Item
Brian Ghafari-Naraghi Oral History, 2022/05/18
Title (Dublin Core)
Brian Ghafari-Naraghi Oral History, 2022/05/18
Description (Dublin Core)
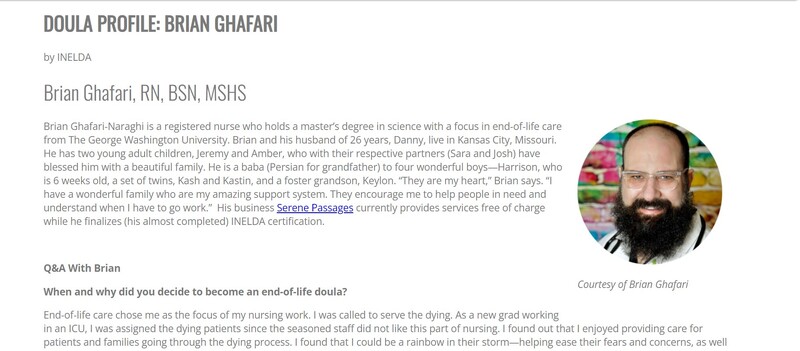
Self Description: ". I am a registered nurse with over 25 years of experience. I hold a Master's in the Life Care, a bachelor's in nursing and associate nursing. I have completed my doula training...end of life doula training. I am do some grief counseling that I was trained for. And a little bit of this, a little bit of that in the medical field. Before my previous job, I was working with ALS patients and Case Manager. Now I'm going to be doing clinical research. Now I'm going to be doing clinical research on psychedelics that pays the bills, so that I could do my doula stuff."
Some of the things we discussed include:
Growing up American Baptist
Coming of age during the AIDS crisis as a gay man; stigma
Relationship with mother; mother dying ~twenty years ago; taking care of siblings
Marriage, relationship with mother in law, children
Working and volunteering in many parts of the medical field: home health aid, registered nurse, death doula, grieving counselor, street medicine, hospice director
Lost work during the pandemic
Birth of grandson during COVID
Connecting with dying clients, listening to life stories
Creating a death plan with clients, education, making your wishes known
Bodily/patient autonomy; medical advocacy
Pain management
Comparing quality and quantity of life
Dying with dignity
Media representations of death
Accessible teaching style, target 5th grade level
Emotional labor and emotional regulation; boundaries
Comfort with silence; being present
Humor, tough love, reassurance, and honesty
Patients needing touch during the pandemic
Authority and power in healthcare infrastructure
Mementos, legacy projects, respecting the dead’s wishes
Saying goodbye
Nursing homes
A nurse-friend dying of COVID
Preparing to host a Death Cafe
Other references: Paul Tschudi (The George Washington University), oncologist Dr. Jesse Roberts, hospice and palliative care physician Dr. Maureen Dudgeon, The Rockettes, Roe v. Wade, Disney Princess Hugs, Aerosmith, Warren Hanson’s The Next Place (1997), survivor’s guilt, Margaret Edson’s Wit (1995), Little Miss Sunshine (TV-series), Mitch Albon’s Five People You Meet in Heaven (2003), Jimmy Buffett’s Cheeseburger in Paradise (1978), Swedish Death Cleaning, active shooter training, Gen X, Millennials, Dasia Taylor’s invention of color-changing sutures
Growing up American Baptist
Coming of age during the AIDS crisis as a gay man; stigma
Relationship with mother; mother dying ~twenty years ago; taking care of siblings
Marriage, relationship with mother in law, children
Working and volunteering in many parts of the medical field: home health aid, registered nurse, death doula, grieving counselor, street medicine, hospice director
Lost work during the pandemic
Birth of grandson during COVID
Connecting with dying clients, listening to life stories
Creating a death plan with clients, education, making your wishes known
Bodily/patient autonomy; medical advocacy
Pain management
Comparing quality and quantity of life
Dying with dignity
Media representations of death
Accessible teaching style, target 5th grade level
Emotional labor and emotional regulation; boundaries
Comfort with silence; being present
Humor, tough love, reassurance, and honesty
Patients needing touch during the pandemic
Authority and power in healthcare infrastructure
Mementos, legacy projects, respecting the dead’s wishes
Saying goodbye
Nursing homes
A nurse-friend dying of COVID
Preparing to host a Death Cafe
Other references: Paul Tschudi (The George Washington University), oncologist Dr. Jesse Roberts, hospice and palliative care physician Dr. Maureen Dudgeon, The Rockettes, Roe v. Wade, Disney Princess Hugs, Aerosmith, Warren Hanson’s The Next Place (1997), survivor’s guilt, Margaret Edson’s Wit (1995), Little Miss Sunshine (TV-series), Mitch Albon’s Five People You Meet in Heaven (2003), Jimmy Buffett’s Cheeseburger in Paradise (1978), Swedish Death Cleaning, active shooter training, Gen X, Millennials, Dasia Taylor’s invention of color-changing sutures
Recording Date (Dublin Core)
May 18, 2022
Creator (Dublin Core)
Kit Heintzman
Brian Ghafari-Naraghi
Contributor (Dublin Core)
Kit Heintzman
Link (Bibliographic Ontology)
Controlled Vocabulary (Dublin Core)
English
Public Health & Hospitals
English
Community Service
English
Emotion
English
Healthcare
English
Gender & Sexuality
English
Health & Wellness
Curator's Tags (Omeka Classic)
Facetime
funeral
training
Contributor's Tags (a true folksonomy) (Friend of a Friend)
abortion
advocate
AIDS
ALS
Alzheimers
Baptist
boundaries
cancer
Buddhist
homebody
hospice
guns
hospital
celebrations
cremation
crying
doula
educator
touch
theology
suicide
spirituality
psychedelics
ER
parenthood
queer
resilience
sacred
pain
nurse
NICU
needles
family
music
Missouri
meditation
marriage
Kansas City
joy
introvert
hugs
grief
funeral
gay
Collection (Dublin Core)
LGBTQ+
Deathways
Curatorial Notes (Dublin Core)
From 03/2020 until 11/2022 we redacted information revealing covid and vaccination status of those other than the contributor but discontinued that practice on 11/14/2022. This note was bulk added to any item with the word "redacted" or "redact" in curatorial notes, so may not apply to all on which it appears. Erin Craft 12/29/2022
Date Submitted (Dublin Core)
05/18/2022
Date Modified (Dublin Core)
08/11/2022
08/12/2022
08/13/2022
08/14/2022
12/29/2022
01/13/2023
03/16/2023
03/20/2023
04/13/2023
Date Created (Dublin Core)
05/18/2022
Interviewer (Bibliographic Ontology)
Kit Heintzman
Interviewee (Bibliographic Ontology)
Brian Ghafari-Naraghi
Location (Omeka Classic)
Kansas City
Missouri
United States of America
Format (Dublin Core)
Video
Audio
Language (Dublin Core)
English
Duration (Omeka Classic)
03:13:23
abstract (Bibliographic Ontology)
Some of the things we spoke about include:Growing up American Baptist. Coming of age during the AIDS crisis as a gay man; stigma. Relationship with mother; mother dying ~twenty years ago; taking care of siblings. Marriage, relationship with mother in law, children. Son’s diagnosis with cancer. Working and volunteering in many parts of the medical field: home health aid, registered nurse, death doula, grieving counselor, street medicine, hospice director. Lost work during the pandemic. Birth of grandson during COVID. Connecting with dying clients, listening to life stories. Creating a death plan with clients, education, making your wishes known. Bodily/patient autonomy; medical advocacy. Pain management. Comparing quality and quantity of life. Dying with dignity. Media representations of death. Accessible teaching style, target 5th grade level. Emotional labor and emotional regulation; boundaries. Comfort with silence; being present. Humor, tough love, reassurance, and honesty. Patients needing touch during the pandemic. Authority and power in healthcare infrastructure. Mementos, legacy projects, respecting the dead’s wishes. Saying goodbye. Nursing homes. A nurse-friend dying of COVID. Preparing to host a Death Cafe
Growing up American Baptist
Coming of age during the AIDS crisis as a gay man; stigma
Relationship with mother; mother dying ~twenty years ago; taking care of siblings
Marriage, relationship with mother-in-law, children
Working and volunteering in many parts of the medical field: home health aid, registered nurse, death doula, grieving counselor, street medicine, hospice director
Lost work during the pandemic
Birth of grandson during COVID
Connecting with dying clients, listening to life stories
Creating a death plan with clients, education, making your wishes known
Bodily/patient autonomy; medical advocacy
Pain management
Comparing quality and quantity of life
Dying with dignity
Media representations of death
Accessible teaching style, target 5th grade level
Emotional labor and emotional regulation; boundaries
Comfort with silence; being present
Humor, tough love, reassurance, and honesty
Patients needing touch during the pandemic
Authority and power in healthcare infrastructure
Mementos, legacy projects, respecting the dead’s wishes
Saying goodbye
Nursing homes
A nurse-friend dying of COVID
Preparing to host a Death Cafe
Growing up American Baptist
Coming of age during the AIDS crisis as a gay man; stigma
Relationship with mother; mother dying ~twenty years ago; taking care of siblings
Marriage, relationship with mother-in-law, children
Working and volunteering in many parts of the medical field: home health aid, registered nurse, death doula, grieving counselor, street medicine, hospice director
Lost work during the pandemic
Birth of grandson during COVID
Connecting with dying clients, listening to life stories
Creating a death plan with clients, education, making your wishes known
Bodily/patient autonomy; medical advocacy
Pain management
Comparing quality and quantity of life
Dying with dignity
Media representations of death
Accessible teaching style, target 5th grade level
Emotional labor and emotional regulation; boundaries
Comfort with silence; being present
Humor, tough love, reassurance, and honesty
Patients needing touch during the pandemic
Authority and power in healthcare infrastructure
Mementos, legacy projects, respecting the dead’s wishes
Saying goodbye
Nursing homes
A nurse-friend dying of COVID
Preparing to host a Death Cafe
Transcription (Omeka Classic)
Brian Ghafari-Naraghi 00:00
Hi, I'm Brian Ghafari. Today is May 18, 2022. It's 3:56 in the afternoon, Central Time.
Kit Heintzman 00:11
And where are you located?
Brian Ghafari-Naraghi 00:13
In Kansas City, Missouri.
Kit Heintzman 00:16
And do you consent to having this interview recorded, digitally uploaded and publicly released under a Creative Commons license attribution noncommercial sharealike?
Brian Ghafari-Naraghi 00:27
Yes.
Kit Heintzman 00:28
Could I just ask you to start by introducing yourself to anyone who might find themselves listening to this?
Brian Ghafari-Naraghi 00:34
Okay, my name is Brian Ghafari, actually Ghafari-Naraghi, but I just go by Ghafari. I am a registered nurse with over 25 years of experience. I hold a Master's in the Life Care, a bachelor's in nursing and associate nursing. I have completed my doula training...end of life doula training. I am do some grief counseling that I was trained for. And a little bit of this, a little bit of that in the medical field. Before my previous job, I was working with ALS patients and Case Manager. Now I'm going to be doing clinical research. Now I'm going to be doing clinical research on psychedelics that pays the bills, so that I could do my doula stuff.
Kit Heintzman 01:35
Tell me a story about your life during the pandemic.
Brian Ghafari-Naraghi 01:42
I'm a homebody. So, you know, stay at home was not not a problem for me. Now, my spouse on the other hand, he likes to be out and about and it was driving him crazy. I started the pandemic out by being like, one of my jobs because I worked for organ transplants. And I was working for an organ recovery organization working with families and helping manage patients in the ICU before recovery surgery. Due to COVID We we've dropped our patient load so then they release some of us so we weren't so many of us. I worked for an insurance company for a while. I was told I was going to be a case manager, our navigator for oncology patients ended up determining our declining authorizations for medications and it sucked my soul. During all this I work end of life. I work with families, I work with patients. I am a doula. So, if you're familiar with like a birth doula where they have a birth plan, we do the exact same thing, but it's the opposite end. So, we have a death plan. So that we can identify what are their fears. I always give the example of pain, I can tolerate pain. I don't want to be nauseous. That is one of those symptoms that freaks me out. But pain is okay. So you know, it's like, so identifying what is important to the patient or, you know, how much sedation are there we're getting, give them because do they want to be able to talk to somebody, you know, if we give them this medicine or I have had some great in the life educators, Paul (unknown spelling) my mentor for my college program at George Washington in the Life Care. Jesse Roberts was a medical director of one of the hospices. Maureen (unknown spelling) was the Medical Director of the part of Care team at one of the hospitals and Karen Williamson was another medical director. So I had some great teachers and nurses. And then of course, social workers chaplains which makes it all so much easier because we it's amazing how many questions I got asked about spirituality but God about pain I actually started my journey on my interest in end of life care because I was working in the emergency room and in a burn ICU right out of nursing school, as a new graduate get all the dying patients which I ended up liking because I had my colleagues gave me that would be my only patient and Instead of having two patients, I would just have one. And I got to do a lot of teaching and a lot of education, a lot of preps about what to expect. And I really enjoyed just having those tough conversations. Because nobody wants to make at the last minute, you know, it's like you're setting in the ICU, then people walking in, what have you, have you ever talked about end of life? Now, my family, when we have like Thanksgiving or Christmas, we invite anybody who doesn't have a place to come. And my kids always warn them that I'm going to ask about end of life wishes. And my kids are in the 30s. And some of their friends are in the 20s. And they're like, well, but I'm not gonna die anytime soon. You don't know that. I said, I could walk across the street and get hit by a bus tomorrow. So, you know, letting your wishes known is a gift you can give your loved ones. So, you know that and I get to hear stories. I I have the honor of caring for patients from World War One, World War Two, Korea, Vietnam, Desert Storm, Enduring Freedom. So, you know, it was amazing. I met one of the first Rockettes.
Brian Ghafari-Naraghi 06:28
And then, you know, just getting to let them tell their stories. One of my favorite questions to ask is, if it's a married couple, how did you meet and who decided this is the one for me. I've got some crazy answers. I had one lady that told me she goes, I was on the bus. And this nice-looking young man got on the bus and she said he was going to off to war, would you want to get married? She goes, I said, Yes. And we've spent our honeymoon in the back of a gas station, we shared a bowl of ice cream. And everybody told him that their wedding or their relationship would not last. And she said 76 years. Together, all their friends had died, who said so they outlive their marriage outlived their friends. But they always had ice cream. They're on their wedding anniversary. So, you know, the oral history that I get to hear is amazing. It's very sacred to me. Because I'm getting in on the one of the most intimate times in somebody's life. You learn things about people, I had a lady that was 96 years old. And she confessed to me two days before she died, but she had an abortion when she was 16. And, you know, you think about that with Roe versus Wade nowadays. And it didn't take effect until 72-73. So, she just went to some closet. And she had not told anybody in her entire life. I was the first person so I just, you know, it's I don't shy away from things that are hard. I think that's, you know, most of my nursing career I've worked with difficult patient populations because they need somebody to be their voice, they need somebody to be there to care for him. You know, I have been witness to people passing. We may I've had help celebrating the lives of my patients. I had a patient that was in a car wreck. He was 16. And she finally was determined brain dead on February 14, which is National Heart donation day, which is Valentine's Day. So, before mom got there, mom and dad got there, I got some red heart lights, and a little bit food decorations and made a little special for 'em and, you know, it's those things that are fun. And, you know, or helping somebody understand that. You don't have to take that next treatment. You know. I'm like, let's talk about let's let me explain to you what it's going to look like. Especially like when it comes to DNRs or Do Not Resuscitate orders. I prefer AMD, which is allow natural death. Because to me, that's what we're doing. We're not withdrawing anything, we're just making them comfortable. But I, you know, had those hard conversations about, about that COVID opened up, a lot of people reached out to me because they were scared, they were grieving, you know, the loss of jobs, the loss of independence, the loss of, you know, being able to meet with friends, you love, so many people, so many things, that, you know, we weren't able to they couldn't find somebody that would specialize in that, you know, it's like, or the, they didn't know what to call it. So, you know, it's, I have a friend, that's a social worker. And, if, and if it was to, she's a therapist, and if there was too deep for me, I pass it on to Andy. But, you know, it's like, whatever I could do to help. And I'm still doing it now.
Brian Ghafari-Naraghi 11:19
We're getting ready to start a death cafe here in Kansas City. It's adaptive K, cafe, they started over in Europe. And it's just a meeting where a group of people get together, we're here, they actually be in a brewery, because that's who volunteered to host us. And we're going to talk about death. And I, I tell people I talked about death to take the power away. Because death is the unknown is unknown. And the unknown is scary. So, if we can talk about it, and take that, that ability to be scared. You know, it's, it's, it's a, it's a very freeing, because I remember that's the point that I realized, Okay, I'm gonna die. You know, it's, that's just part of life. You know, life isn't terminal illness. So, you know, I volunteer with help homeless, boats with, with the street medicine group. I volunteer a lot of as a doula volunteer in school schools around town, but I just like giving back to the community. You know, I tried to leave it a little better for better than I find it is, what is my goal and for each day
Kit Heintzman 13:02
I'd love to go back to the subject of patient autonomy and ask how you feel about that, how your ideas have changed over time and how you share that with your patients and clients.
Brian Ghafari-Naraghi 13:19
You know, it's funny, because I always believed in autonomy. Growing up, I, I remember going to a funeral at age of five, because my mom thought that's part of life. You should experience it you should not have. And so, it was never really...yeah, open caskets still kind of freaked me out. This is just they don't look normal. They don't look natural, you know, and everybody goes, Oh, they look so natural. No, they're kind of a theme. Like wax figures. But when I able to sit down with the patient, and as I see the generations go before the baby boomers, my great grandparents. So, my great grandmother had a pacemaker placed at the age of 96. The cardiologist told her that she needed to change the way she's eaten, because she fried everything in lard, butter on everything. You know, lots of unhealthy dietary stuff. But she was only four foot 10 And maybe maybe 95 pounds. But I told him she was so scared. She didn't know what to eat. And I said, let me come to you come with you to the next doctor's appointment. So, I did and at first she was a little embarrassed because I was talking back to the doctor. How dare I talk back to a doctor? And I'm like, no, this is this is your choice. I said, honestly, I said, if we draw everybody's cholesterol, you probably have the lowest cholesterol of the three of us. Because her body is probably used, you know, she's done it for 96 years, nothing's going to change overnight. So. So that was my first time being able to advocate for somebody. And then my next chance was my great grandmother on my father's side. And we were all sitting around. And they told us that she would probably never get off the ventilator, we could keep her on the ventilator to her feeding to. And my grandfather, her son said, that sounds good. I said, I was probably sixteen at the time. And I said, is that what she'd want? Like? She's a big Royals fan. And loved Royals, love go into the game, you know? And I'm like, she won't be able to do any of that. So laying the bed. And he goes, Oh, I didn't think about that. That I said, you know, for some reason, when I came of age is the AIDS crisis started, and I remember being 15 years old, voluntary, at a Catholic hospital. And I was taking trash back to the to the utility room and in the hallway in front of the jury utility room with a patient on it on a gurney. And I walked over to him and I said, what happened? Why are you back here? And I touched him, and he goes, Oh, you don't want to touch me. I'm like, Why? Because I have AIDS. I said, Well, you know, this, this is why I look at your skin's intact, my skins intact. I don't think I don't think I'm okay. I think I'm okay. So, then I started volunteering as a home health aide and taking care of people getting them in the showers when I was in high school, because, you know, nobody wanted to do it. You know, and being a gay man, scared scared me to death. You know, at one point, I thought that that was, you know, I was gonna get AIDS and die. Because that was in the early 80s, early to mid-80s. That's what happened. And now it's a chronic condition. But, you know, the stigma is still there. And having patient being able to encourage patients to express their wishes, is so rewarding. And again, it's that sacredness of being able to be part of, I'm part of the family, but I'm not, you know, because you don't talk about things like that with strangers. And, you know, when I sit down with a family, it's like, we're gonna talk about some hard things. We're gonna talk about funny things.
