people to think about the vaccine. Now me as a health care provider, I support people who get vaccines and support people who don't want vaccines. But my main thing is education. Educating people on both sides is very important to me. But it is a choice when it comes down to making that decision to get the vaccine or not. And thinking about deaths over the past year, six of my close friends have lost their mother, some due to COVID. And some just due to their medical conditions. My friends asked me, How have I been able to cope with my mom's death, because my mom died when I was 15. So now, not only do I have to put on and take off my healthcare hat, now I have to be able to assist my friends with the death of their mom over the year, especially the ones who have died due to COVID. Um, I have put together a book that I am going to do an anthology for my friends, so that they can live a legacy about their parents, and a legacy. Because when it comes down to COVID, is not one person that's affected. It's a family. It's a community that's affected. And most of us think of just that person that has been affected with COVID. But it is a whole family that is affected from COVID. And that's what I am going to do for my sick friends and their families. I am going to do an anthology. And I have been praying to God that he brings to me that the perfect Anthology for them. And yes, I have came up with the perfect name for the book. And it's called, um, hold on one second. So, the name of that book will be My Tears Flow Upward Towards Heaven's Gate. So, I want my anthology to strictly be for any loss that anybody have had during COVID to help them release some of that pain, some of that decision making that they had to make. And to know that, leaving a legacy for our loved ones who have passed before us is so amazing out here. And it would help I did a lot of writing when my mom passed away, and it helped me to get over those painful moments. And that's what I'm hoping will help my friends get over those trying times.
Kit Heintzman 39:33
Can you say more about your relationship to spirituality?
Charlene Harrod-Owuamana 39:37
Oh, yes. So, I was baptized when I was eight years old. And I have always been a very spiritual person. And when it comes to death, when my mom died, I challenge God like why would you take my mother at 15 years? I did not think that those 15 years that I was with my mom that I was equipped to function in life, and now being 55, I have grown to know that having that spiritual connection was a blessing for me, even at eight years old, and now at 55 know that that spiritual connection helped me not only to help myself, but it helped me to connect with others who are either spiritual or not spiritual, and was able to help them understand the process of grief.
Kit Heintzman 40:48
When you're helping inform people who are deciding whether or not they'd like to be vaccinated, what does some of those conversations look like?
Charlene Harrod-Owuamana 40:57
Um, some of those conversations are, you know, as a healthcare provider, we are instructed not to, um, not to have the patient. Give them a give them what vaccine they should take. So my broad information to patients is, I tell them about Moderna. I tell them about Pfizer. And I also tell them about, oh, let me think for a minute. Is Moderna, Pfizer fan? Huh.
Kit Heintzman 41:43
Is it J&J?
Charlene Harrod-Owuamana 41:44
And J&J. So, I tell them about each vaccine. I told them in the beginning, it was Pfizer one shot. It was Maderna and J&J. I mean, it was it was J&J, one vaccine. It was Moderna and Pfizer, two steps, vaccines. I would tell them, you know, you have to make the decision on which vaccine you want. I can give you literature that tells you about each that J&J vaccine is a onetime shot. Madonna and Pfizer is mRNA vaccines. Now, the dosage, I would even go as far as telling them what the dosages are, and how many days they had in between to get vaccinated. Then once the booster came along, you know, people were more versed on the most question I got when they got the booster was well, I have to get another booster. My question to them was, I'm not sure. But what I can say, if you stick to what the CDC recommend, and stay in contact with the CDC, they have websites that can send you information when it comes out. You know, just keeping people informed was the most important piece when it came down to the vaccines. But most people would say to me, “Well, which one you think I should take?” I had to be very honest with being a healthcare provider, “I cannot tell you which one to take.” So, they would say, “Well, which one did you have?” So I would be honest, and I would say “Pfizer, but it's your choice to decide which one is better fit for you.” And that's how I would keep the lines of communication with my patient, with my honest opinion as a nurse as a health care provider, that we were not allowed to tell our patient or to tell anyone which vaccine was better than the other.
Kit Heintzman 44:08
Do patients have specific questions or concerns about the mRNA vaccine as something that was new wish?
Charlene Harrod-Owuamana 44:18
And they would you know, and the only information again that I could, you know, share with them is the literature that we were given to give them to read about. Now the people who were apprehensive about getting their vaccine, I made sure that they got that paperwork so that they can read over, go home, talk to your friends, talk to your neighbors find out you know what your neighbors are doing. But for healthcare providers, we had to be bipartisan on which vaccine that they were going to get to give them the choice of What to get, and not for them to come back to us and say, “Well, you told me to get Moderna.” And this is what happened, you know, so it had to be the choice up to the patient, the customer, the consumer, on what vaccine they were getting, and we just give them the literature for the people who could not read, I read the literature to them to be sure that they would understand what they were giving.
Kit Heintzman 45:29
I love that. Thank you for doing that.
Charlene Harrod-Owuamana 45:31
Yes.
Kit Heintzman 45:34
How did you decide on Pfizer?
Charlene Harrod-Owuamana 45:36
Um, well as being a health care provider, our facility that we worked for, received certain vaccines, and pretty much it was whatever your facility received, because I got vaccine, I got vaccinated. Two months after the vaccine hit the market. It was mandatory, it was not mandatory. But it was given to us. As you know, you are on the front line. And the only way at this point that the CDC recognize that they had some containment with it was for us to get vaccinated. People who were not getting vaccinated, there were at work at first had to do a COVID test every week, to verify whether they were positive or negative. For me, I didn't feel the need to keep swabbing my nose every week, when I could get a vaccine, and it was a one shot once every 21 days or 30 days apart. And then that was it. And if I got symptoms, then I was gonna get tested. I didn't felt the need to stick that swab way up in my nose once a week. So, for me, it was a no brainer, let me just get this vaccine. But the most part of it was the reason behind it was a reason behind why I got it. Um, me again, being an African American, most African American people were apprehensive with the vaccine. "Oh, I have allergies. Oh, I have this. What would I do if I got the vaccine? Well, I was I had a latex allergy. I'm allergic to penicillin. I'm allergic to strawberries and a fruit with fuzz on it." So, a lot of people, African American descent are allergic to the same things that I'm allergic to add some more. So I say how else can I protect my future generation? I am a generation for generations. So I have great grand nieces. You know? So how can I protect my future generation of it and me be the first in the family to get it. So if I got the vaccine, and of course, the rumors, I didn't grow three eyeballs, or I didn't get sick drastically. I didn't get the vaccine and got COVID I'm still COVID Negative. I also got blood work drawn to see if I was ever exposed to COVID. And I wasn't and why some people have gotten COVID Other people have not gotten COVID other people who have had COVID twice and three times other people who have gotten vaccinated and still gotten COVID I don't know why. But if I was going to be the one who passed away from getting the vaccine, and to teach my family not to get it, I was willing to be that person. Because I had live 53 years so I was going to be that person that show the African American community that I can get vaccinated and that I was willing to put it all on the line for my future generation to be able to survive.
Kit Heintzman 49:14
Did you have conversations with family members about it?
Charlene Harrod-Owuamana 49:18
I did and I had a good conversation with myself and God about it. And it was like just go get it because if you don't and get back to nurses being the number one trust it. If you say to your patient, I am not vaccinated and I am telling you to get vaccinated then you can trust me. You know, so for patient or customer or consumer to know that I am vaccinated and boosted I am waiting to get my second booster. You know they are more they are more trusting that they can do something that I am doing And that, you know, they see me coming to work every day. They saw me get the vaccine and work that same day, you know. So, you know, it was well worth me getting the vaccine to be very trustworthy, to my patient, my residents, my consumers, my customers, it was well worth it was well worth it for me.
Kit Heintzman 50:24
How did your body react to vaccination?
Charlene Harrod-Owuamana 50:27
The first time I got vaccinated, it was challenging, I was weak, I was tired, I got a headache, I got diarrhea. You know, the diarrhea lasted for a day and a half. The headache lasted for two days. It wasn't like a migraine headache, but it was a headache that was there. So, when I took my second vaccine, I took Tylenol and a Benadryl before, I had no problems. When I got boosted, I took a Tylenol and Benadryl, I had no problem. Not that that will work for everybody, it just worked for me.
Kit Heintzman 51:12
I'd love to hear more about the place of compassion that you come from when talking with people who might choose ultimately not to be vaccinated.
Charlene Harrod-Owuamana 51:24
So, for me, for those people who are strongly against vaccinations, I have the strong sense of being that, you know, the more that I educate them, the more that the media talks about vaccination, the more we talk about people and death and dying, with or without the vaccine, I believe that the more people will come to grips that this vaccine will definitely work. Also, I believe that, you know, talking, so now, when we do test pooling in school, and the kids test pool come back positive, that's my opportunity to talk to the kid, when they come to do they have rapid to find out how they feel about COVID. And to educate them, because for me, educating a person before they become positive, and have them to understand what positive mean, helps them be able to understand what they're going through. Because not all people who are positive have symptoms. And I need for our kids to know, because in talking to these kids over the last month that I've been doing this, I find that most of the kids are upset because they think they're gonna die. Um, so for me, it's more important that I talk to them about what they feel first. Because then I can shed some light and give them some information that they're not getting, so that when they go home, they can explain to their parents, and it makes it much easier. I think that kids need to know what immune compromised means. I think that kids need to understand why is it so important to not share? Drinks, and food and chips. I even asked them. If you have a chip bag right now in your hand. And your friend asks for some, how are you going to give it to your friend? Would you let your friend dip in your chip bag? Or would you shake the chip out in your friend’s hand? Some of them say they would let their friend get their own because they don't want to touch it. Some of them will say they shake it in their hand. And I would be honest with them. I told them me when I was younger because I'm a 60s baby when I was younger, we all shared we even shared dirt. You know and we still here. I said times have changed now that we have COVID You guys aren't allowed to share and let people dip in your bag. If somebody dip in you put their hands in your bag to get chips. Them chips even now belong to them or you throw them in the trash. Plain and simple. So now the kids understand the kid don't understand. Don't Don't share your chips and don't let anybody dictate hands and your chip bag that's like opening the conversation to say hey everybody, just a Party Pack stick your hand in my chip bag. No but when I explained it to him like if somebody dip their hands and your chip bag you Then now and your chips are tainted. So now they understand that scenario. So now they're less likely to share their chips, because now they're like ill, you put your dirty hands and my chip bag now my chips dirty. So now they know the reason behind sharing those chips. So now their discussion is different, you know, they perceive this situation a whole lot different. Now they understand the whys, the house, the winds, the waves, those are not being explained to those kids earlier. It's just Oh, no, don't share. But then when I tell you why not to share, now you understand the reason behind it. And we talk about germs, germs, immune. And the reason the how, when, where and why is the best conversation to have with our future generation when you need them not to do something. And it all comes from being a pediatric nurse.
Kit Heintzman 56:09
What are some of the feelings and thoughts that kids have shared with you about the pandemic?
Charlene Harrod-Owuamana 56:15
One kid told, I said, "What do you know about COVID?" He says,"I don't want COVID to take home to my grandmother. If I'm positive, please tell me I don't want to go home. Um I'm gonna die if I get COVID? Um, my father died last week from COVID. Um, if I get COVID Will I die?" That is the most hurtful that is the most harmful question. The most complicated question that I have to answer when they asked me that, you know, because I can give them a definite answer as to whether them getting COVID. And if they're going to die? That's a question that I be honest with a kid about. I cannot tell you, if you get COVID, whether you're gonna die, what I can tell you is signs and symptoms. I can tell you what happens to a patient with an immune premise compromised. I can tell you, what happens if you have asthma, and you get COVID. But I can't tell you whether you're going to die if you get COVID. And I also tell them that I am sorry that I can't answer that question. And that question still today bothers me. Because me being an honest person to a patient and can't give them a definitive answer really bothers me. But what I do say to them is, have you had a cold before? Yes. Have you had the flu before? Yes. So, if you have had the flu before, COVID is a part of flu. So, if you have had the flu before, and you have gotten over the flu, the likelihood of you getting over COVID, it is true. I need you to do the same thing and have the same mindset you had when you had the flu. If there's somebody who said they don't they've never had the flu. Have you had a cold? Have you gotten over a cold? Yes. Then I also talked to patients and kids. Have you had a flu shot? Yes. Have you gotten over the flu? Have you had the flu this year? Since you had the flu shot? No. So why are you so apprehensive was getting the COVID vaccine, but you will take the flu shot? You know, so I compare and contrast other things that are close to COVID to present to them so that it will get them to think about you know, those other things.