Brian Ghafari-Naraghi 18:27
I said, I'm gonna mix it all up. Because death to me, is kind of funny, you know, and as a hospital, hospice director, I went on a on a death call. And I first time meeting this patient, I go back and check her pulse did all my assessment and yet she was dead. I come back. All right, go back into the living room, sat down, start to explain to the family and I hear this uhhhh. So I get this panic look, you know, not panic, but it's like, Oh, my God, I totally missed something. So I excused myself went back to the bedroom. Listen for two minutes with my stethoscope did reflect nothing, walked back out, sat down and started talking to get in and heard the same noise. And at that point, the family goes oh, we have an asthmatic dog that's under the bed. (laughs) So you know...you find you, you know, I think when if you can find humor in the hardest part that makes it so much easier. You know? The first thing I tell people is if you think you have anything under control, that's your first mistake. Because everything's gonna happen no No matter how well we plan, we plan, and I always tell patients, I said, ?I got a through z backup plans. Because nobody's going, I said, if I tell you this is going to happen, something opposite is going to happen. So we'll, we'll be prepared. But letting you know what I'm talking about Golden care. Work with the wonderful oncologist, just one of the best people in the world. But he would give a rock chemo, if they asked. And it's like, why are you giving them chemo? We know, the chances of survival are 5%. So, we're taking what they see have the chicken feel healthy, and making her sick. So, to me, those are days that she can go out and have ice cream with their kids or go to the park or you know, do something that is not being sick in a bed. You know, I as an ICU nurse, I, we kept patients alive because we could. I remember a patient that had meningitis, and she had been in the hospital for three months. And I was getting ready to leave shift and I walked in to hanging in a bag of fluid. And I'm like, God, this room is hot. And I'm like, wait a second. I'm only hot on my left side, which is the side that's closest to the patient's like turn to face the patient. And it was like opening an oven door to the temperature 106. So, our fellow came in, looked at it. First thing he said is let's get the Echo, the heartland bypass. So we won't need the patient. Like, you know, it's like we're taking away her ability to die with dignity. You know? And it was funny because her husband I, I saw six years later, and I was having questions about should I be a nurse? You know, was it worth it? And he goes, you made the world of difference to us. He goes, we were able to make choices because we were informed. And General. One thing my mom taught me is knowledge is power. So, you know, it's explaining things to people.
Brian Ghafari-Naraghi 22:57
The DNR Rs, if you ever watch any TV shows, you will see a patient go into cardiac arrest. And they do a couple tests compressions. They give a couple injections of meds and, and they talk them once or twice and in 15 minutes, they're setting up and talking. Well, that's not reality. In reality, what it is what happens is we push on the chest, we break ribs, we bruise the muscles. It's painful. And if we get a rhythm back, it, we might not be sure that they don't have any brain damage for 72 hours. So, you know, it's a good friend of my mom, or a good friend of ours, her mom had lung cancer. And Mommy didn't want to listen to anybody. And she knew that she was going to die. And of course, she wanted somebody to do everything to save her life. And so, it was funny because our friend was my partner Secretary when he was a school superintendent. And both of them were older than me. And mommy says, you too need to leave grown people need to talk. So we just talked about what it would look like. And she goes, Oh, that's horrible. I get asked that. And I'm like, well, but you know, for some people that's important. It's not the quality. It's the quantity. You know, it's and I said that's a very personal decision. How do you know my husband and I don't say I die. If a cancer and I don't have a bit, if it's a 50/50 chance of survival, I'm gonna go live it up. I'm gonna spend every day my hands, do things that I would never do before, you know, because I don't want to be sick. And sitting in his chair, I seen that too much. But when you're able to empower patients by education, it's it's like a proud parent, you know, it's like, you get you see them, talk back to the doctor, but more question them and ask them. Why are you suggesting this when that x, y and z could happen? And isn't XYZ worse than what this is. And it's amazing by having that knowledge and that power. Because, you know, when you go into the hospital, they take away everything down to your underwear. They take all your clothes, if you're a woman, they take away your makeup. You're lucky if you get to keep your glasses in your teeth. You're stuck in a bed, and you're at the mercy of nurses and personal assistants. And I know that everybody means well, but sometimes they're just too busy. And sadly, patients don't get the care they need. You know, I, I tell people that if you have a loved one in the hospital, somebody needs to be there to be their advocate. And like when I would do teach them with my ALS patients, or my oncology patients, the first thing I would tell or after we were done with my teaching, and I would have that brief down to thirty minutes. I would tell just, that was my initial teaching. And I might if you remember three percent of what I said today. I did I had a really good day. I said, here's my number, so that you can call back when you're at home. And it's like, Oh, I forgot that. To ask this question. And you know, it. It's empowering to the patients. Because I remember my son when he was fourteen year old, fifteen years old had Hodgkin's lymphoma. And I remember sitting in the doctor's office, and it was at the hospital, I worked at the they said the pathologist is going to come in and talk to you. Well, the pathologist walks in, and she was the wife of the Burton fellow. And I knew she did oncology. And so, I immediately reached for the trash can. And both my son and husband are looking at me, like I lost my mind. And I'm like, it's cancer. And it's like, okay, let's slow down and think about this and and then we got through it. My son, you know, at that pre for that teenage years, you know, not as kid not as adult, but in that if he stage and I told him that, if you want me to treat you like a grown up, you need to know what teenagers are hanging the side effects, which order it goes in. Because he he got like, eight different drugs and certain drugs had to be given before others and he caught a mistake. Because he was told that, you know, he he didn't miss on school that year. Because, you know, that wasn't his school counselor. I'm a nurse. So, you know, it's like, you know, people have it worse. You gotta keep going. And he's still with us today. And he goes, You could have let me slack off just a little bit. Like no, because you're here to pitch about it now.I did my job so, you know, just being able to talk to people and have open discussions.
Brian Ghafari-Naraghi 29:43
My neighbor next door to me, called me and they said, I have a questioned, because my dad then proceeded to tell me the story of his dad and they were deciding on whether to start dialysis or not. And it's like, okay, well, let's look at his health. And, you know, I sit down with a pad of paper, and we write pros and cons, for what symptoms, what might happen, or are, what side effects may happen. And then we just, to me, I, you weigh it out. And, you know, I have patients that have a five percent chance of survival, and they're gonna take it, and I support them and one hundred percent I had a patient that had a history of breast cancer in her family, and she had a double mastectomy. And it's like, whoa. She had to get surgery before she even had a mammogram. And, you know, it's like, okay, well, my job is to educate, to support. I, you know, I, I'm not affected by it, I can't tell you what's going to happen. And I have to explain it to you, in the easiest way possible. And I always tell people, I might, my teaching is on a fifth grade level studies have shown that it will cover ninety percent of the population. So you know, there are patients that that I say, Okay, this is how I explained it. Now, what are your questions, and some will ask me, the past the pathophysiology behind the cancer, and that's fine. But some people don't want to know, you know, it's rapid growing cells, it's cancer, you know, and that's fine. But the other thing that's sacred is being able to be there when somebody takes their last breath. It's that completion of the lifecycle. In nursing school, all the all the ladies wanted to go into the labor and delivery, the miracle of birth, that had no appeal to me, I did not want to be there. Even in nursing school, I would switch out because we could do NICU and we were doing NICU and mother baby, I would take Nick You wouldn't have to be in labor and delivery because I knew that wasn't where I wanted to be in life. But the more I look at it, it it's the it's the same sacredness of the end of the pool of the life and, you know, honoring the person, whether it's spiritual. You know, some people want you to set a fireworks, you know, pour one out. I attended a funeral of a twelve-year-old little boy, his father was in a Mexican gang. And as I was getting ready to leave the service, I get pulled back behind the church with a big group of men, that I'm like, oh, Lord, I'm going to be shot. Because they were menacing looking men, it takes a lot to unnerve me. And they're like, No. And of course, they didn't speak much English. But I had to take a shot of tequila with them. I had a patient that her wish was she she lived in a retirement community, and she didn't want the old biddies to know that she was sick. So, she laid down some ground rules. I was never supposed to be never come wearing anything that identified me as a nurse. I couldn't have my stethoscope out. I couldn't have the scrubs on. I just had to like bring bring it back. Sure. Okay. So, this is this is a woman that her husband was a lobbyist in Washington, DC. And when I asked her if she was religious, she goes, Well, I went to the National Cathedral to be seen. And so, you know, there were, there were certain things that she liked. I couldn't go over a certain time because for her, she had to get her hair and makeup on before before she was ready for me. And then it got to be I was putting doing hair and makeup. And when she passed away, she was somebody that I went after work and we had cocktail hours She's like, I, when I found out when she found out that she could drink, whatever she wants, she goes, Okay, I want to lemondrop I want to Manhattan. Then she had this list. And she one-two sips. All these drinks out. It was, it was her, her niece, and her sister-in-law and her brother. And she had no children. So, she told everybody at the facility, I was the grandson. Nobody put together that she didn't have to have a child to have a grandson. But so, she passed away. On a Saturday, I was actually out with my family. And I'm like, Okay, guys, I need to drop me off. I need to go handle this. And so, I went, went there, I snuck the funeral home people up there, we got her in and out of the building without anybody ever knowing that she had that she died, or she was sick. That was she was too proud to she didn't want to look weak.
Brian Ghafari-Naraghi 36:23
And people that are dealing with the end of life, they're not weak. There's some of the strongest people I know. You know, some, some people get angry. And I always tell them, my two things that I ask any emotion is okay, the two emotions that are not okay, is wanting to harm yourself, or wanting to harm others. And the two behaviors that are not acceptable is you spitting on me, or hitting me. And hitting, I'm pretty flexible on that, you know, if they're a little tiny person, I could probably take a blow or two, but you know, it's but giving them the chance to, you know, yell at, I tell them, you know, get out every emotion. I talked about doing a therapeutic scream, I would do it with my oncology patients. And I said, sometimes you just need to scream at the top of your lungs. Well, we had some new staff one day when I was doing the therapeutic screen, we had 10 people. But you know, it was teaching, you know, meditation and guided imagery, aromatherapy, using a nontraditional, with the traditional, I think combines beautifully. I have pre our did a service for a patient of ours, or of a patient of mine that was Scandinavian. So Nordic, the Nordic gods. And so I had to, they had a whalebone that they had, he had to keep in his hand, and I had to figure it out. So do a lot of research. You know, and the other thing too is when I'm talking with families, is I always explain I'm going to start off with saying I'm a human, and I make mistakes. So, I try to understand your culture or your religion, your belief system, but sometimes, I don't know every little detail. In the Hmong tradition, you don't say the word death, you don't say dying. Anything related to that will will cause the person spirit to follow you in the afterlife. So, I, I had read up on this before I went to approach his family and talk to him about death. And I was watching my words very closely. You know, it's like good news. And, and I would stumble a few times. But I because I've started to say something. I'm like, Oh, wait, let me let me rephrase that. And the younger generation laughed. They're like, we appreciate you trying to honor our elders. You know, but I grew up American Baptist. What Methodist Church, Buddhists now, sometimes, you know, at one point I was an atheist, you know, it's into life will make you question and everything because I had I had to start believing in what I consider Omni God, everybody prays to the same God. But we might go a different path. Because, you know, the idea that I die and I go to the pearly gates, and I've been a good actress my whole life and they say, Sorry, it was Episcopalians that were correct. You know, so I have to believe that we're all on a spiritual journey. And, you know, we we get there in our own time, and you know, who's right or who's wrong is anybody's guess. You know, that's the thing about into life, is you get to talk about anything and everything. You know, I had had a couple she was terminally ill, but wanted to have sex. And they're like, they were him. Hi. And I'm like, Are you asking about having sex? And the white blood test? Thank you. Hey, I said, if you feel like it, do it, you know, it's, it's a natural human process. You know, it's, you know, it's, I always tell patients, when we're talking about living with a terminal illness, this is the time of life that you get to eat whatever you want. It's ice cream for every meal. It's ice cream. You know, it's, I said, this is, this is your selfish time. You don't have to please anybody.
Brian Ghafari-Naraghi 42:07
And, you know, I learn so much from my patients. I did an oncology camp for kids. For several years, I was this camp nurse. And I had my three what I refer to as my three stooges. There were three girls that had the same diagnosis the same age, and they were the best friends. Well, Ally, on the night of our dance, which was the night before camp, and and her we, we figured out her cancer recurred. And at that time, I was a pain management nurse at the hospital, so, you know, we, we would go and make recommendations for people's pain. So that, you know, they would wouldn't be undertreated. And I remember getting a call at two o'clock in the morning. And Ally goes, Brian, this fool is trying to give me a milligram morphine. She goes, I think more than that, right through. So I got on the phone with the resident and did the education and he didn't, he didn't want to. He's like, Oh, no, that's too much for her. Like, it's not. And I said, you know, it's, it's at the point where now, you either write the orders, or I call the attending and the attending was the oncologist took care of my (redacted). Dr. Smith, one of the first things that I told my family when they saw Dr. Smith they said, Please don't judge her. Her hair's gonna be nappy her clothes are gonna be wrinkled. She's gonna look like she rolled out of the bed, because her philosophy is she takes time to get her hair down, put on makeup, press clothes, that's time that she's not taking care of her babies. And so, I call that runs a divert. This is just as funny issue. As he goes, I got to and everything was ordered. And, you know, Ally was somebody that I got to know personally. She had a bone marrow transplant. So I would see her in the bone marrow unit which is very, you have to sanitize and scrub down And you can't have plush toys or you know, everything has to be wiped down. So we would joke about from Steel Magnolias or favorite colors or blushing basketball. She loved pink. So, I found some pink plastic flamingos that we decorated the room with because they could be wiped down. So, but sadly she ended up she was dying from her cancer, they did everything he could. And I went over to her house to go see her one last time. And, you know, I started off with, I'm so sorry, you had this cancer, I wish you'd never would have had this cancer. It's just not right. And she looks at me and she goes, but I never would have met you. I said, there you go make me feel like an asshole. I'm tearful, and she's thankful that she got to meet me. It's like, okay. But, you know, it's, it's those things that, that make you humble. You know, it's it changed my view of how I live my life, because I do things that I want to do. If I don't enjoy it, or if I don't love it, I don't do it. because life's too short. You know, there's some nights I have ice cream for dinner. Now the kids are grown, I don't have to put a healthy meal on the table.
Brian Ghafari-Naraghi 46:56
But death takes away all pretense. Everybody's the same when they're dying. You can be rich or you could be poor. And you end up in the same place. And, you know, I've taken care of celebrities, and taking care of people that were homeless. I had a patient I used to go see you in a slide on a playground. It was one of those covered slides. And that's where he lived. Then I had patients in the penthouse in the most expensive part of town. Actually, my preferences are poor. Because they were always thankful. You know, sometimes the rich patients were a little bit entitled or, you know, it's like, I had an emergency. So I'm five minutes late. And I'm like, I called you and told you I'm gonna be late. And I'm only five minutes late. Well, you're wasting my time. And I'm like, okay, but if that was you that had the emergency. Do you want me to leave? And, you know, I tend to be blunt. I joke that I like that filter that says that you should wait, stop think, should you really say that? Now, I just found out that I go go with death. Dying. Straightforward. can be harsh terms. But then there's no confusion. I always tell people, the worst thing that you can do for a child is, especially grandpa or grandma dies. And they tell him well, grandma went to sleep. Well, that's not gonna go to sleep ever again. Because if you go to sleep, you're not gonna wake up. So, you know, if, if there were kids involved, I would get permission from the family. And I would sit down with a child and explain to him what we going to see in the ICU. What tubes. She's gonna be looked at what and, you know, I'm like, she's come, they're comfortable. But it's still scary. But they're there. They're comfortable. And I always tell them, because it's my belief that the last thing togo is hearing. I tell them to tell, you know, you got to say your last whatever. And, you know, even with patients and families it's a you gotta say I love you. I hate you. Die, you know, but say your piece because I don't believe in the word. I don't believe in closure. But I do believe in having a final conversation or a, you know, put a period on that. And, you know, it's and I'm a realist, too, when we, you know, when we talked about, everybody becomes a saint when they die. And, you know, no matter how bad a person is, they were such a wonderful person. And, and, you know, I'm like, I don't want to disparage anybody, but that's not who that person was. Let's be realistic in. My grandmother was a horrible person. She was a nasty, cranky old woman. And she, that's when she died. She died unhappy and you know, and it's like, that was her choice. And, you know, it's like, but then I have people that are very comfortable. We're okay with it. One of my ALS patients from twenty years ago. Ivan, he was a gentleman in his fifties had a child later in life. So she was the same age as my daughter at the time. So she was like twelve. And Courtney ran track. And Ivan had gotten weaker where he needed to start using a walker. And he was not going to use a walker, because that made him look weak.
Brian Ghafari-Naraghi 51:46
And I'm like, no, what makes you look weak is when you're on the floor. But, but that's okay. If you don't want to go to Courtney's track meets, that's fine. Because your pride is more important than seeing your daughter run. I'm okay, I support you. He called me a bastard. And he told me that I was fighting that I wasn't fighting fair. But he started using his walker. And he asked me to, to watch out for his daughter. So Courtney, to this day, is my daughter, I stay in touch with her, she calls me at least once a month, just checking in, you know, because that was important to him. And, you know, it's I think honoring somebody's wishes is the most honest and giving thing you can do. You know, one of my other hospice stories that I laugh about was, I was on administrative call, and we had several deaths. So I went to do a death call. For some of his family, this guy was big, he was six, seven, and about 320. And I was by myself. So, you know, part of the getting a patient ready is, I give him a bath, and I get him dressed, because that's the last time they're leaving their house. So I want to make sure that they look the best they can. And, and I'm from the old school that I talked to the dead bodies, because if I'm, if I'm doing somebody a bath, I'm gonna raise your right arm, and I'm going to use this warm cloth and wipe towards you. So whether they're alive or they're dead, I treat it the same way. Because they still are human. That, you know, it's still somebody's mother or brother, you know, there's somebody's loved one. Well, his wife kept changing her mind on what he wanted to wear, or what she wanted him to wear. So I was playing dress up with this huge man and changing him in to six outfits to getting to look just right, so so he could go to the funeral home. But she needed that, you know, I was exhausted. But, you know, it's like, I that's part of the deal for me is, it's not about me when I'm taking care of people don't matter what is going on in my life that has to stop at the door. And I'm always smiling and happy and you know, when appropriate. Because I try to I hate hospitals that are so sterile. You know, it's like, okay, can we get In color in here, let's put some music on. You know, I always asked the family what what kind of music do they listen to? And my patients did have meningitis that had that spike that temperature. We had her for probably about two months. And she was unconscious. Two months, and she woke up while I was giving her a bath. And she mouthed. Where am I and what happened? And I'm like, Are you talking to me? Yeah, it was like, it was so weird. You know, it's like, Oh, my God, she's interacting with me. And so she got better for a few days, which patients do rally, which is a gift that they can give their family, you know, you get to see him one more time, or they get, you know, mom gets to feature your favorite dish one more time. But, so this goes back to my, my theory about hearing. She looked at me and she goes, You're the nurse that sings? And I'm like, Oh, my God, I am so sorry. I'm a horrible, I can't carry a tune. But, you know, Earth Wind and Fire was her jam. So I'd be in there working and just so, you know, it taught me that. You know, it's like, but she thought it was funny, you know, at least I knew somebody was gonna have a fun having fun with me while I was there.
Brian Ghafari-Naraghi 56:41
But, you know, I get so much more than what I what I give back. Or I it's amazing. I can travel anywhere in the country, and I'll run into somebody that I've taken care of one of their family members. So weird, you know what it's like? Okay, yeah, I have lots of nursing friends that I was, you know, an official hospice nurse, because the dad or mom or dying at home and they hadn't questions and I'm like, Okay, do you need me to come over and check them out? Sure. You know, it's because I just think that's as human, that's the easiest thing I can do. It might inconvenience me. But what is it, you know, 30 minutes or an hour out of my day. That gives them a good memory. You know, luckily, my family understands. My husband was a school superintendent. So school came, you know, he had his kids calling him and I and my patients and, you know, our, our kids grew up knowing that you had to take care of you take care of your elderly, you take care of the sick. Because we're part of the big community. And if we can't take care of each other, where's our humanity going? And I think part of the COVID thing was we lost some of that humanity. No, personal touch. No, I I had a patient that told me, she goes, I just want a hug. I said, Well, I've been vaccinated. If you want to hug me, or if you want me to hug you go ahead. And early on, I was taught by a very wise nurse that you give when you're hugging a patient like that you give Disney Princess Disney Princess hugs. So like at Disney World, they do not let go first. So the patient has to be the first one to let go. So I'm hugging them until they release. And, you know, I've stood there 10 minutes on days. You know, I I work really hard at not crying in front of the family. It's hard. I will go into the bathroom or duty utility room. But, you know, to me, they don't want me to cry. I gotta be the strong one. If they're comforting me. I'm not doing my job.
Brian Ghafari-Naraghi 59:56
And you know it my mom died early, she died up to 53 of malignant hypertension. She went unhealthy to dead within 36 hours. And I come from a big family. I had a brother. So, I was 30. And I had a brother that was 12. And a brother that was 16. And so, okay, guys, Mom is dying. What do you want? Do you want we can say here at the hospital, we can take her home? What is it that you guys want? And sort of you letting the kids decide that it's their mom to you know, it's like everybody gets. I'm like, there's nobody here that gets a override anybody else's vote. Because my stepfather, he says, it's up to you. And I'm like,I understand. I'm a nurse, I'll make those decisions. And, you know, it was kind of funny, because I stayed with my mom overnight, and she had some changes. And so I asked the cardiologist, if we could do a CT of her head to see what was going on. And so he, we get the CT, he comes back and he's like, Well, she has a bleed. And I'm like, where's the bleed that you're talking about? And he goes right here, I said, No, no, that swelling. So we have a 10 minute discussion. What, why he thought it was a bleed, not swelling. I said, you know, have a neurologist or neurosurgeon come in. Somebody that's trained to read those. So I'm in my mom's room, and I could hear him talking to the new doctor. And I hear this man say, she has a son that's a nurse that thinks he knows more than a doctor. I was loaded for bear. I flung those curtains open, two steps out of the room, looked up, and the person that was standing there she goes, is that the uppity nurse? And he goes, that's her son, you know, tried to? She goes, yeah, it's swelling. I taught him how to read those. It was a doctor I had worked with, in neurology. And, you know, it's like, I knew that, you know, it killed April, to have to tell me that my mom was dead. You know, it's like, I wouldn't want it for anybody else. I want, you know, she holds a special place in my heart. But my youngest brother did not want my mom to die in the hospital. So, I asked the cardiologist if he would just take to my mom home.