Kit Heintzman 59:23
I'm curious what's it like talking to people so young about their mortality?
Charlene Harrod-Owuamana 59:29
For me as being a nurse, we are trained to talk to people no matter what their ages are. Some nurses aren't comfortable with talking to pediatric patients about that. But for me, I would rather than know, and know how I feel and give them information because for me knowledge is information and without knowledge and without information, then you don't know how to process it. And my importance of being a nurse is to help you process and to work through, you know, difficult situations.
Kit Heintzman 01:00:15
I would love a kind of rundown of how when COVID hit and you were working in the clinic, what kinds of changes happened in the sort of large-scale practice, you talked about sometimes seeing patients outside, were you at reduced capacity, what other kinds of things change?
Charlene Harrod-Owuamana 01:00:31
What change was, um, before, when patients would come into the clinic, and we would do their vitals or do their intake, we don't necessarily wear gloves. We wash our hands before the examination we wash our hands after now the COVID started, it was mandatory that we wear gloves with every patient, you know, just as with when AIDS came along, you know, things changed in health care a lot. Now, with COVID Coming along those changes, when in effect, and now are still in effect. When you do vitals blood pressure temperatures, you have to wear gloves with patience, you have to wash your hands before and after putting on gloves. You know, we have to wear masks when you're whenever you're in a healthcare facility. Yes, it's okay for you not the way of masks when you're out in the public. Yes, it's okay when you go into supermarkets now. And you don't wear masks. But no, it's not. Okay. When you come into a clinic or into a hospital, it's still mandatory that you wear a mask. So those are the changes that have changed outside of hospitals and medical institutions that inside medical institutions, you have to wear that PPE equipment, it's not up maybe or if you have to, as a health care provider, and I'm going into the schools to test them. The kids are not mandatory to wear masks. But we as healthcare professionals are mandatory to wear masks. We have just went back to win and N-95s back in schools due to the positivity rate going up. So now here in Baltimore, we do, we used to just wear the regular mask. Now we're told that we need to be fit tested. And we need to wear our N-95. And the numbers are going back up. For me, I knew the numbers never went anywhere anyway, the government sent out take home tests so people can test themselves at home. They were testing themselves at home. And if they were positive, they weren't notifying anybody. They were just positive. Whether they stayed in the house those 10 that five to 10 days or not. They were positive and they did whatever they wanted to do. And we didn't know. But for me as a healthcare provider, I've always worn my mask when outside of my home.
Kit Heintzman 01:03:03
How did you feel about the government sending out the at home tests, was it in January? It's quite recent.
Charlene Harrod-Owuamana 01:03:12
Right? For me, I was happy and still happy that the government sent those tests and instructions on how to know whether, they are positive. But what I do wish is that the government set up a way where they can confirm taking that test and finding out whether these folks were negative or positive. That's the only kickback me myself and my personal opinion about it is I wish they had something set up where they could take that test over telehealth and was able to accurately confirm what that test was and what it looked like.
Kit Heintzman 01:04:03
How did you feel about the schools reopening?
Charlene Harrod-Owuamana 01:04:07
For me, I think it was a disservice to close school. One because some of those patients, some of those kids, were not getting meals. Some of those kids homes didn't have electricity. Some of those kids, parents were not available to stay home to help them to get on a computer and work and pay bills. Some people were displaced because they couldn't not work and care for their kids to be home because the school system required parents to be available and they couldn't pay their bills. So now you had a lot of displaced people. You have people who have ran up. They have rent bills because they couldn't afford it. to stay home and educate their kids and work and pay bills, you know, and I fought the government, because over that time, while they were busy handing out all this money, they should have been handing it to these rental complexes and leasing offices to pay these people rent. So that now that it has uplifted, now, no, they are requiring these people to pay $10,000. Where are they going to get that kind of money from? Now they're displaced? Where are they going to live? We're gonna have more homeless people. Is the government worried about that about kids? Now going back to live on street because it's more and more people who can't afford to live where they are? So that part is what I'm concerned about now.
Kit Heintzman 01:05:54
What were some of the other safety precautions you took up in your day-to-day life at the beginning?
Charlene Harrod-Owuamana 01:05:59
At the beginning, you know, it was a lot of overeating, eating, because you're stressed out. It was tons and tons of patients that we had to take care of. Some of the people that were working in the ambulatory side now had to go into the hospital to help support the hospital workers with getting vital signs with helping feed patients with help passing out trays. So now, you know, you had healthcare workers, still in hospitals working, you had people who never worked now getting unemployment, and getting extra money. And here, you're still getting paid $20 an hour to do your job. And people who never worked a day in their life now average making $30 and $40 an hour, and you still out there struggling to make ends meet. And they're making ends meet and purchasing dumb stuff. Like purchasing cars and don't have license. I'm purchasing apartments and living in $2,000 month apartment and here you're living in an $800 apartment with one room, you know, so that bothered me a lot in the beginning when COVID hit, you know, certain jobs, were giving people bonuses for working. During during the um COVID. We as nurses never got paid for working. Extra bonus, thank you nothing, but we still maintain our commitment to people. It was nurses that were out there on the frontline that were dying. You know, who was getting COVID, who didn't know they had immune compromised and were dying from trying to care for someone else's family. You have negativity and people out here saying, “Well, you took on that job to be a nurse. So why are you worried?” You know, so it was the negative comments from people. It was the stress from being overworked. It was the stress just for taking care of a patient that you could not save the day. You know, you go to work, and you might have had a death, maybe once in two months. Now you have in about 10 a day. You know, where did that take our mindset? Are we still traumatized? Yes. Are we still out on the frontline? Yes. Do you think the frontline ever calm down? No. for nurses and never calm down for nurses? Yes, it's still just as detrimental as it was when it first came up. But it's the news media making that a priority? No, because now they're covering some other news. But yes, for me as a healthcare provider for me as a nurse is still evident and it still is vulnerable people are as of when it first started.