Brian Ghafari-Naraghi 01:03:24
And he said, Absolutely not. She's dead. So, I said, Give me a second. I called down to the emergency room and I said, Dr. or Pam, this is Brian. My mom's currently in the ICU. I want to take her home. I'm gonna need to bag her to take her home and withdraw care at home. And I said I need to do to be her physician. Because the cardiologist won't do it because, sure, so I looked at him and told him he was fired. And then I went into what my siblings were referred to as drill sergeant mode. My mom was a red Hatter. So I sent one brother home to get her, her Red Hat. I sent my sister out to get her new purple night gown. My older brother was going to the pharmacy to get meds. I had called all the DME to get it arrived at the house Daphnie was at the house, getting it ready. had had friends my my parent, my mom and stepfather’s son was, You're in my heart by Rod Stewart.. So friends went out and found that CD for him. So to get the house ready, I told Danny I make something spaghetti because we got to feed everybody because my mom fed everybody. She was everybody's mom. And so I explained I explained to the ambulance company, what we were doing. And I said, I don't have a problem bagging her, you know, you know, I'll I'll do the bagging all the way home. And they're like, Absolutely not. But before we leave the hospital, I was the director of a hospice at the time. And I called my on-call nurse and I said, Mary, and I started rambling off of everything that I got and what I was doing, what was I missing, and she's like, slow down, Brian, what's going on? I said, my mom's dying, and I want to take her home, and I'm going to extubate her when I get home, she goes, You are most certainly not going to extubate your mom. She goes, You're the son. She goes, call me when you leave. I will be there. So I had half of my staff here. So we had a caravan of ambulances. So there's like four of them that followed with lights on to to our house, our driveway was lined with Tiki torches. There's candles lit all over the house. My moms song was playing, you could smell the spaghetti. And so why, I let my friends prepare my mom, get her settled in. I'm in there feeding the, the ambulance, the EMTs and paramedics. Because my mom would want that. Because that's rude. You know, you don't you don't have people over to your house without feeding them.
Brian Ghafari-Naraghi 01:06:47
And, you know, these paramedics will just like shocked that I had to make sure they ate it and like, it's like, it's part of the deal. That's who this woman is. That's how, how we honor her. And, you know, so we ended up taking her to my house because my brother didn't want her to die in his house, which is fine. You know, 12 years old, I understand. So I have this big picture window. And we sat, we set the bed in front of it. We all sat on the bed with her. She had six kids and her husband, so and my cat. And we just sat there while she passed. And we told stories. My mom would always tell everybody that she never did much in her life. And she wanted to be a mom. And she was the best mom ever. She worked probably in her entire life a year as a housekeeper. Because I worked at the hotels as front desk, and she could come with me and she can make some extra money. So, you know, and she's like, I didn't make you know, she'd always say I don't make a big difference in the world. So when we had her funeral, my mom hated the fact that my sister and I wore black all the time. So I told everybody that was invited to the funeral is you were the brightest color you have. If anybody wears black, I'm kicking you out. And people, we had people at the altar that we brought things that reminded us of our mom. I brought a bottle of windex because she was always wiping down the glass window, the front door. You know, I my older brother brought pot, furniture polish because she would she polished she would come over to my house one day a week in his house and clean our house.
Brian Ghafari-Naraghi 01:09:27
Well, she had waxed his tables, and he was climbing up on the table to get to change a light bulb and slid off the table. We had the minister; he had his black robe on with the with the purple boa that was hers that she wore with a red hat. And, you know, we had Aerosmith playing at the church. So, you know, Lovin in an Elevator because my mom was a big Aerosmith fan. We had a a traditional non-traditional funeral, that was at a church. I was actually finishing my Masters. And the night before she, so they would come over on a Friday night. Because I had...there was my son. And a year behind him was my, my brother, the year behind him was my sister, or my daughter. And then I had a brother that was three years younger than that. And so, you know, they were raised together as brothers, you know, and I had a pool and so you know, my, my family would come over, we would spend Friday night hanging out. I had just I was doing like children and grief class was what I was doing. And I had to find a book to present to the class. And I found this wonderful book called The Next Place. And I by Warren Hansen and it's it's a beautiful book that explains death in such a gentle way. It talks about I won't be short or tall. I won't be fat or skinny. I'll be perfect. I'll be me, humbly in the ever darkness. I will not be alone because I take the memories of my loved ones. So that the Friday before she she had had the malignant hypertension. We read the book back in my office and where I'm at now and she goes, I need to borrow that book because I want to take it to the old ladies to Red Hat. You know, she called her red hatters the old ladies. And so, my husband read that book at her funeral. We had a couple of songs. And then we did a poem. We're not meant to go to cradle to grave in a perfect perfect wrap box. Were supposed to we should be sliding in sideways, totally worn out. Totally used up. Exclaiming Wow, what a ride. And that's how my mom lived her life. She she was a life of the party. It it's just sad that she didn't get to see her grandkids and great grandkids. But I know she's with us. I have a niece that I swear to God as my mom that came back. She's called me a nickname that my mom only called me. And she died. My mom died 12 years before but before she was born, she was like she my mom would call me Bri-Guy. And I'm like, so we were at the park one day and she called me. Where did you hear that? I don’t know, that's your name is. But she looks like my mom. She acts like my mom. It's just kind of weird. But you know but it gave me a whole different understanding of death. You know, I told people I had attended many deaths.
Brian Ghafari-Naraghi 01:13:54
But my mom has changed me. I I was a mama's boy. My mom and I did all sorts of things. On my birthday. The annual tradition was I would take her out for the day. We would go shopping for her we would get her a nice outfit. We'd have a nice lunch and just spend the day together. Wasting the time. You know who would go to a museum Um, we could be a thrift store, you know, it was just spending time together. So, you know, she was a significant part of my life. And so, when I, we had her curt...cremated and I asked my siblings, I said would you like a necklace with some of her ashes in it and they all thought that was the best idea in the world. Well, so when we had her cremated, she collected amber glass. So instead of using a regular urn, my, my mom's goal in life was to be a drag queen. Because she said that they had the best clothes, the best hair and the best makeup and jewelry. Because she was a stay-at-home mom. I don't get to dress up like that often so. And she chunky. So, she always says she was stuck with fluff. So, in, in the glass urn we wrapped in some gold LeMay. So I had to pop open the the urn to break it out to get the ashes in it. And my sister and my husband, we're in the living room, and I'm in the kitchen. And all of a sudden, I start laughing hysterically. Because I open it up. And I start pulling out stuffing, like pillow stuffing. And I'm like, oh my god, she was stuffed with love.
Brian Ghafari-Naraghi 01:16:18
And it was, you know, that just gave me the moment that I knew that. I did the right thing. You know. And I she had she had an anaphylactic reaction to IV contrast. And I was holding her right before they put her put a breathing tube down and she goes, Don't let me die. And I said I won't. And you know, I didn't have anything, any control over that. I know I shouldn't promise that. But that's what she needed to hear. And, you know, I had a little problem with that. There, there was a little survivor's guilt after that, but I knew I did want honored her. And, you know, I made sure that everybody was okay. I ended up stepping back from being a hospice director. Because I was working 70 to 80 hours a week, because I had two younger brothers. And my mom always referred to her having seven children. And one of them being my stepfather. And I we didn't really grasp the knowledge until after she passed away. The Sunday after she passed away, he went to my sister and said, What do I wear to church, because my mom would set his church clothes out for him. And mom was the more the disciplinarian. He wanted to be their friend. So, I needed to be out of all my siblings, there, there was four of us. One was just a young adult. One was in her mid-20s. I was in my 30s and my brother was two years older than me. So, we had to take over those responsibilities. And my brother was an auto body painter. My sister was an accountant. Another brother was a locksmith, but I was a nurse. So, I took a night. I was a night administrator at a university hospital work three days a week, so I could be off during the week to go check in on my brother because, you know, he, he was a little shit.
Brian Ghafari-Naraghi 01:18:47
I went to school to see how he was doing. I said, so, how's his grades? And they're like, well, we're not pushing him. He's having a hard time. I'm like hard time about what? Your mom dying. I said you need to get him down here now. And so, my brother comes walking in, he looks at me. He goes, What's the matter? I said, if you've been lying, he goes, they asked me if I'm sad, and I say yes. And then I don't have to do any schoolwork. And I'm like, Brandon, what would mom do if you if she was here? Kick my butt. So, what do you need to do? Do my schoolwork. And, you know, it's like, the school counselor thought I was just the meanest person in the world. And I'm like, No. I know my brother, he...he is a body man. But there was a time in his life that I was wasn't sure he was going to be a hitman for the mob, or the President of the United States, it could have went either way. Because he was, he knew how to work things. He was the baby of the family. But then I had another brother that was skipping class. And so, I had worked it out that when our, when I couldn't, I told him, I said, if you aren't showing up to school, I'm gonna start showing up to school and dragging you there. Because that was my mom's number one rule, you had to graduate high school. Didn't have to go to college. But you didn't have to have your high school diploma, GED didn't count. And I said, I, I will black out my teeth, wear junky clothes, and follow you around to every one of your classes. And I said, when I went, I'm not able to do that. Judy, who was my dad's cousin, was also my mom's best friend. And she was a retired schoolteacher. And she goes, Oh, my God, this would be so much fun. So, he had the threat of two people coming up dresses, you know, embarrassing. He graduated high school so. You know, it's like, we had had things that we had to do. And you know, it was great. It turned out good. You know, we the three older kids became the parents, as we are still to this day.
Brian Ghafari-Naraghi 01:21:35
And, you know, my youngest brother went and lived with my oldest brother, because his son was not that much younger or younger than my brother. So, you know, it's like, okay, they were going to the same school. So it worked out really well. My other brothers stayed with, with our dad, we didn't get him through school, but we probably should have moved him into one of our other house, my sister's house or my house, because my dad just didn't make him do things. And, you know, it's like, death is sad. And I remember telling my family that they said, death is sad, but life goes on. And our mom would want us to go on, she'd want us to do stuff with our lives. And when she said do stuff, it didn't have to be, you know, professional, you know, you didn't have to be have a college degree you didn't, you know, as long as you did something that you loved, and it helped others or contributed to society. That's all she wanted. And we all do that now. You know, and it, I went from working 70-80 hours a week and having a part time job to work. It's not about work. You know, as much as I love my jobs. If I die tomorrow, they'll hire somebody to put my place. And it'll keep going on. So, I look at life now that if I die tomorrow, would I be happy with what I'm doing?
Brian Ghafari-Naraghi 01:23:28
And, you know, it changed the way I look at life. And I live free. You know, it's the choices I get to make. You know, it's like, Does this bring me joy? If it doesn't bring me joy, why am I doing it? And that's what I bring to my patients. You know, I help do lifetime legacies. So that could be a scrapbook with a patient for their family. Ivan wrote Ivan got cards for Courtney's 16th birthday, high school graduation, college graduation, masters, when she gets married and when she has a baby and he got cars and gifts. For each one of those milestones, granted, she said that she'll probably never get the child and the marriage gift, but you know, that's okay. But he, he's been part of every milestone in her life. I worked with a friend and we videotape somebody telling their life story. And, you know, these are such things that I missed out on, because I didn't have enough time with my mom. You know, I tell families like when you're having the service for them, but in the back of wherever you're at, or table up, put a picture up and put a sign that says, Please write your favorite story of our mom or our son are... Because the one thing I noticed, I discovered was from my mom's funeral, people told me hundreds of stories that day. I can't remember half of them. And so I suggested that to a family, and they did that. And the wife called me back about six months later and goes, Oh, my God, these are so comforting. So, you know, it's it's the stories that people don't always know. You know, it's you know. I did stupid things. When I was a kid. I car surf, I would get on an I-70 and I had a Celica Supra was a moonroof. So, it opened up, I would plan out the moonroof, and stand on top of the roof, going ninety miles. It's a miracle that I'm alive. Why I thought that was fun. I don't know. I was younger and dumb. You know, I get some of the best stories from people about their life, you know, I, I go in. And any job I've ever had, I've told my boss, I'm going to take the time with patients.
Brian Ghafari-Naraghi 01:26:47
Whether that be thirty minutes or an hour, they get my attention. I sit down. And we talk. Because most people are scared, you know? Or they've never been in the hospital before or, you know, they just got a new diagnosis and they don't know what, what to do with it. What does it mean? And, you know, there's a movie called Wit. It was actually a one-person play. And it's about a college professor who was a English literature specialist. And she's diagnosed with terminal breast cancer. And in one of the scenes, she's getting informed consent about the chemotherapy treatment. And this doctor is talking way over her head. And, you know, she has her side dia..dialogue. It's like, I'm talking Chaucer to this man. And, you know, so I teach ELNEC, which is end of life nursing core curriculum. And I love to show videos, or you know, snippets of movies that talk about dying in a good way or a bad way. Have you ever seen the, show Little Miss Sunshine. It's a very funny show. But it's about this little girl going to a little pageant, Little Miss Sunshine pageant. So, they're taking a family trip from my, Arizona to California. Well, on the way there, grandpa dies. So, the hospital social worker comes up and says I'm sorry for your loss. Here's this paperwork that needs to be done. And, you know, it's everything that you wouldn't want to do. Because, you know, it's like, it gives people a good idea of what not to say, you know, or I tell people I always start off with I'm human, I'm gonna screw up. So, if I offend you know, it's that was not my purpose. Everybody's family communicates a little differently. And I say that I know I'm very straightforward. And I use harsh word. But I don't want there to be any confusion. You know? Like when somebody says, oh so and so moved on, where they moved to didn't move across the street, did they die? Did they move across country? You know, I don't like ambiguity. And because death is such a hard topic to talk about, I don't want it to be ambiguous. And sometimes, you know, family members, and I will tell them, I'm going to use harsh terms. And if you don't want to hear them, this might be the time you step out. Because I want or when I'm having a family meeting, I want everybody to be there. Not that I want to be the center of attention because, Lord, I hate being the center of attention. I'm a wallflower. You know, they always say there's a gardener. And there's, there's the flower. I'm definitely a gardener. But I know that I can do I do this very well. And if somebody ever told me that I would, would be working with the dying would have called you a liar. You know, as a new grad, I was ICU, ER, feed them and street them, you know, as soon as they were excavated and sent into the floor, you know, as little as little interaction I could have was best. And then I got to see, I got put in my place.
Brian Ghafari-Naraghi 01:31:21
I got pru, pro, shown that this is what I was meant to do. Because it didn't bother me. You know, it's, I love doing the education. You know, I like taking the scariness out of it. You know, I want people to know what's coming. One of the things that people always worry about is that the death rattle. So, it's that that gurgling sound, right before somebody's getting ready to pass. Well, all that is, is you and I can clean our throat. So, what happens is, they're unable to clear their throat isn't painful to them, it doesn't cause them any distress. It just causes a weird, a bad sound. And so many people find comfort in that, you know, and it's like, Oh, yeah. So let me tell you how the pathophysiology of it. So let me tell you how this functions why this happened. You know, didn't we talk about the rally, you know, I always say, Don't be surprised if they, wake up one day, and there are old self and I said, that's a blessing. So those are the times you get to spend with the loved one. You know, and I've seen it happen with Alzheimer's patients. And I've seen it happen with all kinds of patients that the families get these sacred moments of, you know, I had a patient that wanted ham and beans. So, she called her the doctor called her best friend and said I need some ham and beans. So, her best friend whipped up some and ran up the hospital. And her daughter got to give her a bowl of ham and bean. Then I reflect on I had a 23-year-old that was dying in the hospital. And he wanted an orange crush soda. And the doctor said, no, he can't have it, too much sodium. And I was a night nurse, and I’m like bring him the orange crush soda. I’ll have to give him a little more fluids to offset the sodium. But you know, I have those orders but I could do that. Well, while mom was getting left to get the orange soda, a nurse brought him the nurse, orange soda. I was livid with that nurse. I'm like you took away that one thing that mom could do. So, we're all going to lie and this is your first drink of orange crush soda with your mom give it because, you know, my job is not to be a hero, it's not to be the savior, not, I am the calm in the storm. I'm the one that, it's gonna be okay. It might not be fun for a while. But everything's gonna work out. And we're gonna make sure we take the best care of them. And, you know, I tell people, I treat everybody like I would my mother. They get the same exact treatment that I would my mother. When my mother-in-law passed away. She was an old retired nurse, and she's going in for a valve replacement. Unfortunately, her heart was too weak to sew the valve in place. So, they told us that. You know, they gave us our options. And her husband looks at me and says, Brian, what are we deciding? And I'm like, Well, remember what Millie said she didn't want to stay on ventilators. And, you know, she, if it's her time, she wants to go peacefully. I was given strict instructions that if she woke up with beta dine on her skin, my ass is grass, because it was itchy. And I was a nurse and I've seen boobs before.
Brian Ghafari-Naraghi 01:36:06
You know, and this is a woman that when I first she hated me when I first met Danny, because she thought I made him gay. And we grew to appreciate each other over the years. Like, when my son had cancer, I was working six 12s to pay for his medicine, and she goes, I give you the money. I said, I do not take money from the devil. Because she had given Danny the down payment on the house that he had bought, or was living in. When we met when we bought our new house. We were gonna give her money back. Well, you know, it takes a little bit to get your money back. And she just kept after I want that five thousand dollars, and I'm like, so when she offered money, I'm like, Ah, you are the devil when it comes to money. And I don't want to owe you anything. This is my son. I will die before I take money. And you know, and I had instructions with her that I was not to let Danny and Carol fight her, her kids. Because they would I was not supposed to let her sisters act a fool because they would and they did. So, my job was to orchestrate her, the passing. And I I remember sitting in the room with Danny and Carol. And they got into a fight over should they let her sisters come back. And I I stopped, turned around and I said out and then he goes you heard him. He said you have to leave. That was for you too. Because your mom did not want this. I said go out, get get a drink. Take a deep breath. Get yourself together and then come back in as an adult. Because this is not what she'd want. And here's like oh my god. You know, it's like she my sister-in-law turns around and says is he serious? He goes dead serious. He goes he's not letting, he goes mom told us we couldn’t act a fool and we're fighting. So, you know, it's I've played referee with families before you know because death brings out all the dysfunction in the families. There's so much you know, I say there we call it there's fun in dysfunctional for a reason. Because it's entertaining. It can be a pain but it can be really entertaining. You know?
Brian Ghafari-Naraghi 01:39:16
Its, I was a bouncer at a friend of mines mom's funeral she her mom had mental illness, was crossing a Main Street at dusk, just as it was getting darker. She was hit and killed by a car. And so, I'm at the funeral. And I'm the only white guy, my friend is African American. And I'm standing next to the coffin with her mom, who, so, it was her grandma, my friend's grandma. And she started talking bad about her daughter. Because mental illness was not an excuse. She was a drunk. It's like, well, she was not self-medicating with alcohol because she had these problems. And so we're sitting in a casket, and she's just talking horribly about her daughter. And I said, I'm gonna stop you right there. She had her flaws. But this is not the time or place. So, if you can't hold your tongue, I'm gonna need you to leave. And she was sitting there, and who are you? I said, the guy telling you that you're going to be leaving if you keep causing a scene. And I just, my friends like, see he’s a bouncer, you know, but it was like, they needed that, you know, it's like, nobody was going to take control. And, you know, of course, she was never going to speak back to her grandmother.
Brian Ghafari-Naraghi 01:41:07
And it's like, it's like, when we got there, Jay and I got went there, we looked at looked at her mom, and in the cast for skirt was off, you know, it was turned to one side, so you can see the seam of her thigh. So, I'm like, and that was a problem for Jay. Jay is one of the people that when you dress you dress perfect, your shoes are white, you know, there's not a spot. I’m like ok, watch me, have my back. I adjust her skirt getting it turned right in the casket, because that was important to her, you know, its, I, I've started, I'm a collection of hands. I take it with permission of families with their loved ones hands. And I can send you some of the pictures that I just love because it's one of the last things they could do. I bought a stethoscope that I can record a heart sound on. And then I can transfer it over to a file. And I can put them in build their heart, or just send them a file on their phone or on the computer. You know, because it's, it's something that is comforting. I had a guy that was 16 years old, or the one that died on Valentine's Day. And I I'm still friends with his his parents. But he goes Brian, that heart got her through the worst time in her life. He goes, she would lay in bed and play his heartbeat. And I'm like, every every mother knows the sound of their child heartbeat. I said you could tell. They know, their child heartbeat. And like it's funny, I don't have any blood with my son. But I know his I know the sound of it. I know, you know is like I know when he's not breathing correctly. You know, it's like, these are things as a parent I know. And I can only imagine the bond between a mother and child when that mother carried him inside for nine months. You know, they felt the baby move. They felt the heartbeat, but you know, so giving them something that they could have as a memory or doing a hand in hand. A moment printed a hand or clipping of the hair. You know things that make it easier for them to get through the day.