Kit Heintzman 01:08:58
Do you have coping strategies for when you lose a patient?
Charlene Harrod-Owuamana 01:09:03
Some days I lose it. Some days I go, I cry, you know, crying is nothing wrong with crying. It's nothing wrong with sharing your emotions is nothing wrong with your spiritual emotions. You know, I want people to know it's nothing wrong with crying. Whether you're male or female, you know, I am so happy that I am doing this. But what I want people to know that it is nothing wrong with crying. Please cry, please spiritually. Take care of yourself. Please know that death, grief. Emotions are something that you have to go through and your lifetime. Please don't take death is a death sentence. You know, my mom died when I was 15 not only my mom, my little brother, we had a house fire. And my mom and my younger brother died and people like, Oh, I'm so sorry. And I'm like, you know Oh, that was a journey that God placed me on. That was a journey that God has helped me to live from 15 to 55. Now, that, you know, I look at death differently than most people, you know, I look at death now as a celebration, spiritually vulnerable, I am vulnerable, you know, to when a patient of mines die, I feel the same way I felt when my mom died. And it's okay. It's okay not to be okay. It really is. And it's, it's, it's an as you can see, I light up like, you know, it is okay. And I want people to know when people say it's gonna be okay. It really truly is gonna be okay. It's just, you know, your mindset. You know, it's just spiritually, mentally emotionally talking to the right people to help you overcome this, you know, not seeking help is the worst thing that you can do during these times, or anytime when death is involved.
Kit Heintzman 01:11:09
I'd love to hear more about nurses and mental health and your sort of longer awareness of the toll that working in health care can have on nurses and then how that got ramped up during the pandemic.
Charlene Harrod-Owuamana 01:11:25
Okay, so already in place, most employers always had an employee assistance program, where you can call and you get x amount of free visits, where you can talk to, they made it accessible. Some people don't like to talk to psychiatrists and psychologists because they don't want to be perceived as crazy. A lot in healthcare, some nurses and some health care professionals don't like to work alongside someone who is depressed because they think your atomic time bomb. Now that COVID has happened, we have all experienced some type of mental depression or mental problems. So now people view it different you know, now all of that stigma about being depressed or having a mental breakdown is a new norm. You know, so now people perceive it a lot different. If I come across a person who don't perceive it, I'm comfortable. I have a conversation with them. Like, what does it look like day to day? When? If you tell me your stress, stress is a part of mental health. Let's get let's let's get it let's see it for what it is, you know, some people like, “Oh, I've never been depressed.” Have you ever been stressed out? Heard you say you were stressed yesterday? You know, that's a part of mental health. You know, how can we bring ourselves back? You know, so employers have made days like, oh, today is ice cream day, we're gonna pass out ice cream to everybody. Today is the coffee day Dunkin Donuts is coming here to provide free coffee for the staff. It's not a full cup of coffee, it's a 12 ounce cup of coffee. You know, today, we're going to do snowballs, we're going to provide snowballs for you today. You know, those little things help. When it comes down to health care providers. Over the pandemic, it was restaurants providing food for us, that made us happy, we didn't have to worry about going out to lunch. We didn't have restaurants weren't open. We had to cook food bring food in we didn't have enough food to go around the feed people at home and they have free fruits and vegetables and things like that for people. So all of that was helping, you know, it made people accountable for each other the way it used to be, you know, getting back into knowing who your neighbors are, making sure your neighbors have things that eat making sure your neighbor say making sure your your neighbor take time for self care. All of that was wonderful. You know, so for me, that is what mental health means to me to acknowledge what part of mental health you are going through pain, stress being burned out. All of that is mental health. And we need to pay attention to know that it is which means we've all had that mental breakdown at one given time in our lives.
Kit Heintzman 01:14:44
Thinking of your social life outside of work, what are some of the things that you maybe gave up because of the pandemic and maybe at this point have gone back to but??
Charlene Harrod-Owuamana 01:14:56
Right, so me and my friends we made a pact fact that once a month, we will either go to breakfast, lunch, or dinner, or we will do something together on a Saturday or something. And all of that came to a screeching halt. Everything was computer base, we would do zooms, we would do our little girls day out over zoom. You know, we weren't together. But we were together, we could see our facial expressions. If we had a bad day, we could zoom each other, we could FaceTime each other Oh, I had a rough day to day. What do you think about this? Or How are you coping with this or, and it still was that communication. It just wasn't that touchy feely communication time, and we made it through. And then when we could get together, we were so excited that we were all together, that we sat outside for lunch, still sat outside still came in with our mask on and took it down to eat. So, you know, we still think of that, you know, we still think of that time where we still have to protect ourselves, we have kids, we don't know whether one person is going around someone else, you know, I had a friend because I do a radio show. The radio show people at first everybody was contained to where they would go and what be more mindful of who they're going around. So, the people at the radio station wind up going to a family function, then their uncle got COVID, and then they got COVID. So, then we couldn't go into the station anymore. And the station had to be thoroughly cleaned and things had to be clean. And then you know, now people are back to being mindful, you will be very, very, very surprised at where your friends would say, you know, I'd be very careful about who I go around and where I go now. You know, people are more hyper vigilant with what they're doing and where they're going, and who they are being around nowadays, then, you know, before the pandemic.
Kit Heintzman 01:17:08
What do you think that vigilance does?
Charlene Harrod-Owuamana 01:17:11
What does what do I think what ?
Kit Heintzman 01:17:13
That kind of hyper vigilance is doing?
Charlene Harrod-Owuamana 01:17:16
What I think is some people are really, really taking heed to our guidelines, you know, when we were told to stay home, and you could only be out because you medical professionals, that took a great toll on a lot of people, you know, you started hearing about abuse a lot, and you started hearing about crazy things was happening in certain states and homes. And, you know, that was almost a given for health care provider to know that those things were going to be taking place. Because sometimes being out of the house was some people safe haven. And when that safe haven was taken away, it kind of took people by surprise. So, you know, having vigilance about where you're going, the people you're around the crowds that you're in it, it is really keeping a lot of us safe now.
Kit Heintzman 01:18:18
Has your relationship to touch changed over the course of the pandemic?
Charlene Harrod-Owuamana 01:18:22
Really not because me as a nurse, I still know patients, residents customers still need the the feeling of touch, you know, as being a health care provider. I wouldn't say that I feel like I'm in a different class. But I would say that my patients pin in on what's going on with them still need that touch. And you know, I still practice safely, because that's a part of my training. But the form of touch, whether it be touched with a glove on or touch with just my hand, you know, I still need to give my patient what they need and protect myself and my patient, client customer, because everybody has a different name, you know, family friends.
Kit Heintzman 01:19:21
Were you able to maintain contact with family during the pandemic?
Charlene Harrod-Owuamana 01:19:25
Absolutely. Um, I had an aunt who does have immune compromised who couldn't not go to the market. So, me and my cousins would take turns taking them groceries we would leave it out on the steps, haul them sit in a car, tell them come get the groceries carry the groceries and so we almost had to go out and buy a storage bin to put outside their house to tell them not to touch the bag. We will leave the bag open they will get the groceries out of the bin and then take the groceries in the house. So, it was a lot of you know how can we make your life safer, we will tell them go out on the back porch don't come out on the front porch, you know, because you still need that vitamin D, you still need that ray of sunshine on you. You know, just because you can't go out don't mean you can open the window when the sunshine come in, you know, things of that nature. So, we had to teach people how to get their vitamins, other ways than just eating and drinking orange juice, oranges, bananas, and things of that nature, how you just get that old, good old sun. And to explain to them that you get sun in the wintertime too. It's not those rays, that's gonna give you skin cancer, but you can still get sun during the winter months and things of that nature. So, we did a lot of education.
Kit Heintzman 01:20:48
What is the word health mean to you?
Charlene Harrod-Owuamana 01:20:51
So, the word health means not only your general health, but your emotional, spiritual, physical. It just remains it means all around health to me. It's not just your day to day function. It's everything. To me healthcare is not just what most people think is. Are you feeling good today? How's your blood pressure today? No, it's everything. It's just the whole continuum.
Kit Heintzman 01:21:25
What are some of the things that you'd like for your own health and the health of people in your life?
Charlene Harrod-Owuamana 01:21:30
Um, what I would like for health is for people to spend more time thinking about togetherness, spending more time learning about themselves and their special gift that they have been given to give to others. I have always, even as a child, my mom always taught me to give more to get more back. That's what I really enjoy given more, because I always get more back.
Kit Heintzman 01:22:02
Curious 2020, the President has had so much going on on top of the pandemic, what are some of the other big issues that have been on your mind over the last few years.
Charlene Harrod-Owuamana 01:22:15
And what's been on my mind over the last three years is our urgency for our future generation to know that we really do care about them. The urgency that I try to stress the young people that education is so important, and don't take it lightly. What I try to express to young adults is, you know, be mindful of where you're going, what you're doing and who you are around. You know, in Baltimore City, we have a murder rate that is so high, you know, not only do we have to worry about COVID pandemics and epidemics, now we have to worry about community involvement and murders. And, you know, it's just so much that we have to worry about now, that it's just not only our health that we have to worry about, we have to worry about everything and everything around us. So, for me, it's not just COVID the bigger issues such as voting, voting rights, you know, so much going on in the news is just so much all around, that we have to be, you know, mindful of, and that is concerning. So, it's just all of that to take into consideration.
Kit Heintzman 01:23:44
Sometimes when I try and think about which, like what historian is watching this and some version of the future, I like to one of them. I like to think of it as one who finds this world very weird. Because their world is so different. Explain to an alien, which is someone 50 years in the future that person's alien. What it's like to live in a city with so much murder, and how that works you.
Charlene Harrod-Owuamana 01:24:14
So, I've been in Baltimore all my life. Um, some of the murders that happen in our city I hear about and some I don't. You ride through our city, you see memorials, whether it be balloons or whether it be alcohol bottles all over the street corners and step corners, and, you know, me as a child being raised and the projects, which is a large building with a lot of people in one area. And I stress that to the kids that I meet, you know, they see me as a healthcare professional. They see me as a person that they are Sin. I grew up in a family that was wealthy, a family that did a lot. You know, I tell them, I'm just like you, I was born and raised, broke, but full of love, full of spiritual guidance full of a community building, nurturing, training me telling me what's good for me and what's not good for me. You know, that's what worked for me. That's what got me out of those areas, you know, and 2017, I started writing books. And now I'm like, at my 15th book, and I'm gonna share this with you. I wrote a chapter in the anthology called my mom's death saved my life. My family asked me, “Why would I write something like that?” I explained to them, that when I go back in my old neighborhood, and I see my friends, from when I was younger, they're either dead, strung out on drugs, and some of us are professionals. Not only healthcare professionals, lawyers, doctors, or what have you. But some of us go back in that neighborhood, and we see our friends, and I cry, you know, me and one of my best friends made a pact that we were going to be this nurse, Doctor team. And we was going to do this. And we was going to do that, and she strung out on drugs. And when she see me, she tried to avoid me. One day, I caught her. And I said to her, I said, “Please don't avoid me. But if you need help, I'm here.” You know, she started crying, I started crying, you know, it's about going back in those communities, reaching back out to your friends and your family, animals, communities, and trying to get them to work in health care facilities in those communities, because they know what they need in that community. And if you don't get yourself together to go work in your community, then your community is going to continue to go down, where I can help you get that community back up and running. Let's train you, let's send you to classes and education. And yes, college is not for everybody. And I understand that. But you can take a training course that can get you where you can go, you can actually take what you have learned throughout your life and get a job. You can be an attic, get yourself together and be a counselor who helped other people get themselves together because you've been through it. You know, what they've been through me as a nurse cannot tell an addict what they have been through because I have no experience. You as an addict can get help. And go out and start to minister start to treat, start to help your fellow worker, your fellow. Get high partner get help. And they know truly you have been through it. You know what you saw what you did? You know how you feel now you can show them the joy of how you feel now and know that it's the best now for me being born and raised in Baltimore, and went and took a contract on the West Coast and San Francisco. Not in LA Where's high crime? Right, right. Not in Oakland, where's high crime Laurie? But in San Francisco, and San Mateo, San Jose, where they are murderers, but not as much as here. The whole time that I was in San Francisco, I never saw a helicopter.