Brian Ghafari-Naraghi 01:44:11
I had a young man that was killed on a motorcycle hit by a car. His mom was a nurse that worked at a hospital with in the metro area, and somehow I became their surrogate support person. So, I had to go to a funeral home when they were planning his funeral that I had, you know, and somebody's like, that's overstepping your bounds. And I'm like, no, because I'm there to provide support. I'm like, I taught a class before with ALS patients, help, I'm dying. I've never done this before. And why I did that class, I had a friend do one with the caregivers. And then we switch. And you know, it. It was just so neat for them. to be able to talk about it. You know, the funniest thing is, I was a palliative care nurse in the hospital, you know, I go talk to family about end of life. And I would meet the family in the hallway. And they would tell me, Mom doesn't know she's dying. Please don't use the word dying. Don't talk about dying don't. So, what I said, I won't use those words. But if she asked, I will not lie. Because, you know, I always talk about goals of care. And anytime you go to the doctor, you should have a goal of care. What, Why are you there? Because if you don't have a goal, why do you need to go to the doctor. But then I go in and talk with the patient. And the patient tells me, I know I'm dying. But don't tell my children, they can't handle it. And then I'm like, you know, you're both telling me this, right? I’m like it's, it's not that scary. It's part of life. I said, you know, if we could keep our mothers another 100 years, it still wouldn't be long enough. But we cherish the moments we have with them. And they live on in US. I have my mom's death stare according to my my siblings. My mom had this look that when you messed up, you knew you messed up. And I guess I have that look. Because it even says my older brother. But you know, it's it's that sacred family time and giving them permission to do things. Play music. I had another patient that, Martin was a character to say the least. Martin was gay. He had HIV. But then he also had lung cancer. And he had a twin sister. So, Martin was always causing havoc, just because he could. So, he had to have move out of his apartment. So, we got we had some hospice volunteers that we're gonna go over and help him pack. And these were young college girls that were going over to pack and I'm like, Martin, don't let them start packing in your bedroom until I get there. And of course, I had a patient get sick, so I had to stop off before going there. And I call Martin. I'm like, okay, Martin. Remember, don't let those girls in your bedroom. So, I get there and they're like, what's the rubber fist use for? He had a drawer of sex toys. I had to explain to them, I don't know if the girls were fascinated or horrified.
Brian Ghafari-Naraghi 01:48:54
But he just thought it was the funniest thing in the world. And his sister goes, of course he did. And then I get a call from his mom one time that he's running down one of the main streets naked as a jaybird. And she goes, I don't know what to do. I'm like, Okay, I'll be there. So I don't have, I have a black trash bag is all I have with me at the time. So, I go stop on the side of the road, put the trash bag on him, put him in my car and drive me back home. And, you know, then then he went to a facility. And he called me upset, because they were having a Cinco de Mayo party. And nobody was doing a margarita. It wasn't the fifth of May. It was July. So I went there and met his sister there. And he's like, they took all the decorations. They knew you guys were coming. But when I talked to Martin about, is there something you would like to do, like, you know, something you want to leave your family, he wanted to do make a set of wind chimes. Like, okay, I can do that. So, my husband was the vice principal of a school. So we got some copper pipe, and they cut it for me in links, put holes in it so that we can string it, we got beads, and they had the top made for it. So he got to make these wind chimes. And the day that Martin was dying, I was there with a family. And at first, we were all in the room. And he was just hanging on. And the wind chimes were in the dining room and I go, Margaret Ann, his twin, I said why don't you go in and lay with him. He came into this world with you. Maybe that's what he needs. After about 10 minutes inside, there's no wind, you know, there's no fans, the wind chimes, chime, and Margaret Ann comes out and says that he's gone. And that's what he needed. He needed it to be with his sister. And to this day Margaret Ann goes, You gave me such a wonderful gift. She goes, I've never thought about I came in, we came in the world together. She goes, I know he'll be there with when it's my turn, but I got to be there with him. She goes, he's in my arms. And you know, it's like, I get to make those moments happen. You know, and I tell everybody, you know, families always, like, want to take a picture of the nurse. And I'm like, you know, I prefer not to have a picture taken. Because I want to be that warm feeling. I don't want to be the person, I don't want to be the person because that's not my job. I'm not a character in this play. I'm the stage manager making sure that everything goes off correctly. And, you know, most people, accept that, I've had a few families that insisted I will do it. But you know, but, you know, it's truly not about me. And that's what I I always tell everybody. I I've helped several of our friends say goodbye to their parents. And I think, you know, it's such an honor. I get to make things better. I I can help. I can find ways of making a bad situation a little bit better. You know, there's always a rainbow after a storm. So, I would you just have to look sometimes a little harder, or there's a silver lining through stuff. You know, sometimes we have to read, refocus what we're talking about, you know, I hate when people say they lost the battle with cancer. Because sometimes it's a fight, you're not going to win. That's a battle that is impossible. The patient had cancer and they died of cancer. Because if a person really has the ability to fight that cancer, they would be alive. But some things are out of our control. And, you know, we just get to be there and support them and tell stories, you know, I get to hear stories I, you know, I always ask what's the funniest story, you know, most embarrassing story, funniest story. How'd you meet? You know, because somebody's always got a story, you know, every family has that one person in their family that does something or, you know, I have a whole family full of people that that I like to let them tell those stories. And it shows it shows them that they're valued. Because no one ever dies alone. I will set vigil with a patient before I let him die alone.
Brian Ghafari-Naraghi 01:55:12
Sometimes patients want to die alone. And I tell families don't you know, it is truly up to the patient. Because I had this one family that they have around the clock family with, with this guy. And two o'clock in the morning, his sister went to the bathroom. I said he doesnt want you to see him die. He was probably probably I said he probably probably said, Thank God, you guys are gone. Now I can make my exit. And she goes, That sounds like my brother. You know, it's being able to explain those things. You know, because I don't want there's no guilt. Nobody should feel guilty. Unless they did something really bad. Because a patient's gonna die. When it's when they're ready. I had a patient on hospice, that for all practical purposes, he had went two months without food or water. He was skin and bones. And, you know, we, we talked to the family about give him permission and, and oh, yeah, we’ve given him permission. Well, turns out the wife goes, anytime they were by themselves, because her son heard this, I can't live without you don't leave me. And we finally worked with her that she's gonna be okay. And we made sure you know, the son had a plan that mom was gonna move in, or he was gonna move to mom's house. And live with her because he was a single man. That way, she had her regular space and could function. And as soon as she gave him permission, he passed. You know, and, it's amazing to me. People see, see things that I believe they do. You know, people talk about seeing their loved one before they die, and, you know, I think heaven is a moment in time when we're more when we are at our happiest. If you ever have a chance to read the book, the five people you meet in heaven. It's one of the best books. There is, Tuesday with Maurey is Mitch Album is the writer. And everybody meets five people before they go to heaven. And you might not know, you might be one of those five people. But you might not have ever met that person. Yet, you might not have had, you know, like these kids are rolling tires down a hill. And it caused a car wreck. And they died. Well, that kid was tied to that death. But he didn't know that person. And you know, but it's just a really I find that comforting that have, you know, the pearly gates and all that. I don't know if I buy that. So I think heaven is when we're at a moment in time that we're the happiest you know, my mom and her best friend are in heaven, probably thrift shopping right now. These are these two women were nothing but trouble together. Judy lost her eyesight. My mom didn't drive because it scared to death Jeannie drove well they decided that when Judy lost her eyesight they could drive mom could me the eyes Judy can steer. I'm like, No. And, you know, it's like I don't I, I always do something in honor of somebody that passes, you know, I random act of kindness I Okay, a flowers to hand somebody looks like they're having a rough day or, you know, picking up the tab for, I was at the gas station, there was a police officer that came in to get a snack. I’ll pay it, Hes like you don’t have to do that. I said I know, but I had a friend that passed and I'm doing this in her honor, because sending flowers to a funeral, really, the family's not going to enjoy it because the funeral flowers. You know, it's like, I remember looking at them going, okay, I really don't want any of these flowers because there are funeral bouquets.
Brian Ghafari-Naraghi 02:00:50
You know, when I was with one hospice, we had a volunteer that with funeral flowers or wedding flowers, they could donate them. And this florist would arrange flowers for pay, our patients all had fresh flowers in the room. So, you know, what a great use of upcycling something that would have just ended up in the trash. You know, this woman that got married, just loved the idea. And she asked if she could deliver the flowers. She goes, I want to wear my wedding dresses and drop, because I know it sounds silly, but like, you know, everybody loved it. You know, it's like, who doesn't like a woman in her wedding dress? Because there's singing and they are happy, you know, it's it's a happy moment. And, you know, I've been with friends, I've been with enemies. And it means I, you know, taking care of people that repulsed me. But they get the same care. I don't. We had a guy that killed a little girl abducted her raped her killed her. And he was my patient. And people were going, I don't understand how you can take care of him. At the end of the day, he's a patient, he needs care. My job is not to judge. You know, my job is to provide care. Because, first of all, I don't want the responsibility of judging anybody. Yeah, what he did was repulsive. But I'm better than him. Because I'm going to treat him with dignity. Because that was the way I was raised. I don't know if this is anything that you're needing or wanting. I'm just rambling. So, if you want or need to redirect me, please do. Because I can talk about this for hours. I get, I love when I get to go to nursing schools, and do have in the life lecture. My nephew just graduated nursing school I gave the end of life lecture in the last semester for his class. But it's fun, because I love being able to educate people and being able to teach people about it not being scary, or how we can make it what can we do to make it not scary? What can we do to make things better? And, you know, I, it's, I'm blessed. You know, I always tell patients, it's an honor, a privilege, I get to care for them. I see it as a sacred time. And to be asked to be in an intimate moment of people you don't know. It's such an honor. And I don't want to do anything that would ruin that. You know, I have to admit, sometimes it doesn't turn out good. I've been called a murderer before, you know. But I know it's not me. I know it's grief. And that that goes back to don't spit on me and or hit me. We're good. You can call me any name you want. I'm cool with that because I understand you're losing control.
Brian Ghafari-Naraghi 02:04:58
You know sometimes you have to care for the spouse dying, or of the dying, too. I had a lady that I had to teach how to balance a checkbook. Because her husband did the bills all their lives. She had never written a check. So I started teaching her and, we got a volunteer to, there was an accountant that was showing her how to do do that. And that, to me, the family is the unit of care. And family is who's the patient says, his family. We're born with family, and we collect family along the way. And sometimes the family we collect are more important than the ones that are related to us by blood. And, you know, because I want people to be surrounded by love, at the end of the day. They were loved. No matter. My grandmother was a nightmare of a person. I loved her, despite everything she did. But, you know, it's like, I moved her into my house and cared for her for two months, or no, no, not two months, eight months. And by the second day, I was calling my best friend because nurse going, why can't I do this? This is what I was trained to do. I'm a nurse. And she goes, Brian. When you nurse, you get to go home at the end of the day. Because you get to go home, home is work. And it made me prioritize. Making time for myself. self care is not a bad thing. You know, and teaching families that it's okay, I need you to go home and take a shower. I want you to go get them to the you know, just get out of this hospital just for a few moments. I promise you that they won't be left alone. And my poor husband has been left at a bedside before when I couldn't find anybody else. Because he knows how passionate I am about and, you know, he volunteered with many a hospice patients. Arthur was my god Arthur was just a little he was an Irish guy. He looks like a little leprechaun. But he had heart disease. And he was on diuretic so he was peeing all the time. And he told me that our he told me that he was going to die pissing himself to death. He died on the commode. You know, it's like, we all had to chuckle about it. Because that's what he said.You know, and then I learned learn from a wise Chaplain when I first started in hospice, that sometimes what we do to care for a patient has nothing to do with the patient. Because I was going out to ride along with him, he's like, you might want to wear some jeans and shirts and bring some gloves. Like, why? Because you'll see when we get there. This man had a beautiful lawn, manicure, soft graph, but he had a walnut tree in his yard. And as walnut trees break down, they release an acid and burn the grass. So his spiritual distress was related to watching his lawn go bad. So the correct treatment for him was we went out and picked up walnuts. And, you know, it's like How simple is that? You know? Yeah, I'm just lucky. I it's and I find it funny because it parties, people will walk, you know, what, what do you do? I work with people that are dying. And they start walking, taking steps back like, you know, it's not contagious. But, you know, it's like, like, it's just so funny that, you know, people are so scared, and we're all gonna go through it. So It's the unknown. You know, once you make peace with the unknown, it's all good. You know, I remember being in a rough area that had a guy pulling down on me. And I looked at him and I said, do what you got to do. Good work God. I'm at peace. So if you can shoot me shoot me, because that's how, that's my end. But if you're not get the hell out of here. And he ran away, calling me a crazy white man. But you know, it's like, okay, you can't, the worst you could do is kill me. And I'm okay with that. Or with, you know, the, the, the Spirit the big guy or big girl in sky. I, I think of him as the genie from Aladdin. Because that makes makes me happy. And well, I'll tell you the one one more story than that I pulled off that I have no idea how I did this. So I had, it was a little Hispanic boy, the father was in the gang. So I had him at camp. So they were from East LA. They had just moved to the Midwest. And they went to camp for a week. So there's woods, there's a lake there, you know, we taught them how to fish. A friend of mine, Joyce has been taking her fishing club up there for twenty years, teaching kids to fish. And she used to say that I would she goes, we know not to let them hook or put the bait on the hook. Because you know what l wants to get stuck. And she goes, and Lord knows Brian will come down here and let us know. But Enrique ended up getting a bone marrow transplant. And I would go in and see him I was the night supervisor at the time. I found these handheld games that were like a fishing reel. So youd cast. And so him and I would fish in the room. And he goes, Brian, what do you think heavens like? And I don't know where I came up with this. But I was like, you know, when you first came to Camp, how you were nervous and scared. Didn't know what it was gonna be like, by the end of the week, you didn't want to leave. I think that's what happens like. And he he found comfort in that. And I have no idea where I pulled that out of. But, you know, I'm like, that was like, the nurse who was on the unit. She goes, That was a good analogy. How long did you practice it? I said, I just popped into my head. You know, it's like, I think we're just given. We make mistakes, you know, and that's, it's all about life. And living the life we have, and being appreciative of what we have and who's in our lives. You know, whether their four legged friends or two legged friends are, you know, we're, we're blessed. And I think being able to share these stories with you. I I know this is the first time we met, but I feel close to you because, you know, some of the most topics about my life. But I'm not afraid to talk, you know, and I there is a balance between when I'm working with a family and giving them enough to know that I understand but not giving them so much. It puts more stress on them. But you know, the power of presence is an amazing gift. I tell people you know sometimes you don't have to say anything. Just being there holding their hand or just you know Doing something. I remember one of the things that I started when I first started joining the hospices of clinical director, I went out and bought polish, nail polish and fingernail polish remover. And every one of my staff had polish a kit, kit with them. And didn't matter what your discipline was, would you like to nails polished if it was a female? People loved that. And I would have said that I, I started getting smelly lotion, you know, lavender lotions, and because we all want to feel good. And if we can give them that little bit of, you know, special moments.
Brian Ghafari-Naraghi 02:15:52
Right now, I'm watching a dear friend, I convinced, she was actually a recruiter, when I met her. She was recruited office staff when I was a clinical director. And I convinced her to come work for the hospice. And then, so I had a lady that was my volunteer coordinator, that part of orientation, everybody had to go out with every discipline. So, nurses went out with the social workers, the chaplains, bath aide, everybody in administration, because I wanted everybody to know what each one of us did. And so, I hired a volunteer coordinator. She comes in on the second day, being on the job and she goes, Brian, I can't do it. She goes, this is just too hard. And I, I had been to New Orleans. Prior to this, and I had this sign in my office, it says, Why don't you pull up your big girl panties and get over it? And Cindy goes, I can't, can't get over it. I’m like, okay. I appreciate your time. You know, thank you for bringing one experience to have and your gifts. This is not the right place for you. I want you to be in the right place. So, Veronica, who was my staffing coordinator, and like I said, you'd be really good as a volunteer coordinator. And she goes, I don't know the first thing about I said, well, let me see if I can do something. So, I called Cindy. And I said, I have a favor to ask. Would you be willing to kind of mentor Veronica was taking over the volunteer program? And, she was sure. After two weeks of mentoring Veronica, she asked me to come back. Because she saw her place in there, and it was it. It was her home. You know, my staff was I told people at my you know, we're a family. We're going to fight. It's going to be ugly at times. But at the end of the day, we love each other. And no matter what, some some day, somebody's gonna walk in and they had a bad day, and they're just gonna lay into you. And you give them grace. Because you're gonna be there someday. And Veronica, her mom had early onset Alzheimer's. And Veronica, remember, she goes, I just remembered her teaching her mom like music and dancing. So, she goes every Friday, and they play music and dance at the nursing home. And, you know, it's like, Veronica, she goes, Brian, I started doing it for her, but oh my god, I get so close. I get she goes, I get a connection that I wouldn't otherwise have. You know, and I'm like, nobody wants you to just stand there and stare at them. So, you know, play music, read a book, you know, but just be present. And, you know, when I’m with a patient, so the only thing that matters in the world I had a habit of looking at my watch. Not that I was looking. I was just curious what time it was. Not that I was in a hurry to go anywhere. But a family thought I was in a hurry. So, I started stopped wearing a watch. Because I didn't want them to ever think that I had somewhere else better to be and you know, there are a few times that, in life that, like when my son got married, my daughter got married. And when my daughter had her baby, well, my daughter had her baby during COVID. So, not very well, we could go up, but, you know, I, I know not to waste my sacred moments. But then again, if I can be there for something sacred moment, I'm gonna be there. And I'm lucky that my husband, and my children understand, and they give me the grace to do when to do this.
Brian Ghafari-Naraghi 02:21:28
You know, if I can make a situation a tiny bit better, if I could be that spark, or that sparkle in that dull day. You know, by giving them something to do like paint nails, I mean, I can empower people to give some, some comfort or some bonding, you know, playing card games, or I hate I hate playing board games, but I will sit down and play a board game. If that's what the patient wants, because, again, I'm there for them, and to take care of them and to help people. And that's what I found myself doing a lot. During COVID is, you know, I did all my research, I read everything the CDC, NIH, published, so that I could answer a question, you know, because I'm really scared. And I, let me just talk to you about it. You know, not too long ago, my my friend who's my eye doctor, she called me and she has a rheumatoid arthritis. And so, she's on an immunosuppressant. Her neighbor came over to let him let her know that his wife died of COVID. And it's like, okay, [inaudible] call your doctors see if you need to go on preventative, I said, Because I said, but would you be on an immunosuppressant. I would rather not take that chance with you. Or, you know. I went with more people that got the shots to hold hands. I've given that up for those shots. And I'm a smartass by nature. And typically, when I'm given a shot, I typically say something about, there's gonna be a little prick. But don't worry, that's your nerves. And by the time they are processed, what I said, I'm the needles done. And, you know, it's like, and they didn't feel it. And, you know, it's like, my mom hated getting her blood drawn. And so that's why I learned those tricks of like, okay, I'm gonna give you a shot, I want you to yawn for me, or cough. And if you're doing that, you can't tense your muscles up. So, it doesn't hurt as bad. You know, I've had the privilege to learn from some of the best nurses in the world. Because when I went to school, part of your night care, as a night nurse, is you gave a backrub you massage them. They don't do that anymore. And I was teaching my nephew because his dad's a nurse, his mom's a doctor, his aunt is a nurse, you know, it's like, this is what you need to do. And I said, I said, you know, I'm always appreciative of the nursing assistants because I was a nursing assistant. But for me, give me a bath is a great time to one doing a full body assessment and to just talk and sometimes it's nonsense. I'm not a big sports guy. But I can talk sports if I needed to. I got a talent of being able to BS my way through, you know, conversations to make them think I know enough, just but, you know, it's like what kind of music? And you know, when I'm working with somebody that's planning their funeral? What kind of music do you want at your funeral? What? What do you see your funeral looking like, I have a playlist for my celebration of life. And one day, I got to pair it down because it's getting to be over 500 songs because I hear a song and and some of them are inappropriate, and you know, to say the least, but they have good memories for me. I remember playing Cheeseburger in Paradise, as we move to comfort care on this, this woman that that was her and her uncle song. And they would just bellow it out. So, everybody in the room was bellowing that song. The other ICU, we gotten complaints from the other nurses that we were making too much noise, but like, sorry, this is this is our sacred moment. And sometimes sacred is not quiet. And, you know, that's the other thing is that I always tell people, people die as they live. So, like, I've always lived in chaos, because I've had a big family.
Brian Ghafari-Naraghi 02:27:31
It, to this day, I have to have if I'm studying, I have to have the TV on and the radio on. So, I had that different noises. Because that's how I learned to study. So, you know, it's like, if, if you if you're allowed family, then talk, interact, tell stories. If you're a quiet family, that's okay. You quietly say prayer or read a book, or you do something. But like, I just put myself in, in the fog of if I'm in that bed, wondering if everybody's standing around me being quiet. I'd be thinking something bad's happening. Because my family's noisy. I like to do a couple of exercises, when I work with nurses, or healthcare professionals. And one of them is called my diner. So, you have an eight by ten Nursing homeroom. You have a three-bedroom house that you've lived in for 25 years. What are the twenty items thirty items that you're going to take them with you and put in your room? What what what what would be what's something that's important to you that you'd want to be you want to see pictures of family? An Afghan? You know, but I think that it helps to make make it real. And I always tell people, I'm gonna make you cry. And I'm sorry. And then I'm like, well, not really, because that's the whole purpose of this. And then I have a story. And so, I have them. I tell people to write out body parts, either motion by people, by things that are important to them. So then I start reading the story. And it's about a woman that's been diagnosed with cancer. And I'll say, cross out two items. And I'm like that, so when a patient that's what they're losing. So, you know, it's like, I had I, I had one woman walk out and she goes, I have my five children down. How do I pick which five? I'm like, sometimes we don't have that luxury of walking out. I said I said, but you know now that's not your calling in life and that's okay. But you know, it's I try to express being real. I want, because it's so important to be authentic. And to meet people where they come from, you know? Do I want an alcoholic to keep drinking? No. But they find comfort in it? Sure? What is it gonna do, kill 'em? You know, I've watched I've seen people take illegal drugs. And I'm like, Well, if you're going for the high, let me know, because I can get, I can increase your pharmaceutical grade, which is safer. But like, if you want to do a psychedelic, okay?
Brian Ghafari-Naraghi 02:31:50
I’m like, do you have somebody to be there to be safe? And I've been there, I've been the person to be the one we took it. But it gives them that sense of freedom, not being tied down to or defined as a diagnosis. And, you know, I find myself and I know, it's inappropriate. But if I hear a nurse, talk about a patient, you know, the guy, this are the heart attack that room six. I'll stop and say, the heart attack and room six has a name, what is his name? Because I don't want you to make it, if it's me in that bed, I don't want I don't want to be defined as my illness, or, you know, disability. And, you know, one of the things that we talked about I, people die of suicide. And I try to get people to understand they died of suicide, didn't die of bleeding out. They, you know, they didn't kill themselves, it was suicide. And to be in that dark and deep hole. I can't imagine that, that's your only option. You know, and so my heart breaks for those people. And I've told people, I'd rather spend all night talking with you, than having to attend your funeral. Call me, I'm there. I'll be there on the worst night. Because I don't want you to, I don't want you to feel like they're alone. Because nobody should be alone. And, you know, I have a lot of family that I've adopted along the way because they didn't have anybody. But that was kind of my mom, she, she fed everybody. We were poor, but there was always enough. And, you know, I get to live my life that way. And, you know, there are times I want to quit. I asked myself, Why did I become a nurse because of the politics or, you know, fighting with insurance companies. And then I think, Oh, I'm here. Back on my wall, here are some of my patients. There's pictures of my some of my patients with with me, or, like I had a picture. Some of the parents would send me a picture and a note about their child. And those to me are my prized possessions because it's priceless. And to be thought of, a mom made these Christmas ornaments one year with she took his shirts and made flowers and put them in ornaments, and I have one and it's so meaningful. I have a I have a bobber over over there for Enrique because I did, at camp we did a little memorial service and By using the example because Enrique loved the fish, about the bobber in life, we kind of just float down, sometimes we get pulled down, but we're all gonna be pulled back up, probably gonna pop back up and just kind of have faith that, you know, bad things happen. But that's part of life. And I would never trade, the bad things that occurred in my life because they made me who I am. They keep me humble, they keep me grounded. And what a great way to live life. You know, it's, it's an about who has the most junk at the end of it. But I do have a lot of junk. raising two kids, our parents dying 27 years together. You get a lot of junk. But I keep telling my son, you know, I'm not worried about it, it's gonna be your problem. But on a side note, my son nominated us for a show that they're going to be taping it over in Sweden, they have what they called Swedish death cleaning. So, you, you start cleaning your house to prepare for your death. I'm pretty sure as long as I pass the psychological evaluation, we're on the show. I've horrified that I'm going to be on the show. Danny's a, he is my extrovert. He's my flower. I'm like, oh, god, okay. But I said, there are rooms that they can't come into. Because these are my sacred spaces. Like, there's a line in my hallway, that nobody can go past that, because that that's my safe space. And, you know, that's, I think, part of my success of being able to do what I do, you know, because, you know, it's like, I write on a canvas, like, a patient's name that passes. So, I have years of starting back in 2010 of canvases that I've written their name on. Because, you know, I always say, you want to say their name, because that's the worst thing that can happen to somebody to be forgotten. And, you know, it's like, I, it's amazing how many people are afraid to talk to somebody, especially after they have a child that died. They don't want to say their name because they don't want to put them on. But then you lose, you know, part of that child dies as you don't acknowledge their existence. Or, you know, I, I try to correct parents when they say I have two children and, and one that passed. No, you have three children, two are living one is deceased, but you still have three children. Right? It doesn't change. Whether it's a day that you have with them, or lifetime. It's still important. My one last story when I was a night charge nurse in the large teaching hospital, I traumatize two units, all at the same time. So, we had a woman that was in a car wreck, she was 38 weeks pregnant. We knew the baby wasn't gonna make it. And there was question whether the mom was going to make it. So, I get my NICU nurses to bring the baby downstairs to the adult ICU. And we take pictures of mom holding the baby because I wanted that mom to have, she wouldn't remember it. But I, you know, and I hope they go What if she doesn't want them, then we throw them away. And that's something that you know, I can't recreate. So, my adult nurses were horrified by seeing the dead baby, and my pediatric nurses are horrified by seeing the sick adult. But, you know, it's like, but they still talk about it to this day. You know, it's like, what an amazing, I wouldn't have thought of that. It's like, you know, I tried to think of what I would want, you know, it's like, and I laugh because I never wanted children. And I have two, and I love them. But I never want them. Because you worry all the time. You know, it's like, now now, grandbabies. The worry, just continue is the new stages of worry. If I have a blessed life, I'm just so lucky. So that's kind of my story.
Kit Heintzman 02:42:01
I'm so curious. I think that the last two years for many has been an exposure to mass death that they haven't had before. Coming to it with your experience of so much death. Tell me something about what it felt like to be, to have deaths or around everyone for some of whom it felt kind of new.
Brian Ghafari-Naraghi 02:42:31
Well, I had that was a group of a population of people that I've never seen. But, you know, I never thought about as, as a death doula, you know, I’m thinking, I'm working with a family, somebody has a life limiting illness. But this got me thinking, I was talking to my friend who was a social worker, she moved to France, right before COVID started. And we started talking one day about you know, peoples need so we started posting on, on Facebook or on Instagram, if you need to talk. I'm here. And, you know, it's like, what do you charge? Nothing. Because, you know, it's like, it wouldn't be nice to make a living at it one day, but, there's no pair source for it. So, people wouldn't get it. So, it's how I give back to make my community better. You know its. Watching, I had a patient, that ALS patients that recently passed, and it was pretty sudden, and I got really close with him and his wife. He was a big governor of the university. So yeah, VIP. And my first introduction to him was he asked me, he told me I was gonna give him my cell phone. No, I don't know you, I don't give my cell phone out right away. And we kind of bonded over that. And when he died, his wife goes, Brian, I have this, these three wheelchairs that are in perfect shape. I said, Well, you could sell them. Or, if you want, you can donate them, and we can use them on patients that don't have the resources. And she did and the perfect patient got the perfect wheelchair. It was so amazing. Because this guy was six, five, and he's six, six. So those big wheelchairs are hard to find. And, you know, if I can make somebody's life a little easier, then I have you know, or laugh until they pee their pants. It's been a good day. I describe myself as I tell everyone, I’m a little bit crazy, you know, the best of us are you know, which helped me You know, one of the things that you learn early to have kind of a twisted sense of humor as an ICU nurse. And there's one, one shift, I come home and I won100 bucks. We had two patients actively dying. And we, we were betting on time. You know, and it was totally inappropriate. But it was the way we survived that shift. You know, do you know, I have, I have a collection of skeletons and coffins. And because after I got my masters people thought it was funny. And now I, I kind of like it. I have a large book, collection of death and dying grief and bereavement. And it's, it's a loaner library, I will loan out any other books or, you know, like, if I've worked with a family or friend or a patient, here, this might be helpful for you. And, you know, I had a patient or a husband, when I suggested that, he couldn't read. And I don't like the sound of my voice. You know, I just, but I have, I have a friend who has a beautiful voice. She could read the phone book, and it would sound good. So, she recorded it, she read the book, and we were able to give him the book where he could listen to it. And, you know, I love that aspect. Because I get to be creative. I get to MacGyver a lot of things. To make them work. I, I do have my stockpile of medical supplies that I that people give me and they're in my garage and drives my husband crazy. But, you know, somebody always needs them. And, you know, it's like, I have a wheelchair in my garage that just got returned, because my friend’s cousin had had surgery and needed a wheelchair for a month. And it was gonna cost him over $500 to rent it. And it's like, okay, it takes up a little space, I can hold on to it. And I joke about my nurses network of, if I don't have something, I have friends that I can call and say, Hey, do you know where I can find? Because, you know, some of the best nurses hold on to that stuff, because we know we're gonna need it.
Brian Ghafari-Naraghi 02:49:09
Yeah, I being able to support people during COVID has been a blessing. You know, I could easily become a hermit. Give me a book and a blanket and I can be lost for hours. But having to zoom or FaceTime with people to talk and sometimes it's just they just need to say it. You know, you have to name it. And once you name it, it's okay. You know, I've dealt with people who have never dealt with death in their life, and they were in their 40s. I was very thankful, you know, thinking back I'm thankful my mom took me to a funeral at five because I was exposed to it. It wasn't you know; it wasn't unusual for me. And, you know, being able to, to provide mementos or our keepsakes, so important. It cost nothing for me to do some of this stuff. And if it does cost me money, I come from the belief. You give what you have, and everything works out in the end. You cant take it with you. But I can actually say I love working in the death industry. I am mentoring a funeral director from Nairobi. She is interested in starting, like hospice in the life and the doula stuff. So, she reached out, kind of like you did on on my Doula page, and she goes, would you help teach me? Absolutely. She said, what do you charge? I said, if you can do something, give me something, you know, a decoration that is traditional for your country like, a little box or, you know, a little basket. Because those things, I have mean more to me than some of the things that we've spent tons of money on, because there's a story about them. And, you know, when I have bad days, I look at those things, and they get me through my days. Luckily, I don't have very many bad days, they do come, you know its. When my first friend, this was a nurse that died of COVID That was a kick in the stomach. And the sad part was, she was supposed to retire, retire, and then talked her into working one more month. And she died two weeks after she was supposed to retire. And, you know, I know she wouldn't be sorry for it. I felt horrible for her family. But you know, I always run towards danger. You know, they do active shooter training. And it's run, hide, fight. And I told them, and they're like, if somebody's shot, you step over. And I said, not going to happen. I said, its too ingrained in me to help somebody I, I beat the dumb person running after the shooter to tell you how they got me. At least I can mitigate multiple people because I'm just one person, you know, and I do what little I can. But you know, I cover this thing on Facebook that I saw one time that said, what if the person that had knows the cure for cancer isn't able to go to college? So as you know, I might be able to do this but somebody else might be able to do something that will change the world and I get to change the world a little bit at a time. You know. That's fine with me because that goes back to by working behind the scenes
Kit Heintzman 02:54:57
What are some of the ways that you've been taking care of yourself recently?
Brian Ghafari-Naraghi 02:55:02
Family time, massage, I paint. I started painting abstracts and part of it is I have chronic migraine. So I started painting what I see. But I also paint colors that I see around patients or feelings that I get from patients. I will kind of paint it out like it splattered across the canvas or you know I garden, but my friends and my family are my, my gift they're the one make it where I can do what I do.
Kit Heintzman 02:55:57
What's it been like negotiating your needs with your family, during COVID needs for safety you would mentioned being a homebody or husband more extroverted. How have you been navigating all of them?
Brian Ghafari-Naraghi 02:56:13
You know, you're just at the end of the day, it goes back to that you pull up your big girl panties and get over it, you know, life life goes on. Sometimes life sucks. And sometimes, you know, it's not what I would expect or hope for. A gift my mom always taught me is that there's always a silver lining. So I got closer with my husband during COVID You know, I got to share time with my my son and daughter in law, you know? So, you know, it's like I had time to do some genealogy research, or just stuff that I would consider wasting time in my normal everyday life I tend to just be lazy watch TV for one day I watch movies all day. So, I get it you know, I didn't have to feel guilty and you know, it's like I still mask when I'm out in public because I was working with ALS patients and I couldn't risk carrying something to one of them and because I wouldn't have been able to live with myself. Yes, it's uncomfortable. Yes, I don't like them. But a little bit of uncomfortable-ness to keep people safe. Not a bad thing. How about you what do you do to take care of yourself during COVID?
Kit Heintzman 02:58:08
I took up meditation.
Brian Ghafari-Naraghi 02:58:12
Well, I can only imagine this project is bringing up a lot of emotions.
Kit Heintzman 02:58:23
It does, um the primary one is actually gratitude. I am so grateful any anyone chooses to have this conversation with me.
Brian Ghafari-Naraghi 02:58:37
And know, you're always welcome to call me if you're having a bad day. I'm here I don't mind talking because that's how we're gonna get to get through this together that's the only way is we got to do it as a community and you know it's not ideal you know the world has changed and who knows if it'll go back to the same way, but I think it's a chance to learn and grow.
Kit Heintzman 02:59:27
How are you feeling about the immediate future?
Brian Ghafari-Naraghi 02:59:32
I'm positive I'm realistic I'm I'm afraid there's gonna be another surge, but I know we can handle it and you know it's all gonna work out me and one way or the other. And it might not be the way I want it to work out. But again, its not my play book.
Kit Heintzman 03:00:10
What are some of your hopes for a longer-term future?
Brian Ghafari-Naraghi 03:00:16
Oh, I love to see us, as a country, come together and help more people you know, or to learn from this, although, after watching Roe, Roe v. Wade, like okay, please don't repeat, we need to grow. But I am hopeful You know, one of the things that a lot of people talk about the millennials being entitled, but they're better at setting boundaries. You know, I was Gen X we suck it up and do it you know, keep on pushing through. And sometimes it's not bad to say, hey, I need a break. And, you know, it's I like to I do a lot of thinking and a lot of what ifs are kind of interesting and fun. But, you know, it's like, what if we don't do this? You know? I read I read the leaked Roe vs. Wade document. And they talked about domestic product, babies. And that's how they refer to them. And I'm like, okay, that's not okay. They're not a widget, but I think technology is making us lazier. And gentle, it's, I'm, I'm happy to be able to share as a they, they say old timers’ ways of doing things. Like, I don't need an IV pump to give medicine. I can count drips. I said, I can do so much without the monitor because I have those skills. And I'm grateful that I have those skills and being able to teach my nephew some of those tricks and tips. You know, because I really love old farm recipes or the old neighborhood mom. You know, like, for constipation I learned this years ago, you take two apples two oranges, a couple raisons. Put them in a blender with orange juice, till the top. You blend that down. You haven't drink three out of the first day and announced every day and they go regularly and there's no chemicals. I try not because I don't like medicines, you know because to get put on one medicine then you have to look for the side effect and. Thank you for letting me tell my story.
Kit Heintzman 03:04:04
Thank you so much for telling it.
Brian Ghafari-Naraghi 03:04:09
Hopefully it's something that was meaningful. You know, I think what I do is not special. Because because it's what what I'm supposed to do. You know? You know? I'm very humble about what, you know. I like my I get uncomfortable. I have a family that called me, Oh youre such an angel. No, I'm a nurse because it's like a whole different level of who I don't you know, it's like I was I do it was like you know, it's like it was just how I was raised, I had an amazing mom. I’m gonna, hold on just a second. Change my air buds, just a moment [inaudible]
Kit Heintzman 03:05:32
I can still hear you.
Brian Ghafari-Naraghi 03:05:39
[inaudible] what do you make of this?
Kit Heintzman 03:05:44
You dropped in and out there.
Brian Ghafari-Naraghi 03:05:44
Oh, I look forward to seeing what what I always thought to be interesting is to document nurses story. Know, in the twenty two years that I've been doing this just something just changed,[inaudible] I remember cus, they were being clinically trialed that were standard care. And, you know, it's like, I, when I was a volunteer, years ago, this nurse must have been nine, she worked her cap in our cape, she had a white starch uniform every day. And I think, well, I don't have to wear white, because I'm a dirt magnet., but it's like, just to see how far we've, we've come in critical thinking and, you know, anticipating being proactive, I think is amazing. So, I'm hopeful for the future. You know, what, that was one of the things that I enjoyed with Danny's getting a school superintendent, I get to meet some amazing kids turned into amazing adults. And, you know, that's what's going to change our world, is these bright, bright minds that would not traditionally have the chance.
Kit Heintzman 03:07:43
What would you want historians listening to this, to know about this moment that they might not know because they weren't here?
Brian Ghafari-Naraghi 03:07:51
We're resilient. No matter what, we're always gonna make it back. And the harder you, you make it, we're gonna push back harder. Because that's what we do. You know, I was raised, defeat is not have an option. Now your goals change, might change. But you're never beat, you never lose. Because you can always grow. And, you know, I think that we learned a lot about people during COVID, you know, some good, some bad. We've seen the good, the best and the worst of people. And, but we're still making it through, you know, we're still, We're surviving, and thriving, you know, in some ways, you know, because it's more than just surviving, we got to thrive. And we're growing and, you know, watching that vaccine be developed and knowing that it's been in development for three years prior to this is exciting. And, you know, to watch stuff that okay, we're gonna try this, you know, might not work. But, you know, one of the things that popped in my mind is I worked with muscular dystrophy and spinal muscular atrophy is a disease that was a terminal diagnosis. And actually, our my son's best friend in high school had it. Now they can do gene therapy, because they test at birth, and they can do this gene therapy. injection into their spine, and they can be normal kids. 20 years ago, that's unheard of. And I think we're just going to learn more and more. Yeah, it's, I just read about high schooler that develops sutures that change color when there's an infection. You know its like, what a simple idea. There's so much, University of Missouri where I was at just open this physician Research Building, called the next gem. So they have are bringing in the brightest for medical advancements and just watching it get built, my boss was the lead in that and, you know, him developing, getting in the right people in the right places. You know, it's like, like, I joke with him, I'm like, I did get to ride your coattails for a little bit. But you know, the thing that I think, like I keep coming back to is we're going to make it through will not be a little little worse for the wet. And, you know, I might need to learn to dress better again. I never used to wear sweatpants. So, I think that's pretty much what I wear but, yeah, you know, just looking over the last 100 years, the developments and how we've grown in, in our knowledge in our emotions. How we know how to we look, we're learning how to better to care for each other. And, you know, there's somethings that I don't understand. But I tried to learn, you know, it's like, sometimes I just don't know. But hey, it's always that's the thing about like, life is a learning opportunity always. And I think once you stop learning you die.
Kit Heintzman 03:12:43
I want to thank you so much. Those are all the questions I know how to ask right now.
Brian Ghafari-Naraghi 03:12:49
Ok.
Kit Heintzman 03:12:50
At this point, I just want to open some space. If there's anything you'd like to say that I haven't made room for. Please do so.
Brian Ghafari-Naraghi 03:12:57
Oh, I think youve just let me ramble on. But ya know, I had so much fun talking to you. And if you have more questions later on, hit me up. Or if you get overwhelmed. Hearing all the stories. And you need a safe place, I'm here.
Kit Heintzman 03:13:16
I really appreciate that. Thank you.
Brian Ghafari-Naraghi 03:13:19
No problem. Have a great night.
Kit Heintzman 03:13:21
You too.
Hi, I'm Brian Ghafari. Today is May 18, 2022. It's 3:56 in the afternoon, Central Time.
Kit Heintzman 00:11
And where are you located?
Brian Ghafari-Naraghi 00:13
In Kansas City, Missouri.
Kit Heintzman 00:16
And do you consent to having this interview recorded, digitally uploaded and publicly released under a Creative Commons license attribution noncommercial sharealike?
Brian Ghafari-Naraghi 00:27
Yes.
Kit Heintzman 00:28
Could I just ask you to start by introducing yourself to anyone who might find themselves listening to this?