Charlene Harrod-Owuamana 01:28:40
I saw planes, but I never saw helicopter him Baltimore's like you can see helicopter 15 times a day. You know. So there is a difference in the area. And I'm quite sure in California and Oakland. I'm quite sure they have helicopters, but I was in Oakland. I never saw a helicopter when I was in Oakland. But if I was back home in Baltimore, I would have seen helicopters many times, if not heard one, you know. So I think that I am. I hate to hear that term that. You know, it's something you used to. Because when I lived in the inner city, I saw helicopter more. When I moved out to the county. I saw helicopters less. When I went to city and I saw a helicopter. I was like, What in the world is that noise? Because being out in the county, I wasn't used to hearing it. But people who are in the city are so used to hearing it, that it's a noise that they don't they don't even pay attention to. So you know, what I kind of figured out was that, you know, being in certain environments. It's not that it's a norm. It's just that your brain I mean, as you said, that norm, so it's not a norm because it's not normal, but the brain become less conscious to to extra noise.
Kit Heintzman 01:30:15
I'm curious what does safety mean to you?
Charlene Harrod-Owuamana 01:30:19
Safety means security. Safety means being informed safety mean education. Safety means safe safety means that you have someone who has your best interest or not have your best interests have a way to point you in the right direction to get it. So that's what safety means to me.
Kit Heintzman 01:30:48
You've mentioned education a few times, I'd love to hear a bit about what you think is so important about education and why you want young people especially to have it.
Charlene Harrod-Owuamana 01:30:59
So, when I was younger, and coming out of high school, a lot of people when I was younger, stressed to me that I needed to get a job, and that it was so important that I graduated from high school. So that's what was important to my generation when we were coming up. Nowadays, for the generations that are coming behind us and the millennials, a high school graduation, is not going to get them where they need to be. Not even an associate degree is going to get them where they want to be, it will get you somewhere, but it will not get you where you want to be making 90 and six and seven figures. Now, don't get me wrong, you may be lucky. And God had a plan to make you a billionaire, or had a plan to make you come up with some type of device that would help us out in America, such as the cell phones and cameras and making this able to be you know, produced. But not everybody is going to have that opportunity. Not everybody. Not everybody is going to be able to not everybody is going to be able to be rich, not everybody is going to have that opportunity. Not everybody is college material. But education is so important that our fire chief stated. I could train anybody to be a firefighter, but they have to have the willing to be educated. You know, to learn a new task doesn't take a lot, you just have to be willing to be educated. So when the fire chief said that, you know, that that gave me the hope that our city have hope that we envy other cities that have a high murder rate, that if we put Education First, we can get rid of this. But first and foremost, there are some things that need to happen first. And if it costs for us to have the national guards on our corners, then so be it, you know, but there should be nothing that could not protect us to make us safe, make us feel healthy, and make us feel like education cannot improve our environment. You know, to go a little further, what I've heard is your health, your wealth. And your safety depends on your zip code, and your city that you live in, no matter what city you live in. It's across the board, your zip code, where you live, and your health. All depends on how long you're gonna live. And it says it's studies that have been done that have proved this, you know, so that's why I stress to young people that education is so important. And when I see a kid play or I see a class that is out of control, it would behoove me to say something to that teacher and give her a little, just a little bit on how you can control your situation easily by turning off a light and let your kids sleep for 10 minutes in class.
Kit Heintzman 01:35:03
Have you had much of a chance to mentor other nurses?
Charlene Harrod-Owuamana 01:35:07
Yes, I was a part of an organization called Black Nurses Rock. I was the president, I have 52 nurses under me, which range from LPNs nursing students, all we have to nurses with PhDs that when we were in that organization, your title, your certification did not matter. But going out in the community, and advocating for health care, and given people in the community information was so important. And that's what makes me get up every day and do what I do. And I'm ever so sad that that chapter, had close. But they do have other chapters. And they do have a chapter here in Baltimore now. But I felt like I needed to do more on my own and get out and get the word out. So I started a program called Nurses Hive that go into schools and go into community after school programs that educate kids on what was taught to me to find a job. But what now I teach to them is to find a career. It is so important that our youth find careers and not a job, because going to a job and hating it every day is sad, but going to do a career that you're proud of every day, just make the light bulb shine bright on you.
Kit Heintzman 01:36:50
I would be so grateful if you shared more about credentialism and hierarchies in medicine, given what you just said about black nurses rock, not emphasizing which letters you have.
Charlene Harrod-Owuamana 01:37:05
Right. So, what happens is, what happens that I feel is when some people get education, and they get educated, they feel and it's not for all, it's just some individuals feel like if I have a master's degree, and you don't have a degree, I don't even want to be bothered with you. And you can tell me nothing because I have a master's degree. Well, I like to tell you, if you have a master's degree, and you come into my hospital sick, you don't know about medicine, you have a master's degree, and biology, all you know about pretty much is cells and how they replicate. But if you have high blood pressure, do you know that stress can take you to have a stroke? Do you know signs and symptoms of a stroke? No. But guess who do? I do? So, what I try to stress to people is if you know biology, and I am brand new, and I don't know what a cell is, yes, you would that master's degree can help me. But if you sick and you have hypertension, and you have not been trained on medication, and how I can help you and when I need to call the doctor to either get a medication to you or take a medication away from you, then you have a master's degree, me with an associate degree does not correspond because me as Associate Degree nurse can care for you in a health care facility without a master's degree. So, when people come to me about their letters behind their name, and some people really do truly have the whole alphabet behind their name. But when you come to me and you sick, and I am a LPN nurse, I do know how to care for you, how to assess you by looking at you, and how to go to the doctor and advocate for you and your healthcare and what you need and what I think you should not have. And also talk it out with that doctor to figure out why that doctor feel that you need x, y and z. So, when it comes down to having letters behind your name, I really get into it with people to let them know Yes, I am so happy that you're educated. Because when I need to know what's wrong and what's going on with a cell, I'm coming to you, but when I also need to put on my nursing hat and care for you and be sure that I'm giving you the right amount of fluids, the right medication, you know the right health care that you need, appointing you to the right doctor, the right specialist, that's going to help you come out with a good Read health score, then yes, we can communicate and not talk about letters behind your name.