Brian Ghafari-Naraghi 00:34
Okay, my name is Brian Ghafari, actually Ghafari-Naraghi, but I just go by Ghafari. I am a registered nurse with over 25 years of experience. I hold a Master's in the Life Care, a bachelor's in nursing and associate nursing. I have completed my doula training...end of life doula training. I am do some grief counseling that I was trained for. And a little bit of this, a little bit of that in the medical field. Before my previous job, I was working with ALS patients and Case Manager. Now I'm going to be doing clinical research. Now I'm going to be doing clinical research on psychedelics that pays the bills, so that I could do my doula stuff.
Kit Heintzman 01:35
Tell me a story about your life during the pandemic.
Brian Ghafari-Naraghi 01:42
I'm a homebody. So, you know, stay at home was not not a problem for me. Now, my spouse on the other hand, he likes to be out and about and it was driving him crazy. I started the pandemic out by being like, one of my jobs because I worked for organ transplants. And I was working for an organ recovery organization working with families and helping manage patients in the ICU before recovery surgery. Due to COVID We we've dropped our patient load so then they release some of us so we weren't so many of us. I worked for an insurance company for a while. I was told I was going to be a case manager, our navigator for oncology patients ended up determining our declining authorizations for medications and it sucked my soul. During all this I work end of life. I work with families, I work with patients. I am a doula. So, if you're familiar with like a birth doula where they have a birth plan, we do the exact same thing, but it's the opposite end. So, we have a death plan. So that we can identify what are their fears. I always give the example of pain, I can tolerate pain. I don't want to be nauseous. That is one of those symptoms that freaks me out. But pain is okay. So you know, it's like, so identifying what is important to the patient or, you know, how much sedation are there we're getting, give them because do they want to be able to talk to somebody, you know, if we give them this medicine or I have had some great in the life educators, Paul (unknown spelling) my mentor for my college program at George Washington in the Life Care. Jesse Roberts was a medical director of one of the hospices. Maureen (unknown spelling) was the Medical Director of the part of Care team at one of the hospitals and Karen Williamson was another medical director. So I had some great teachers and nurses. And then of course, social workers chaplains which makes it all so much easier because we it's amazing how many questions I got asked about spirituality but God about pain I actually started my journey on my interest in end of life care because I was working in the emergency room and in a burn ICU right out of nursing school, as a new graduate get all the dying patients which I ended up liking because I had my colleagues gave me that would be my only patient and Instead of having two patients, I would just have one. And I got to do a lot of teaching and a lot of education, a lot of preps about what to expect. And I really enjoyed just having those tough conversations. Because nobody wants to make at the last minute, you know, it's like you're setting in the ICU, then people walking in, what have you, have you ever talked about end of life? Now, my family, when we have like Thanksgiving or Christmas, we invite anybody who doesn't have a place to come. And my kids always warn them that I'm going to ask about end of life wishes. And my kids are in the 30s. And some of their friends are in the 20s. And they're like, well, but I'm not gonna die anytime soon. You don't know that. I said, I could walk across the street and get hit by a bus tomorrow. So, you know, letting your wishes known is a gift you can give your loved ones. So, you know that and I get to hear stories. I I have the honor of caring for patients from World War One, World War Two, Korea, Vietnam, Desert Storm, Enduring Freedom. So, you know, it was amazing. I met one of the first Rockettes.
Brian Ghafari-Naraghi 06:28
And then, you know, just getting to let them tell their stories. One of my favorite questions to ask is, if it's a married couple, how did you meet and who decided this is the one for me. I've got some crazy answers. I had one lady that told me she goes, I was on the bus. And this nice-looking young man got on the bus and she said he was going to off to war, would you want to get married? She goes, I said, Yes. And we've spent our honeymoon in the back of a gas station, we shared a bowl of ice cream. And everybody told him that their wedding or their relationship would not last. And she said 76 years. Together, all their friends had died, who said so they outlive their marriage outlived their friends. But they always had ice cream. They're on their wedding anniversary. So, you know, the oral history that I get to hear is amazing. It's very sacred to me. Because I'm getting in on the one of the most intimate times in somebody's life. You learn things about people, I had a lady that was 96 years old. And she confessed to me two days before she died, but she had an abortion when she was 16. And, you know, you think about that with Roe versus Wade nowadays. And it didn't take effect until 72-73. So, she just went to some closet. And she had not told anybody in her entire life. I was the first person so I just, you know, it's I don't shy away from things that are hard. I think that's, you know, most of my nursing career I've worked with difficult patient populations because they need somebody to be their voice, they need somebody to be there to care for him. You know, I have been witness to people passing. We may I've had help celebrating the lives of my patients. I had a patient that was in a car wreck. He was 16. And she finally was determined brain dead on February 14, which is National Heart donation day, which is Valentine's Day. So, before mom got there, mom and dad got there, I got some red heart lights, and a little bit food decorations and made a little special for 'em and, you know, it's those things that are fun. And, you know, or helping somebody understand that. You don't have to take that next treatment. You know. I'm like, let's talk about let's let me explain to you what it's going to look like. Especially like when it comes to DNRs or Do Not Resuscitate orders. I prefer AMD, which is allow natural death. Because to me, that's what we're doing. We're not withdrawing anything, we're just making them comfortable. But I, you know, had those hard conversations about, about that COVID opened up, a lot of people reached out to me because they were scared, they were grieving, you know, the loss of jobs, the loss of independence, the loss of, you know, being able to meet with friends, you love, so many people, so many things, that, you know, we weren't able to they couldn't find somebody that would specialize in that, you know, it's like, or the, they didn't know what to call it. So, you know, it's, I have a friend, that's a social worker. And, if, and if it was to, she's a therapist, and if there was too deep for me, I pass it on to Andy. But, you know, it's like, whatever I could do to help. And I'm still doing it now.
Brian Ghafari-Naraghi 11:19
We're getting ready to start a death cafe here in Kansas City. It's adaptive K, cafe, they started over in Europe. And it's just a meeting where a group of people get together, we're here, they actually be in a brewery, because that's who volunteered to host us. And we're going to talk about death. And I, I tell people I talked about death to take the power away. Because death is the unknown is unknown. And the unknown is scary. So, if we can talk about it, and take that, that ability to be scared. You know, it's, it's, it's a, it's a very freeing, because I remember that's the point that I realized, Okay, I'm gonna die. You know, it's, that's just part of life. You know, life isn't terminal illness. So, you know, I volunteer with help homeless, boats with, with the street medicine group. I volunteer a lot of as a doula volunteer in school schools around town, but I just like giving back to the community. You know, I tried to leave it a little better for better than I find it is, what is my goal and for each day
Kit Heintzman 13:02
I'd love to go back to the subject of patient autonomy and ask how you feel about that, how your ideas have changed over time and how you share that with your patients and clients.
Brian Ghafari-Naraghi 13:19
You know, it's funny, because I always believed in autonomy. Growing up, I, I remember going to a funeral at age of five, because my mom thought that's part of life. You should experience it you should not have. And so, it was never really...yeah, open caskets still kind of freaked me out. This is just they don't look normal. They don't look natural, you know, and everybody goes, Oh, they look so natural. No, they're kind of a theme. Like wax figures. But when I able to sit down with the patient, and as I see the generations go before the baby boomers, my great grandparents. So, my great grandmother had a pacemaker placed at the age of 96. The cardiologist told her that she needed to change the way she's eaten, because she fried everything in lard, butter on everything. You know, lots of unhealthy dietary stuff. But she was only four foot 10 And maybe maybe 95 pounds. But I told him she was so scared. She didn't know what to eat. And I said, let me come to you come with you to the next doctor's appointment. So, I did and at first she was a little embarrassed because I was talking back to the doctor. How dare I talk back to a doctor? And I'm like, no, this is this is your choice. I said, honestly, I said, if we draw everybody's cholesterol, you probably have the lowest cholesterol of the three of us. Because her body is probably used, you know, she's done it for 96 years, nothing's going to change overnight. So. So that was my first time being able to advocate for somebody. And then my next chance was my great grandmother on my father's side. And we were all sitting around. And they told us that she would probably never get off the ventilator, we could keep her on the ventilator to her feeding to. And my grandfather, her son said, that sounds good. I said, I was probably sixteen at the time. And I said, is that what she'd want? Like? She's a big Royals fan. And loved Royals, love go into the game, you know? And I'm like, she won't be able to do any of that. So laying the bed. And he goes, Oh, I didn't think about that. That I said, you know, for some reason, when I came of age is the AIDS crisis started, and I remember being 15 years old, voluntary, at a Catholic hospital. And I was taking trash back to the to the utility room and in the hallway in front of the jury utility room with a patient on it on a gurney. And I walked over to him and I said, what happened? Why are you back here? And I touched him, and he goes, Oh, you don't want to touch me. I'm like, Why? Because I have AIDS. I said, Well, you know, this, this is why I look at your skin's intact, my skins intact. I don't think I don't think I'm okay. I think I'm okay. So, then I started volunteering as a home health aide and taking care of people getting them in the showers when I was in high school, because, you know, nobody wanted to do it. You know, and being a gay man, scared scared me to death. You know, at one point, I thought that that was, you know, I was gonna get AIDS and die. Because that was in the early 80s, early to mid-80s. That's what happened. And now it's a chronic condition. But, you know, the stigma is still there. And having patient being able to encourage patients to express their wishes, is so rewarding. And again, it's that sacredness of being able to be part of, I'm part of the family, but I'm not, you know, because you don't talk about things like that with strangers. And, you know, when I sit down with a family, it's like, we're gonna talk about some hard things. We're gonna talk about funny things.
Brian Ghafari-Naraghi 18:27
I said, I'm gonna mix it all up. Because death to me, is kind of funny, you know, and as a hospital, hospice director, I went on a on a death call. And I first time meeting this patient, I go back and check her pulse did all my assessment and yet she was dead. I come back. All right, go back into the living room, sat down, start to explain to the family and I hear this uhhhh. So I get this panic look, you know, not panic, but it's like, Oh, my God, I totally missed something. So I excused myself went back to the bedroom. Listen for two minutes with my stethoscope did reflect nothing, walked back out, sat down and started talking to get in and heard the same noise. And at that point, the family goes oh, we have an asthmatic dog that's under the bed. (laughs) So you know...you find you, you know, I think when if you can find humor in the hardest part that makes it so much easier. You know? The first thing I tell people is if you think you have anything under control, that's your first mistake. Because everything's gonna happen no No matter how well we plan, we plan, and I always tell patients, I said, ?I got a through z backup plans. Because nobody's going, I said, if I tell you this is going to happen, something opposite is going to happen. So we'll, we'll be prepared. But letting you know what I'm talking about Golden care. Work with the wonderful oncologist, just one of the best people in the world. But he would give a rock chemo, if they asked. And it's like, why are you giving them chemo? We know, the chances of survival are 5%. So, we're taking what they see have the chicken feel healthy, and making her sick. So, to me, those are days that she can go out and have ice cream with their kids or go to the park or you know, do something that is not being sick in a bed. You know, I as an ICU nurse, I, we kept patients alive because we could. I remember a patient that had meningitis, and she had been in the hospital for three months. And I was getting ready to leave shift and I walked in to hanging in a bag of fluid. And I'm like, God, this room is hot. And I'm like, wait a second. I'm only hot on my left side, which is the side that's closest to the patient's like turn to face the patient. And it was like opening an oven door to the temperature 106. So, our fellow came in, looked at it. First thing he said is let's get the Echo, the heartland bypass. So we won't need the patient. Like, you know, it's like we're taking away her ability to die with dignity. You know? And it was funny because her husband I, I saw six years later, and I was having questions about should I be a nurse? You know, was it worth it? And he goes, you made the world of difference to us. He goes, we were able to make choices because we were informed. And General. One thing my mom taught me is knowledge is power. So, you know, it's explaining things to people.
Brian Ghafari-Naraghi 22:57
The DNR Rs, if you ever watch any TV shows, you will see a patient go into cardiac arrest. And they do a couple tests compressions. They give a couple injections of meds and, and they talk them once or twice and in 15 minutes, they're setting up and talking. Well, that's not reality. In reality, what it is what happens is we push on the chest, we break ribs, we bruise the muscles. It's painful. And if we get a rhythm back, it, we might not be sure that they don't have any brain damage for 72 hours. So, you know, it's a good friend of my mom, or a good friend of ours, her mom had lung cancer. And Mommy didn't want to listen to anybody. And she knew that she was going to die. And of course, she wanted somebody to do everything to save her life. And so, it was funny because our friend was my partner Secretary when he was a school superintendent. And both of them were older than me. And mommy says, you too need to leave grown people need to talk. So we just talked about what it would look like. And she goes, Oh, that's horrible. I get asked that. And I'm like, well, but you know, for some people that's important. It's not the quality. It's the quantity. You know, it's and I said that's a very personal decision. How do you know my husband and I don't say I die. If a cancer and I don't have a bit, if it's a 50/50 chance of survival, I'm gonna go live it up. I'm gonna spend every day my hands, do things that I would never do before, you know, because I don't want to be sick. And sitting in his chair, I seen that too much. But when you're able to empower patients by education, it's it's like a proud parent, you know, it's like, you get you see them, talk back to the doctor, but more question them and ask them. Why are you suggesting this when that x, y and z could happen? And isn't XYZ worse than what this is. And it's amazing by having that knowledge and that power. Because, you know, when you go into the hospital, they take away everything down to your underwear. They take all your clothes, if you're a woman, they take away your makeup. You're lucky if you get to keep your glasses in your teeth. You're stuck in a bed, and you're at the mercy of nurses and personal assistants. And I know that everybody means well, but sometimes they're just too busy. And sadly, patients don't get the care they need. You know, I, I tell people that if you have a loved one in the hospital, somebody needs to be there to be their advocate. And like when I would do teach them with my ALS patients, or my oncology patients, the first thing I would tell or after we were done with my teaching, and I would have that brief down to thirty minutes. I would tell just, that was my initial teaching. And I might if you remember three percent of what I said today. I did I had a really good day. I said, here's my number, so that you can call back when you're at home. And it's like, Oh, I forgot that. To ask this question. And you know, it. It's empowering to the patients. Because I remember my son when he was fourteen year old, fifteen years old had Hodgkin's lymphoma. And I remember sitting in the doctor's office, and it was at the hospital, I worked at the they said the pathologist is going to come in and talk to you. Well, the pathologist walks in, and she was the wife of the Burton fellow. And I knew she did oncology. And so, I immediately reached for the trash can. And both my son and husband are looking at me, like I lost my mind. And I'm like, it's cancer. And it's like, okay, let's slow down and think about this and and then we got through it. My son, you know, at that pre for that teenage years, you know, not as kid not as adult, but in that if he stage and I told him that, if you want me to treat you like a grown up, you need to know what teenagers are hanging the side effects, which order it goes in. Because he he got like, eight different drugs and certain drugs had to be given before others and he caught a mistake. Because he was told that, you know, he he didn't miss on school that year. Because, you know, that wasn't his school counselor. I'm a nurse. So, you know, it's like, you know, people have it worse. You gotta keep going. And he's still with us today. And he goes, You could have let me slack off just a little bit. Like no, because you're here to pitch about it now.I did my job so, you know, just being able to talk to people and have open discussions.
Brian Ghafari-Naraghi 29:43
My neighbor next door to me, called me and they said, I have a questioned, because my dad then proceeded to tell me the story of his dad and they were deciding on whether to start dialysis or not. And it's like, okay, well, let's look at his health. And, you know, I sit down with a pad of paper, and we write pros and cons, for what symptoms, what might happen, or are, what side effects may happen. And then we just, to me, I, you weigh it out. And, you know, I have patients that have a five percent chance of survival, and they're gonna take it, and I support them and one hundred percent I had a patient that had a history of breast cancer in her family, and she had a double mastectomy. And it's like, whoa. She had to get surgery before she even had a mammogram. And, you know, it's like, okay, well, my job is to educate, to support. I, you know, I, I'm not affected by it, I can't tell you what's going to happen. And I have to explain it to you, in the easiest way possible. And I always tell people, I might, my teaching is on a fifth grade level studies have shown that it will cover ninety percent of the population. So you know, there are patients that that I say, Okay, this is how I explained it. Now, what are your questions, and some will ask me, the past the pathophysiology behind the cancer, and that's fine. But some people don't want to know, you know, it's rapid growing cells, it's cancer, you know, and that's fine. But the other thing that's sacred is being able to be there when somebody takes their last breath. It's that completion of the lifecycle. In nursing school, all the all the ladies wanted to go into the labor and delivery, the miracle of birth, that had no appeal to me, I did not want to be there. Even in nursing school, I would switch out because we could do NICU and we were doing NICU and mother baby, I would take Nick You wouldn't have to be in labor and delivery because I knew that wasn't where I wanted to be in life. But the more I look at it, it it's the it's the same sacredness of the end of the pool of the life and, you know, honoring the person, whether it's spiritual. You know, some people want you to set a fireworks, you know, pour one out. I attended a funeral of a twelve-year-old little boy, his father was in a Mexican gang. And as I was getting ready to leave the service, I get pulled back behind the church with a big group of men, that I'm like, oh, Lord, I'm going to be shot. Because they were menacing looking men, it takes a lot to unnerve me. And they're like, No. And of course, they didn't speak much English. But I had to take a shot of tequila with them. I had a patient that her wish was she she lived in a retirement community, and she didn't want the old biddies to know that she was sick. So, she laid down some ground rules. I was never supposed to be never come wearing anything that identified me as a nurse. I couldn't have my stethoscope out. I couldn't have the scrubs on. I just had to like bring bring it back. Sure. Okay. So, this is this is a woman that her husband was a lobbyist in Washington, DC. And when I asked her if she was religious, she goes, Well, I went to the National Cathedral to be seen. And so, you know, there were, there were certain things that she liked. I couldn't go over a certain time because for her, she had to get her hair and makeup on before before she was ready for me. And then it got to be I was putting doing hair and makeup. And when she passed away, she was somebody that I went after work and we had cocktail hours She's like, I, when I found out when she found out that she could drink, whatever she wants, she goes, Okay, I want to lemondrop I want to Manhattan. Then she had this list. And she one-two sips. All these drinks out. It was, it was her, her niece, and her sister-in-law and her brother. And she had no children. So, she told everybody at the facility, I was the grandson. Nobody put together that she didn't have to have a child to have a grandson. But so, she passed away. On a Saturday, I was actually out with my family. And I'm like, Okay, guys, I need to drop me off. I need to go handle this. And so, I went, went there, I snuck the funeral home people up there, we got her in and out of the building without anybody ever knowing that she had that she died, or she was sick. That was she was too proud to she didn't want to look weak.
Brian Ghafari-Naraghi 36:23
And people that are dealing with the end of life, they're not weak. There's some of the strongest people I know. You know, some, some people get angry. And I always tell them, my two things that I ask any emotion is okay, the two emotions that are not okay, is wanting to harm yourself, or wanting to harm others. And the two behaviors that are not acceptable is you spitting on me, or hitting me. And hitting, I'm pretty flexible on that, you know, if they're a little tiny person, I could probably take a blow or two, but you know, it's but giving them the chance to, you know, yell at, I tell them, you know, get out every emotion. I talked about doing a therapeutic scream, I would do it with my oncology patients. And I said, sometimes you just need to scream at the top of your lungs. Well, we had some new staff one day when I was doing the therapeutic screen, we had 10 people. But you know, it was teaching, you know, meditation and guided imagery, aromatherapy, using a nontraditional, with the traditional, I think combines beautifully. I have pre our did a service for a patient of ours, or of a patient of mine that was Scandinavian. So Nordic, the Nordic gods. And so I had to, they had a whalebone that they had, he had to keep in his hand, and I had to figure it out. So do a lot of research. You know, and the other thing too is when I'm talking with families, is I always explain I'm going to start off with saying I'm a human, and I make mistakes. So, I try to understand your culture or your religion, your belief system, but sometimes, I don't know every little detail. In the Hmong tradition, you don't say the word death, you don't say dying. Anything related to that will will cause the person spirit to follow you in the afterlife. So, I, I had read up on this before I went to approach his family and talk to him about death. And I was watching my words very closely. You know, it's like good news. And, and I would stumble a few times. But I because I've started to say something. I'm like, Oh, wait, let me let me rephrase that. And the younger generation laughed. They're like, we appreciate you trying to honor our elders. You know, but I grew up American Baptist. What Methodist Church, Buddhists now, sometimes, you know, at one point I was an atheist, you know, it's into life will make you question and everything because I had I had to start believing in what I consider Omni God, everybody prays to the same God. But we might go a different path. Because, you know, the idea that I die and I go to the pearly gates, and I've been a good actress my whole life and they say, Sorry, it was Episcopalians that were correct. You know, so I have to believe that we're all on a spiritual journey. And, you know, we we get there in our own time, and you know, who's right or who's wrong is anybody's guess. You know, that's the thing about into life, is you get to talk about anything and everything. You know, I had had a couple she was terminally ill, but wanted to have sex. And they're like, they were him. Hi. And I'm like, Are you asking about having sex? And the white blood test? Thank you. Hey, I said, if you feel like it, do it, you know, it's, it's a natural human process. You know, it's, you know, it's, I always tell patients, when we're talking about living with a terminal illness, this is the time of life that you get to eat whatever you want. It's ice cream for every meal. It's ice cream. You know, it's, I said, this is, this is your selfish time. You don't have to please anybody.
Brian Ghafari-Naraghi 42:07
And, you know, I learn so much from my patients. I did an oncology camp for kids. For several years, I was this camp nurse. And I had my three what I refer to as my three stooges. There were three girls that had the same diagnosis the same age, and they were the best friends. Well, Ally, on the night of our dance, which was the night before camp, and and her we, we figured out her cancer recurred. And at that time, I was a pain management nurse at the hospital, so, you know, we, we would go and make recommendations for people's pain. So that, you know, they would wouldn't be undertreated. And I remember getting a call at two o'clock in the morning. And Ally goes, Brian, this fool is trying to give me a milligram morphine. She goes, I think more than that, right through. So I got on the phone with the resident and did the education and he didn't, he didn't want to. He's like, Oh, no, that's too much for her. Like, it's not. And I said, you know, it's, it's at the point where now, you either write the orders, or I call the attending and the attending was the oncologist took care of my (redacted). Dr. Smith, one of the first things that I told my family when they saw Dr. Smith they said, Please don't judge her. Her hair's gonna be nappy her clothes are gonna be wrinkled. She's gonna look like she rolled out of the bed, because her philosophy is she takes time to get her hair down, put on makeup, press clothes, that's time that she's not taking care of her babies. And so, I call that runs a divert. This is just as funny issue. As he goes, I got to and everything was ordered. And, you know, Ally was somebody that I got to know personally. She had a bone marrow transplant. So I would see her in the bone marrow unit which is very, you have to sanitize and scrub down And you can't have plush toys or you know, everything has to be wiped down. So we would joke about from Steel Magnolias or favorite colors or blushing basketball. She loved pink. So, I found some pink plastic flamingos that we decorated the room with because they could be wiped down. So, but sadly she ended up she was dying from her cancer, they did everything he could. And I went over to her house to go see her one last time. And, you know, I started off with, I'm so sorry, you had this cancer, I wish you'd never would have had this cancer. It's just not right. And she looks at me and she goes, but I never would have met you. I said, there you go make me feel like an asshole. I'm tearful, and she's thankful that she got to meet me. It's like, okay. But, you know, it's, it's those things that, that make you humble. You know, it's it changed my view of how I live my life, because I do things that I want to do. If I don't enjoy it, or if I don't love it, I don't do it. because life's too short. You know, there's some nights I have ice cream for dinner. Now the kids are grown, I don't have to put a healthy meal on the table.
Brian Ghafari-Naraghi 46:56
But death takes away all pretense. Everybody's the same when they're dying. You can be rich or you could be poor. And you end up in the same place. And, you know, I've taken care of celebrities, and taking care of people that were homeless. I had a patient I used to go see you in a slide on a playground. It was one of those covered slides. And that's where he lived. Then I had patients in the penthouse in the most expensive part of town. Actually, my preferences are poor. Because they were always thankful. You know, sometimes the rich patients were a little bit entitled or, you know, it's like, I had an emergency. So I'm five minutes late. And I'm like, I called you and told you I'm gonna be late. And I'm only five minutes late. Well, you're wasting my time. And I'm like, okay, but if that was you that had the emergency. Do you want me to leave? And, you know, I tend to be blunt. I joke that I like that filter that says that you should wait, stop think, should you really say that? Now, I just found out that I go go with death. Dying. Straightforward. can be harsh terms. But then there's no confusion. I always tell people, the worst thing that you can do for a child is, especially grandpa or grandma dies. And they tell him well, grandma went to sleep. Well, that's not gonna go to sleep ever again. Because if you go to sleep, you're not gonna wake up. So, you know, if, if there were kids involved, I would get permission from the family. And I would sit down with a child and explain to him what we going to see in the ICU. What tubes. She's gonna be looked at what and, you know, I'm like, she's come, they're comfortable. But it's still scary. But they're there. They're comfortable. And I always tell them, because it's my belief that the last thing togo is hearing. I tell them to tell, you know, you got to say your last whatever. And, you know, even with patients and families it's a you gotta say I love you. I hate you. Die, you know, but say your piece because I don't believe in the word. I don't believe in closure. But I do believe in having a final conversation or a, you know, put a period on that. And, you know, it's and I'm a realist, too, when we, you know, when we talked about, everybody becomes a saint when they die. And, you know, no matter how bad a person is, they were such a wonderful person. And, and, you know, I'm like, I don't want to disparage anybody, but that's not who that person was. Let's be realistic in. My grandmother was a horrible person. She was a nasty, cranky old woman. And she, that's when she died. She died unhappy and you know, and it's like, that was her choice. And, you know, it's like, but then I have people that are very comfortable. We're okay with it. One of my ALS patients from twenty years ago. Ivan, he was a gentleman in his fifties had a child later in life. So she was the same age as my daughter at the time. So she was like twelve. And Courtney ran track. And Ivan had gotten weaker where he needed to start using a walker. And he was not going to use a walker, because that made him look weak.
Brian Ghafari-Naraghi 51:46
And I'm like, no, what makes you look weak is when you're on the floor. But, but that's okay. If you don't want to go to Courtney's track meets, that's fine. Because your pride is more important than seeing your daughter run. I'm okay, I support you. He called me a bastard. And he told me that I was fighting that I wasn't fighting fair. But he started using his walker. And he asked me to, to watch out for his daughter. So Courtney, to this day, is my daughter, I stay in touch with her, she calls me at least once a month, just checking in, you know, because that was important to him. And, you know, it's I think honoring somebody's wishes is the most honest and giving thing you can do. You know, one of my other hospice stories that I laugh about was, I was on administrative call, and we had several deaths. So I went to do a death call. For some of his family, this guy was big, he was six, seven, and about 320. And I was by myself. So, you know, part of the getting a patient ready is, I give him a bath, and I get him dressed, because that's the last time they're leaving their house. So I want to make sure that they look the best they can. And, and I'm from the old school that I talked to the dead bodies, because if I'm, if I'm doing somebody a bath, I'm gonna raise your right arm, and I'm going to use this warm cloth and wipe towards you. So whether they're alive or they're dead, I treat it the same way. Because they still are human. That, you know, it's still somebody's mother or brother, you know, there's somebody's loved one. Well, his wife kept changing her mind on what he wanted to wear, or what she wanted him to wear. So I was playing dress up with this huge man and changing him in to six outfits to getting to look just right, so so he could go to the funeral home. But she needed that, you know, I was exhausted. But, you know, it's like, I that's part of the deal for me is, it's not about me when I'm taking care of people don't matter what is going on in my life that has to stop at the door. And I'm always smiling and happy and you know, when appropriate. Because I try to I hate hospitals that are so sterile. You know, it's like, okay, can we get In color in here, let's put some music on. You know, I always asked the family what what kind of music do they listen to? And my patients did have meningitis that had that spike that temperature. We had her for probably about two months. And she was unconscious. Two months, and she woke up while I was giving her a bath. And she mouthed. Where am I and what happened? And I'm like, Are you talking to me? Yeah, it was like, it was so weird. You know, it's like, Oh, my God, she's interacting with me. And so she got better for a few days, which patients do rally, which is a gift that they can give their family, you know, you get to see him one more time, or they get, you know, mom gets to feature your favorite dish one more time. But, so this goes back to my, my theory about hearing. She looked at me and she goes, You're the nurse that sings? And I'm like, Oh, my God, I am so sorry. I'm a horrible, I can't carry a tune. But, you know, Earth Wind and Fire was her jam. So I'd be in there working and just so, you know, it taught me that. You know, it's like, but she thought it was funny, you know, at least I knew somebody was gonna have a fun having fun with me while I was there.
Brian Ghafari-Naraghi 56:41
But, you know, I get so much more than what I what I give back. Or I it's amazing. I can travel anywhere in the country, and I'll run into somebody that I've taken care of one of their family members. So weird, you know what it's like? Okay, yeah, I have lots of nursing friends that I was, you know, an official hospice nurse, because the dad or mom or dying at home and they hadn't questions and I'm like, Okay, do you need me to come over and check them out? Sure. You know, it's because I just think that's as human, that's the easiest thing I can do. It might inconvenience me. But what is it, you know, 30 minutes or an hour out of my day. That gives them a good memory. You know, luckily, my family understands. My husband was a school superintendent. So school came, you know, he had his kids calling him and I and my patients and, you know, our, our kids grew up knowing that you had to take care of you take care of your elderly, you take care of the sick. Because we're part of the big community. And if we can't take care of each other, where's our humanity going? And I think part of the COVID thing was we lost some of that humanity. No, personal touch. No, I I had a patient that told me, she goes, I just want a hug. I said, Well, I've been vaccinated. If you want to hug me, or if you want me to hug you go ahead. And early on, I was taught by a very wise nurse that you give when you're hugging a patient like that you give Disney Princess Disney Princess hugs. So like at Disney World, they do not let go first. So the patient has to be the first one to let go. So I'm hugging them until they release. And, you know, I've stood there 10 minutes on days. You know, I I work really hard at not crying in front of the family. It's hard. I will go into the bathroom or duty utility room. But, you know, to me, they don't want me to cry. I gotta be the strong one. If they're comforting me. I'm not doing my job.
Brian Ghafari-Naraghi 59:56
And you know it my mom died early, she died up to 53 of malignant hypertension. She went unhealthy to dead within 36 hours. And I come from a big family. I had a brother. So, I was 30. And I had a brother that was 12. And a brother that was 16. And so, okay, guys, Mom is dying. What do you want? Do you want we can say here at the hospital, we can take her home? What is it that you guys want? And sort of you letting the kids decide that it's their mom to you know, it's like everybody gets. I'm like, there's nobody here that gets a override anybody else's vote. Because my stepfather, he says, it's up to you. And I'm like,I understand. I'm a nurse, I'll make those decisions. And, you know, it was kind of funny, because I stayed with my mom overnight, and she had some changes. And so I asked the cardiologist, if we could do a CT of her head to see what was going on. And so he, we get the CT, he comes back and he's like, Well, she has a bleed. And I'm like, where's the bleed that you're talking about? And he goes right here, I said, No, no, that swelling. So we have a 10 minute discussion. What, why he thought it was a bleed, not swelling. I said, you know, have a neurologist or neurosurgeon come in. Somebody that's trained to read those. So I'm in my mom's room, and I could hear him talking to the new doctor. And I hear this man say, she has a son that's a nurse that thinks he knows more than a doctor. I was loaded for bear. I flung those curtains open, two steps out of the room, looked up, and the person that was standing there she goes, is that the uppity nurse? And he goes, that's her son, you know, tried to? She goes, yeah, it's swelling. I taught him how to read those. It was a doctor I had worked with, in neurology. And, you know, it's like, I knew that, you know, it killed April, to have to tell me that my mom was dead. You know, it's like, I wouldn't want it for anybody else. I want, you know, she holds a special place in my heart. But my youngest brother did not want my mom to die in the hospital. So, I asked the cardiologist if he would just take to my mom home.
Brian Ghafari-Naraghi 01:03:24
And he said, Absolutely not. She's dead. So, I said, Give me a second. I called down to the emergency room and I said, Dr. or Pam, this is Brian. My mom's currently in the ICU. I want to take her home. I'm gonna need to bag her to take her home and withdraw care at home. And I said I need to do to be her physician. Because the cardiologist won't do it because, sure, so I looked at him and told him he was fired. And then I went into what my siblings were referred to as drill sergeant mode. My mom was a red Hatter. So I sent one brother home to get her, her Red Hat. I sent my sister out to get her new purple night gown. My older brother was going to the pharmacy to get meds. I had called all the DME to get it arrived at the house Daphnie was at the house, getting it ready. had had friends my my parent, my mom and stepfather’s son was, You're in my heart by Rod Stewart.. So friends went out and found that CD for him. So to get the house ready, I told Danny I make something spaghetti because we got to feed everybody because my mom fed everybody. She was everybody's mom. And so I explained I explained to the ambulance company, what we were doing. And I said, I don't have a problem bagging her, you know, you know, I'll I'll do the bagging all the way home. And they're like, Absolutely not. But before we leave the hospital, I was the director of a hospice at the time. And I called my on-call nurse and I said, Mary, and I started rambling off of everything that I got and what I was doing, what was I missing, and she's like, slow down, Brian, what's going on? I said, my mom's dying, and I want to take her home, and I'm going to extubate her when I get home, she goes, You are most certainly not going to extubate your mom. She goes, You're the son. She goes, call me when you leave. I will be there. So I had half of my staff here. So we had a caravan of ambulances. So there's like four of them that followed with lights on to to our house, our driveway was lined with Tiki torches. There's candles lit all over the house. My moms song was playing, you could smell the spaghetti. And so why, I let my friends prepare my mom, get her settled in. I'm in there feeding the, the ambulance, the EMTs and paramedics. Because my mom would want that. Because that's rude. You know, you don't you don't have people over to your house without feeding them.
Brian Ghafari-Naraghi 01:06:47
And, you know, these paramedics will just like shocked that I had to make sure they ate it and like, it's like, it's part of the deal. That's who this woman is. That's how, how we honor her. And, you know, so we ended up taking her to my house because my brother didn't want her to die in his house, which is fine. You know, 12 years old, I understand. So I have this big picture window. And we sat, we set the bed in front of it. We all sat on the bed with her. She had six kids and her husband, so and my cat. And we just sat there while she passed. And we told stories. My mom would always tell everybody that she never did much in her life. And she wanted to be a mom. And she was the best mom ever. She worked probably in her entire life a year as a housekeeper. Because I worked at the hotels as front desk, and she could come with me and she can make some extra money. So, you know, and she's like, I didn't make you know, she'd always say I don't make a big difference in the world. So when we had her funeral, my mom hated the fact that my sister and I wore black all the time. So I told everybody that was invited to the funeral is you were the brightest color you have. If anybody wears black, I'm kicking you out. And people, we had people at the altar that we brought things that reminded us of our mom. I brought a bottle of windex because she was always wiping down the glass window, the front door. You know, I my older brother brought pot, furniture polish because she would she polished she would come over to my house one day a week in his house and clean our house.
Brian Ghafari-Naraghi 01:09:27
Well, she had waxed his tables, and he was climbing up on the table to get to change a light bulb and slid off the table. We had the minister; he had his black robe on with the with the purple boa that was hers that she wore with a red hat. And, you know, we had Aerosmith playing at the church. So, you know, Lovin in an Elevator because my mom was a big Aerosmith fan. We had a a traditional non-traditional funeral, that was at a church. I was actually finishing my Masters. And the night before she, so they would come over on a Friday night. Because I had...there was my son. And a year behind him was my, my brother, the year behind him was my sister, or my daughter. And then I had a brother that was three years younger than that. And so, you know, they were raised together as brothers, you know, and I had a pool and so you know, my, my family would come over, we would spend Friday night hanging out. I had just I was doing like children and grief class was what I was doing. And I had to find a book to present to the class. And I found this wonderful book called The Next Place. And I by Warren Hansen and it's it's a beautiful book that explains death in such a gentle way. It talks about I won't be short or tall. I won't be fat or skinny. I'll be perfect. I'll be me, humbly in the ever darkness. I will not be alone because I take the memories of my loved ones. So that the Friday before she she had had the malignant hypertension. We read the book back in my office and where I'm at now and she goes, I need to borrow that book because I want to take it to the old ladies to Red Hat. You know, she called her red hatters the old ladies. And so, my husband read that book at her funeral. We had a couple of songs. And then we did a poem. We're not meant to go to cradle to grave in a perfect perfect wrap box. Were supposed to we should be sliding in sideways, totally worn out. Totally used up. Exclaiming Wow, what a ride. And that's how my mom lived her life. She she was a life of the party. It it's just sad that she didn't get to see her grandkids and great grandkids. But I know she's with us. I have a niece that I swear to God as my mom that came back. She's called me a nickname that my mom only called me. And she died. My mom died 12 years before but before she was born, she was like she my mom would call me Bri-Guy. And I'm like, so we were at the park one day and she called me. Where did you hear that? I don’t know, that's your name is. But she looks like my mom. She acts like my mom. It's just kind of weird. But you know but it gave me a whole different understanding of death. You know, I told people I had attended many deaths.
Brian Ghafari-Naraghi 01:13:54
But my mom has changed me. I I was a mama's boy. My mom and I did all sorts of things. On my birthday. The annual tradition was I would take her out for the day. We would go shopping for her we would get her a nice outfit. We'd have a nice lunch and just spend the day together. Wasting the time. You know who would go to a museum Um, we could be a thrift store, you know, it was just spending time together. So, you know, she was a significant part of my life. And so, when I, we had her curt...cremated and I asked my siblings, I said would you like a necklace with some of her ashes in it and they all thought that was the best idea in the world. Well, so when we had her cremated, she collected amber glass. So instead of using a regular urn, my, my mom's goal in life was to be a drag queen. Because she said that they had the best clothes, the best hair and the best makeup and jewelry. Because she was a stay-at-home mom. I don't get to dress up like that often so. And she chunky. So, she always says she was stuck with fluff. So, in, in the glass urn we wrapped in some gold LeMay. So I had to pop open the the urn to break it out to get the ashes in it. And my sister and my husband, we're in the living room, and I'm in the kitchen. And all of a sudden, I start laughing hysterically. Because I open it up. And I start pulling out stuffing, like pillow stuffing. And I'm like, oh my god, she was stuffed with love.
Brian Ghafari-Naraghi 01:16:18
And it was, you know, that just gave me the moment that I knew that. I did the right thing. You know. And I she had she had an anaphylactic reaction to IV contrast. And I was holding her right before they put her put a breathing tube down and she goes, Don't let me die. And I said I won't. And you know, I didn't have anything, any control over that. I know I shouldn't promise that. But that's what she needed to hear. And, you know, I had a little problem with that. There, there was a little survivor's guilt after that, but I knew I did want honored her. And, you know, I made sure that everybody was okay. I ended up stepping back from being a hospice director. Because I was working 70 to 80 hours a week, because I had two younger brothers. And my mom always referred to her having seven children. And one of them being my stepfather. And I we didn't really grasp the knowledge until after she passed away. The Sunday after she passed away, he went to my sister and said, What do I wear to church, because my mom would set his church clothes out for him. And mom was the more the disciplinarian. He wanted to be their friend. So, I needed to be out of all my siblings, there, there was four of us. One was just a young adult. One was in her mid-20s. I was in my 30s and my brother was two years older than me. So, we had to take over those responsibilities. And my brother was an auto body painter. My sister was an accountant. Another brother was a locksmith, but I was a nurse. So, I took a night. I was a night administrator at a university hospital work three days a week, so I could be off during the week to go check in on my brother because, you know, he, he was a little shit.
Brian Ghafari-Naraghi 01:18:47
I went to school to see how he was doing. I said, so, how's his grades? And they're like, well, we're not pushing him. He's having a hard time. I'm like hard time about what? Your mom dying. I said you need to get him down here now. And so, my brother comes walking in, he looks at me. He goes, What's the matter? I said, if you've been lying, he goes, they asked me if I'm sad, and I say yes. And then I don't have to do any schoolwork. And I'm like, Brandon, what would mom do if you if she was here? Kick my butt. So, what do you need to do? Do my schoolwork. And, you know, it's like, the school counselor thought I was just the meanest person in the world. And I'm like, No. I know my brother, he...he is a body man. But there was a time in his life that I was wasn't sure he was going to be a hitman for the mob, or the President of the United States, it could have went either way. Because he was, he knew how to work things. He was the baby of the family. But then I had another brother that was skipping class. And so, I had worked it out that when our, when I couldn't, I told him, I said, if you aren't showing up to school, I'm gonna start showing up to school and dragging you there. Because that was my mom's number one rule, you had to graduate high school. Didn't have to go to college. But you didn't have to have your high school diploma, GED didn't count. And I said, I, I will black out my teeth, wear junky clothes, and follow you around to every one of your classes. And I said, when I went, I'm not able to do that. Judy, who was my dad's cousin, was also my mom's best friend. And she was a retired schoolteacher. And she goes, Oh, my God, this would be so much fun. So, he had the threat of two people coming up dresses, you know, embarrassing. He graduated high school so. You know, it's like, we had had things that we had to do. And you know, it was great. It turned out good. You know, we the three older kids became the parents, as we are still to this day.