Kit Heintzman 01:40:09
How do you find your relationship with doctors, by which I mean like MDs,
Charlene Harrod-Owuamana 01:40:14
With doctors, you know, each doctor, each profession, each specialty, each doctor has have a different personality. And being a nurse, you have to know your place. And you have to actually almost know your doctors you're talking to and working with. Yeah, there are some doctors who have made me mad. There are some doctors who have not listened to me. And there are some doctors who have came back to me and thanked me for my services and my decisions and my input on a patient care or diagnosis. But you know, what really, really makes it great when it comes to health care is a team that can work together. Because there's no I in team. So I do make sure I say that to a doctor or healthcare provider that's being mean or out of character. I do say there's no I in team, which means we have to care for this patient together.
Kit Heintzman 01:41:28
Would you tell me about a memory from the last two years that you think will stick with you for quite a while?
Charlene Harrod-Owuamana 01:41:38
Okay, I'm going back to California. I don't know California, California has a meaning for me. Let me tell you about this meaning. When my mom died, I was so depressed, I had to figure out a way how I could get as a child, you know, children have imagination. So, I had to figure out a way that I could deal with my mom's death. So out of the clear blue, I came up with the saying, my mom and my younger brother moved to California. And since they was in California, I couldn't see them every day. So, I was able to cope with their death a little bit. Little did I know 54 years later, I will be working in California. And when that light bulb came on that 38 years ago, I told myself this to get over my mom's death. And now I am in California. So, California really means a lot to me, because it was my safe haven until I realized that I needed to deal with death, grief, and everything. So bad. For instance, in California, a kid came to get his vaccine. And he was so petrified he laid in the floor because he did not want to get his shot. His mother's dragging him the nurse over there, they were going to make him get the shot no matter what. Because his mother said he couldn't go home if he didn't get it. So, I stopped my line. I went over there, I looked at him. I said, Now why are you laying in his floor blocking me from walking over here to the door to get some fresh air? He said he wanted me to get a shot and I don't want it. I said, “Okay, get up. Let's come walk with me. We're going out here. And we're gonna talk about this”. So, I talked to him. And what I found out was what a lot of kids, you know, think if I get COVID, I'm gonna die. Because this is what he told me. My mom said, If I don't get this vaccine, I'm going to die. Now how plants equivalent dying with vaccine? I don't know. But anyway, we went out there to have a conversation about it. So, I asked him, “Well, what is the worst part of getting a shot?” And he said, “it hurts.” I said, so if I tell you, “I'm gonna give you a vaccine and it's not going to hurt. Are you willing to go back in here and sit at my desk at my chair and take this vaccine?” He said, “Um, how about I think about it.” I said, Well, that's fine. But you only have two minutes to think about it. Because your mom says that you're gonna have to get it anyway. He said, “Well, okay, if I go back to your chair and get this vaccine, is it gonna hurt?” I say “yes, it's a possibility. But I give pediatric shots a lot. And I've been given him for 12 years. So how does that make you feel?” He said, “Well, that makes me feel a lot better.” I said, “Okay, so we're gonna walk back in here. I say you're helping school.” He said “yes, but it's not my turn.” To be a helpless Ma, my turn next month I said, “Okay, so the day is your turn to be a helper, and you have to help me. So when we get back over here and put a glove on your hand and I need you to clean your arm, so I can give you this vaccine, that's not going to hurt.” So he said, “Okay,” so we walks on and I'll give him the back. I give him the, the glove. He rubbed his arm. I say it's a clean, he said, Yeah, I said, “No, it's not clean at arm I need to clean arm to work with now so he's rubbing rubber.” I say it's a clean. He said, No, I say okay, so get the rubbing, rubbing, rubbing, rubbing. I say Okay, now we're gonna let it dry. I say, “Okay, I'm gonna give it a shot”. So, I get the needle, and I get ready to give it to him. He said, “No, no, no.” I said, “Well, we made a deal outside, that if you came back to my chair, that I was gonna give you a vaccine, this needle here. And you see is clear, right? It's not cloudy. So when it's clear, it's not gonna hurt. It's just like water.” He said, “Okay.” I said, he said no way. I say yes way. He said no way. It didn't even hurt. He said, “Mom, I got the shot. It didn't even hurt.” I say “excuse me, I didn't give you a shot, I gave you a vaccine, and it didn't hurt.” And what I did not know is that he was an autistic kid too. So that just goes to show that if you communicate with them, use kids and educate them.
Charlene Harrod-Owuamana 01:46:38
Then your job is done. You know, and I believe that that is what it's going to take for us to vaccine our country is education. And the more education that we give to our community, our friends, our family, our consumer, our customer, our Pez patients, our residents, even our enemies, then we won't be able to vaccinate our country, city, whatever, nation unless we do that. And the last thing I like to say is my kids that I talked to, I asked them if they knew who the World Health Organization was. And they told me no. I said, so who do you know, they say the CDC? I said, Okay, what I want you to do when you leave here today is I want you to look up the World Health Organization, their acronym is who look them up. And the next time you see me, tell me what you learn. You know, that means that if that kid come back to me, I educated them to go look something up. And I'm gonna see if they come back to me and tell me what, who is. And it's just the mere education that we give to people to look things up and to read things. Because when I was younger, my father used to let us read the comics and the newspaper, even though we couldn't read, we would still look at the pictures and tell what the pictures don't. So I believe if we educate our country, our community abroad, I think that we can overcome this epidemic pandemic that we're in now.
Kit Heintzman 01:48:30
How are you feeling about the immediate future?
Charlene Harrod-Owuamana 01:48:34
I feel like some little person that I have had contact with will be able to care, a lot of issues that's going on in our country and other countries, and particularly know enough about our brain so that we can use more than 2% of our brain that we're currently using right now. That is my take on this world that some little genius is going to come up with what we can use more of our brains and be able to reduce the amount of pandemics and epidemics that we go through. And like
Kit Heintzman 01:49:21
What are some of your hopes for a longer-term future?
Charlene Harrod-Owuamana 01:49:24
Some of my hopes is that my legacy live on and to the next century, to provide a lot of education and to let people know that I really truly enjoy being a nurse and being an advocate for people all over the country when it comes from the East Coast and to go work for West Coast as far as you can go. It's just amazing at what we can do in life and one person if we just add advocate for our country.
Kit Heintzman 01:50:06
I'm coming to the end of my questions and the last ones are a bit funny. I'd like to ask so you know that there's been all of this biomedical research happening because you've been teaching it. I wonder wondering what you think people in the humanities and social sciences, so people who are doing literature degrees in sociology and political science? What kinds of things should we be asking about the human side of the pandemic?
Charlene Harrod-Owuamana 01:50:35
Well, I learned today, I'm one of the kids in a school had gotten COVID probably about nine months ago. Um, yesterday, he at the school, was doing an activity that was fun for the kids at the school. He went home, he told his mom that his chest hurt. When he got home, they took him to the emergency room, and it turned out that he had myocarditis. So that's inflammation around the heart. Now, a lot of people have been hearing about people who have gotten a vaccine and have had COVID gotten a vaccine and have been diagnosed with myocarditis, which is inflammation around the heart. This child had gotten myocarditis, and that's what they diagnosed him with. But he was not vaccinated. The doctors gave him the immunoglobulin medication, and vaccinated him. And the parents were told that most people who have gotten COVID and did not get vaccinated have been coming up with myocarditis. So, me, I am going to do some more investigation and research to educate myself about that. And that's why I feel so strongly that I need to get my book out a little bit more, I'm going to send you a picture of my book cover. So that you can see what I've written about. And the other thing is, I also in the back of my book, thank a couple of organizations in California, for allowing me to vaccinate their employees as well. My thought process was to send the CEO of Tesla email to see if he could purchase some of my books to send to some of the kids in California because that's where my inspiration came from to do that, but, but I'm trying to research on who I could send an email to, and I just have not come up with it yet. But I am going to come up with it to x some of those companies like Facebook, Google Tesslar spoton, which is a part of Safeway where I was vaccinating adults in California, to see if they can purchase my book to distribute, you know, to those kids in California, who got the vaccine because that's where my inspiration came from, to write this book. And I did put them on the back of my book to thank them Fleur, what took place in California, but I haven't figured out a way to distribute it. But by the grace of God, he's going to help me figure out how to distribute that book in California.
Kit Heintzman 01:54:10
How do you think historians might remember this moment?
Charlene Harrod-Owuamana 01:54:15
Well, for me, I'm hoping that historians would remember that it took a lot of folks to collaborate together to start the process of healing the country, the nation, from this pandemic, when you know, the swine flu came out. That was a pandemic as well. And the swine flu it's no careful what but it was under control. And that is the same series of thought process that I'm hoping that history Oracle will be through, talked about forever that this pandemic was a another successful. Another successful issue that came up that was contained.
Kit Heintzman 01:55:25
We see sort of over and over again, that history ends up with blind spots. If you can use this as a chance to talk to historians of the future, what do you want to tell them, can't be forgotten about this moment? Like, yeah,
Charlene Harrod-Owuamana 01:55:43
What I would tell them that I would like for historically, to be placed on a map that it takes honesty, to give people information. And it takes a better person to admit when they are wrong. And never, ever take lightly the conversation that you have with people, for people to believe in you. Honesty, trust. And being very, very, and having a lot of integrity is so important. When it comes down to health, wealth, spiritual commitment, emotionally, physically, it takes a village to raise people, it takes a country and a nation to work together to come up with a common cure, or cars, to get to the root, and just not man to make the decision on what happens in the future, to contain anything that comes upon us as humans.
Kit Heintzman 01:57:07
I want to thank you so much for the generosity of your time and the beauty of your answers. Those are all of the questions I know how to ask at the moment, but I want to open some space. So if there's anything you'd like to share that my questions haven't made room for, please take them now.
Charlene Harrod-Owuamana 01:57:27
I would just like for the CDC, the president, governors, mayors of cities, social workers, police, all government officials to know that it really takes honesty. And it really takes a big person, if you are wrong, to make it right. People in America, really enjoy hearing sympathy, people being empathetic people really truly caring and given forth. The strength the safekeeping, the right emotions, and to know it's okay to cry. It's okay to pray to whatever God or whatever person you pray to, it's okay. Because at the end of the day, we're still people. We are in the visual, we depend on you guys expertise, to help us take in the information, to relate to information to be able to equip each individual with what we need, but also take a strong government to accept criticism from people who are living out that issue with that pandemic or or epidemic that's going on. Please be mindful that people have that people have empathy and sympathy within themselves and their country. You know, it takes a lot for any individual to sustain death, stress. And for health care workers. We are grateful to be able to assist a country, a nation with health care, but please be willing to also think of us when you think of supporting, acknowledging and giving please think of us as the front But one people not to forget those police officers, manufacturers, mail people, truck drivers, distributors, who did not have the luxury of staying home and caring for their families, and had to go out and put our lives on the line for someone else life, whether they were committed to thank us for it or not, whether they felt like we took this job, that we should be doing it and that they could say whatever they wanted to say to us, and it was okay. Because it wasn't, we do what we do on a daily basis, because that's what we feel in our heart should have been done. And that's what we will always feel in our heart. That should happen. So what I like to tell them is please don't forget those people that were really on the front line, and then just not consist of doctors and nurses. And CNAs. It was radiation techs. It was it was the whole team. It took a team of us to get where we are today. I don't want the government, the CDC, our health care world people to think that it was all them who got us here. It was a team of us. And I want to think of us as us that got us here. And that's what I want to portray.
Kit Heintzman 02:01:41
Thank you so much.
Charlene Harrod-Owuamana 02:01:42
You're welcome.
This item was submitted on June 15, 2022 by [anonymous user] using the form “Upload” on the site “Oral Histories”: https://covid-19archive.org/s/oralhistory
Click here to view the collected data.