Brian Ghafari-Naraghi 01:21:35
And, you know, my youngest brother went and lived with my oldest brother, because his son was not that much younger or younger than my brother. So, you know, it's like, okay, they were going to the same school. So it worked out really well. My other brothers stayed with, with our dad, we didn't get him through school, but we probably should have moved him into one of our other house, my sister's house or my house, because my dad just didn't make him do things. And, you know, it's like, death is sad. And I remember telling my family that they said, death is sad, but life goes on. And our mom would want us to go on, she'd want us to do stuff with our lives. And when she said do stuff, it didn't have to be, you know, professional, you know, you didn't have to be have a college degree you didn't, you know, as long as you did something that you loved, and it helped others or contributed to society. That's all she wanted. And we all do that now. You know, and it, I went from working 70-80 hours a week and having a part time job to work. It's not about work. You know, as much as I love my jobs. If I die tomorrow, they'll hire somebody to put my place. And it'll keep going on. So, I look at life now that if I die tomorrow, would I be happy with what I'm doing?
Brian Ghafari-Naraghi 01:23:28
And, you know, it changed the way I look at life. And I live free. You know, it's the choices I get to make. You know, it's like, Does this bring me joy? If it doesn't bring me joy, why am I doing it? And that's what I bring to my patients. You know, I help do lifetime legacies. So that could be a scrapbook with a patient for their family. Ivan wrote Ivan got cards for Courtney's 16th birthday, high school graduation, college graduation, masters, when she gets married and when she has a baby and he got cars and gifts. For each one of those milestones, granted, she said that she'll probably never get the child and the marriage gift, but you know, that's okay. But he, he's been part of every milestone in her life. I worked with a friend and we videotape somebody telling their life story. And, you know, these are such things that I missed out on, because I didn't have enough time with my mom. You know, I tell families like when you're having the service for them, but in the back of wherever you're at, or table up, put a picture up and put a sign that says, Please write your favorite story of our mom or our son are... Because the one thing I noticed, I discovered was from my mom's funeral, people told me hundreds of stories that day. I can't remember half of them. And so I suggested that to a family, and they did that. And the wife called me back about six months later and goes, Oh, my God, these are so comforting. So, you know, it's it's the stories that people don't always know. You know, it's you know. I did stupid things. When I was a kid. I car surf, I would get on an I-70 and I had a Celica Supra was a moonroof. So, it opened up, I would plan out the moonroof, and stand on top of the roof, going ninety miles. It's a miracle that I'm alive. Why I thought that was fun. I don't know. I was younger and dumb. You know, I get some of the best stories from people about their life, you know, I, I go in. And any job I've ever had, I've told my boss, I'm going to take the time with patients.
Brian Ghafari-Naraghi 01:26:47
Whether that be thirty minutes or an hour, they get my attention. I sit down. And we talk. Because most people are scared, you know? Or they've never been in the hospital before or, you know, they just got a new diagnosis and they don't know what, what to do with it. What does it mean? And, you know, there's a movie called Wit. It was actually a one-person play. And it's about a college professor who was a English literature specialist. And she's diagnosed with terminal breast cancer. And in one of the scenes, she's getting informed consent about the chemotherapy treatment. And this doctor is talking way over her head. And, you know, she has her side dia..dialogue. It's like, I'm talking Chaucer to this man. And, you know, so I teach ELNEC, which is end of life nursing core curriculum. And I love to show videos, or you know, snippets of movies that talk about dying in a good way or a bad way. Have you ever seen the, show Little Miss Sunshine. It's a very funny show. But it's about this little girl going to a little pageant, Little Miss Sunshine pageant. So, they're taking a family trip from my, Arizona to California. Well, on the way there, grandpa dies. So, the hospital social worker comes up and says I'm sorry for your loss. Here's this paperwork that needs to be done. And, you know, it's everything that you wouldn't want to do. Because, you know, it's like, it gives people a good idea of what not to say, you know, or I tell people I always start off with I'm human, I'm gonna screw up. So, if I offend you know, it's that was not my purpose. Everybody's family communicates a little differently. And I say that I know I'm very straightforward. And I use harsh word. But I don't want there to be any confusion. You know? Like when somebody says, oh so and so moved on, where they moved to didn't move across the street, did they die? Did they move across country? You know, I don't like ambiguity. And because death is such a hard topic to talk about, I don't want it to be ambiguous. And sometimes, you know, family members, and I will tell them, I'm going to use harsh terms. And if you don't want to hear them, this might be the time you step out. Because I want or when I'm having a family meeting, I want everybody to be there. Not that I want to be the center of attention because, Lord, I hate being the center of attention. I'm a wallflower. You know, they always say there's a gardener. And there's, there's the flower. I'm definitely a gardener. But I know that I can do I do this very well. And if somebody ever told me that I would, would be working with the dying would have called you a liar. You know, as a new grad, I was ICU, ER, feed them and street them, you know, as soon as they were excavated and sent into the floor, you know, as little as little interaction I could have was best. And then I got to see, I got put in my place.
Brian Ghafari-Naraghi 01:31:21
I got pru, pro, shown that this is what I was meant to do. Because it didn't bother me. You know, it's, I love doing the education. You know, I like taking the scariness out of it. You know, I want people to know what's coming. One of the things that people always worry about is that the death rattle. So, it's that that gurgling sound, right before somebody's getting ready to pass. Well, all that is, is you and I can clean our throat. So, what happens is, they're unable to clear their throat isn't painful to them, it doesn't cause them any distress. It just causes a weird, a bad sound. And so many people find comfort in that, you know, and it's like, Oh, yeah. So let me tell you how the pathophysiology of it. So let me tell you how this functions why this happened. You know, didn't we talk about the rally, you know, I always say, Don't be surprised if they, wake up one day, and there are old self and I said, that's a blessing. So those are the times you get to spend with the loved one. You know, and I've seen it happen with Alzheimer's patients. And I've seen it happen with all kinds of patients that the families get these sacred moments of, you know, I had a patient that wanted ham and beans. So, she called her the doctor called her best friend and said I need some ham and beans. So, her best friend whipped up some and ran up the hospital. And her daughter got to give her a bowl of ham and bean. Then I reflect on I had a 23-year-old that was dying in the hospital. And he wanted an orange crush soda. And the doctor said, no, he can't have it, too much sodium. And I was a night nurse, and I’m like bring him the orange crush soda. I’ll have to give him a little more fluids to offset the sodium. But you know, I have those orders but I could do that. Well, while mom was getting left to get the orange soda, a nurse brought him the nurse, orange soda. I was livid with that nurse. I'm like you took away that one thing that mom could do. So, we're all going to lie and this is your first drink of orange crush soda with your mom give it because, you know, my job is not to be a hero, it's not to be the savior, not, I am the calm in the storm. I'm the one that, it's gonna be okay. It might not be fun for a while. But everything's gonna work out. And we're gonna make sure we take the best care of them. And, you know, I tell people, I treat everybody like I would my mother. They get the same exact treatment that I would my mother. When my mother-in-law passed away. She was an old retired nurse, and she's going in for a valve replacement. Unfortunately, her heart was too weak to sew the valve in place. So, they told us that. You know, they gave us our options. And her husband looks at me and says, Brian, what are we deciding? And I'm like, Well, remember what Millie said she didn't want to stay on ventilators. And, you know, she, if it's her time, she wants to go peacefully. I was given strict instructions that if she woke up with beta dine on her skin, my ass is grass, because it was itchy. And I was a nurse and I've seen boobs before.
Brian Ghafari-Naraghi 01:36:06
You know, and this is a woman that when I first she hated me when I first met Danny, because she thought I made him gay. And we grew to appreciate each other over the years. Like, when my son had cancer, I was working six 12s to pay for his medicine, and she goes, I give you the money. I said, I do not take money from the devil. Because she had given Danny the down payment on the house that he had bought, or was living in. When we met when we bought our new house. We were gonna give her money back. Well, you know, it takes a little bit to get your money back. And she just kept after I want that five thousand dollars, and I'm like, so when she offered money, I'm like, Ah, you are the devil when it comes to money. And I don't want to owe you anything. This is my son. I will die before I take money. And you know, and I had instructions with her that I was not to let Danny and Carol fight her, her kids. Because they would I was not supposed to let her sisters act a fool because they would and they did. So, my job was to orchestrate her, the passing. And I I remember sitting in the room with Danny and Carol. And they got into a fight over should they let her sisters come back. And I I stopped, turned around and I said out and then he goes you heard him. He said you have to leave. That was for you too. Because your mom did not want this. I said go out, get get a drink. Take a deep breath. Get yourself together and then come back in as an adult. Because this is not what she'd want. And here's like oh my god. You know, it's like she my sister-in-law turns around and says is he serious? He goes dead serious. He goes he's not letting, he goes mom told us we couldn’t act a fool and we're fighting. So, you know, it's I've played referee with families before you know because death brings out all the dysfunction in the families. There's so much you know, I say there we call it there's fun in dysfunctional for a reason. Because it's entertaining. It can be a pain but it can be really entertaining. You know?
Brian Ghafari-Naraghi 01:39:16
Its, I was a bouncer at a friend of mines mom's funeral she her mom had mental illness, was crossing a Main Street at dusk, just as it was getting darker. She was hit and killed by a car. And so, I'm at the funeral. And I'm the only white guy, my friend is African American. And I'm standing next to the coffin with her mom, who, so, it was her grandma, my friend's grandma. And she started talking bad about her daughter. Because mental illness was not an excuse. She was a drunk. It's like, well, she was not self-medicating with alcohol because she had these problems. And so we're sitting in a casket, and she's just talking horribly about her daughter. And I said, I'm gonna stop you right there. She had her flaws. But this is not the time or place. So, if you can't hold your tongue, I'm gonna need you to leave. And she was sitting there, and who are you? I said, the guy telling you that you're going to be leaving if you keep causing a scene. And I just, my friends like, see he’s a bouncer, you know, but it was like, they needed that, you know, it's like, nobody was going to take control. And, you know, of course, she was never going to speak back to her grandmother.
Brian Ghafari-Naraghi 01:41:07
And it's like, it's like, when we got there, Jay and I got went there, we looked at looked at her mom, and in the cast for skirt was off, you know, it was turned to one side, so you can see the seam of her thigh. So, I'm like, and that was a problem for Jay. Jay is one of the people that when you dress you dress perfect, your shoes are white, you know, there's not a spot. I’m like ok, watch me, have my back. I adjust her skirt getting it turned right in the casket, because that was important to her, you know, its, I, I've started, I'm a collection of hands. I take it with permission of families with their loved ones hands. And I can send you some of the pictures that I just love because it's one of the last things they could do. I bought a stethoscope that I can record a heart sound on. And then I can transfer it over to a file. And I can put them in build their heart, or just send them a file on their phone or on the computer. You know, because it's, it's something that is comforting. I had a guy that was 16 years old, or the one that died on Valentine's Day. And I I'm still friends with his his parents. But he goes Brian, that heart got her through the worst time in her life. He goes, she would lay in bed and play his heartbeat. And I'm like, every every mother knows the sound of their child heartbeat. I said you could tell. They know, their child heartbeat. And like it's funny, I don't have any blood with my son. But I know his I know the sound of it. I know, you know is like I know when he's not breathing correctly. You know, it's like, these are things as a parent I know. And I can only imagine the bond between a mother and child when that mother carried him inside for nine months. You know, they felt the baby move. They felt the heartbeat, but you know, so giving them something that they could have as a memory or doing a hand in hand. A moment printed a hand or clipping of the hair. You know things that make it easier for them to get through the day.
Brian Ghafari-Naraghi 01:44:11
I had a young man that was killed on a motorcycle hit by a car. His mom was a nurse that worked at a hospital with in the metro area, and somehow I became their surrogate support person. So, I had to go to a funeral home when they were planning his funeral that I had, you know, and somebody's like, that's overstepping your bounds. And I'm like, no, because I'm there to provide support. I'm like, I taught a class before with ALS patients, help, I'm dying. I've never done this before. And why I did that class, I had a friend do one with the caregivers. And then we switch. And you know, it. It was just so neat for them. to be able to talk about it. You know, the funniest thing is, I was a palliative care nurse in the hospital, you know, I go talk to family about end of life. And I would meet the family in the hallway. And they would tell me, Mom doesn't know she's dying. Please don't use the word dying. Don't talk about dying don't. So, what I said, I won't use those words. But if she asked, I will not lie. Because, you know, I always talk about goals of care. And anytime you go to the doctor, you should have a goal of care. What, Why are you there? Because if you don't have a goal, why do you need to go to the doctor. But then I go in and talk with the patient. And the patient tells me, I know I'm dying. But don't tell my children, they can't handle it. And then I'm like, you know, you're both telling me this, right? I’m like it's, it's not that scary. It's part of life. I said, you know, if we could keep our mothers another 100 years, it still wouldn't be long enough. But we cherish the moments we have with them. And they live on in US. I have my mom's death stare according to my my siblings. My mom had this look that when you messed up, you knew you messed up. And I guess I have that look. Because it even says my older brother. But you know, it's it's that sacred family time and giving them permission to do things. Play music. I had another patient that, Martin was a character to say the least. Martin was gay. He had HIV. But then he also had lung cancer. And he had a twin sister. So, Martin was always causing havoc, just because he could. So, he had to have move out of his apartment. So, we got we had some hospice volunteers that we're gonna go over and help him pack. And these were young college girls that were going over to pack and I'm like, Martin, don't let them start packing in your bedroom until I get there. And of course, I had a patient get sick, so I had to stop off before going there. And I call Martin. I'm like, okay, Martin. Remember, don't let those girls in your bedroom. So, I get there and they're like, what's the rubber fist use for? He had a drawer of sex toys. I had to explain to them, I don't know if the girls were fascinated or horrified.
Brian Ghafari-Naraghi 01:48:54
But he just thought it was the funniest thing in the world. And his sister goes, of course he did. And then I get a call from his mom one time that he's running down one of the main streets naked as a jaybird. And she goes, I don't know what to do. I'm like, Okay, I'll be there. So I don't have, I have a black trash bag is all I have with me at the time. So, I go stop on the side of the road, put the trash bag on him, put him in my car and drive me back home. And, you know, then then he went to a facility. And he called me upset, because they were having a Cinco de Mayo party. And nobody was doing a margarita. It wasn't the fifth of May. It was July. So I went there and met his sister there. And he's like, they took all the decorations. They knew you guys were coming. But when I talked to Martin about, is there something you would like to do, like, you know, something you want to leave your family, he wanted to do make a set of wind chimes. Like, okay, I can do that. So, my husband was the vice principal of a school. So we got some copper pipe, and they cut it for me in links, put holes in it so that we can string it, we got beads, and they had the top made for it. So he got to make these wind chimes. And the day that Martin was dying, I was there with a family. And at first, we were all in the room. And he was just hanging on. And the wind chimes were in the dining room and I go, Margaret Ann, his twin, I said why don't you go in and lay with him. He came into this world with you. Maybe that's what he needs. After about 10 minutes inside, there's no wind, you know, there's no fans, the wind chimes, chime, and Margaret Ann comes out and says that he's gone. And that's what he needed. He needed it to be with his sister. And to this day Margaret Ann goes, You gave me such a wonderful gift. She goes, I've never thought about I came in, we came in the world together. She goes, I know he'll be there with when it's my turn, but I got to be there with him. She goes, he's in my arms. And you know, it's like, I get to make those moments happen. You know, and I tell everybody, you know, families always, like, want to take a picture of the nurse. And I'm like, you know, I prefer not to have a picture taken. Because I want to be that warm feeling. I don't want to be the person, I don't want to be the person because that's not my job. I'm not a character in this play. I'm the stage manager making sure that everything goes off correctly. And, you know, most people, accept that, I've had a few families that insisted I will do it. But you know, but, you know, it's truly not about me. And that's what I I always tell everybody. I I've helped several of our friends say goodbye to their parents. And I think, you know, it's such an honor. I get to make things better. I I can help. I can find ways of making a bad situation a little bit better. You know, there's always a rainbow after a storm. So, I would you just have to look sometimes a little harder, or there's a silver lining through stuff. You know, sometimes we have to read, refocus what we're talking about, you know, I hate when people say they lost the battle with cancer. Because sometimes it's a fight, you're not going to win. That's a battle that is impossible. The patient had cancer and they died of cancer. Because if a person really has the ability to fight that cancer, they would be alive. But some things are out of our control. And, you know, we just get to be there and support them and tell stories, you know, I get to hear stories I, you know, I always ask what's the funniest story, you know, most embarrassing story, funniest story. How'd you meet? You know, because somebody's always got a story, you know, every family has that one person in their family that does something or, you know, I have a whole family full of people that that I like to let them tell those stories. And it shows it shows them that they're valued. Because no one ever dies alone. I will set vigil with a patient before I let him die alone.
Brian Ghafari-Naraghi 01:55:12
Sometimes patients want to die alone. And I tell families don't you know, it is truly up to the patient. Because I had this one family that they have around the clock family with, with this guy. And two o'clock in the morning, his sister went to the bathroom. I said he doesnt want you to see him die. He was probably probably I said he probably probably said, Thank God, you guys are gone. Now I can make my exit. And she goes, That sounds like my brother. You know, it's being able to explain those things. You know, because I don't want there's no guilt. Nobody should feel guilty. Unless they did something really bad. Because a patient's gonna die. When it's when they're ready. I had a patient on hospice, that for all practical purposes, he had went two months without food or water. He was skin and bones. And, you know, we, we talked to the family about give him permission and, and oh, yeah, we’ve given him permission. Well, turns out the wife goes, anytime they were by themselves, because her son heard this, I can't live without you don't leave me. And we finally worked with her that she's gonna be okay. And we made sure you know, the son had a plan that mom was gonna move in, or he was gonna move to mom's house. And live with her because he was a single man. That way, she had her regular space and could function. And as soon as she gave him permission, he passed. You know, and, it's amazing to me. People see, see things that I believe they do. You know, people talk about seeing their loved one before they die, and, you know, I think heaven is a moment in time when we're more when we are at our happiest. If you ever have a chance to read the book, the five people you meet in heaven. It's one of the best books. There is, Tuesday with Maurey is Mitch Album is the writer. And everybody meets five people before they go to heaven. And you might not know, you might be one of those five people. But you might not have ever met that person. Yet, you might not have had, you know, like these kids are rolling tires down a hill. And it caused a car wreck. And they died. Well, that kid was tied to that death. But he didn't know that person. And you know, but it's just a really I find that comforting that have, you know, the pearly gates and all that. I don't know if I buy that. So I think heaven is when we're at a moment in time that we're the happiest you know, my mom and her best friend are in heaven, probably thrift shopping right now. These are these two women were nothing but trouble together. Judy lost her eyesight. My mom didn't drive because it scared to death Jeannie drove well they decided that when Judy lost her eyesight they could drive mom could me the eyes Judy can steer. I'm like, No. And, you know, it's like I don't I, I always do something in honor of somebody that passes, you know, I random act of kindness I Okay, a flowers to hand somebody looks like they're having a rough day or, you know, picking up the tab for, I was at the gas station, there was a police officer that came in to get a snack. I’ll pay it, Hes like you don’t have to do that. I said I know, but I had a friend that passed and I'm doing this in her honor, because sending flowers to a funeral, really, the family's not going to enjoy it because the funeral flowers. You know, it's like, I remember looking at them going, okay, I really don't want any of these flowers because there are funeral bouquets.
Brian Ghafari-Naraghi 02:00:50
You know, when I was with one hospice, we had a volunteer that with funeral flowers or wedding flowers, they could donate them. And this florist would arrange flowers for pay, our patients all had fresh flowers in the room. So, you know, what a great use of upcycling something that would have just ended up in the trash. You know, this woman that got married, just loved the idea. And she asked if she could deliver the flowers. She goes, I want to wear my wedding dresses and drop, because I know it sounds silly, but like, you know, everybody loved it. You know, it's like, who doesn't like a woman in her wedding dress? Because there's singing and they are happy, you know, it's it's a happy moment. And, you know, I've been with friends, I've been with enemies. And it means I, you know, taking care of people that repulsed me. But they get the same care. I don't. We had a guy that killed a little girl abducted her raped her killed her. And he was my patient. And people were going, I don't understand how you can take care of him. At the end of the day, he's a patient, he needs care. My job is not to judge. You know, my job is to provide care. Because, first of all, I don't want the responsibility of judging anybody. Yeah, what he did was repulsive. But I'm better than him. Because I'm going to treat him with dignity. Because that was the way I was raised. I don't know if this is anything that you're needing or wanting. I'm just rambling. So, if you want or need to redirect me, please do. Because I can talk about this for hours. I get, I love when I get to go to nursing schools, and do have in the life lecture. My nephew just graduated nursing school I gave the end of life lecture in the last semester for his class. But it's fun, because I love being able to educate people and being able to teach people about it not being scary, or how we can make it what can we do to make it not scary? What can we do to make things better? And, you know, I, it's, I'm blessed. You know, I always tell patients, it's an honor, a privilege, I get to care for them. I see it as a sacred time. And to be asked to be in an intimate moment of people you don't know. It's such an honor. And I don't want to do anything that would ruin that. You know, I have to admit, sometimes it doesn't turn out good. I've been called a murderer before, you know. But I know it's not me. I know it's grief. And that that goes back to don't spit on me and or hit me. We're good. You can call me any name you want. I'm cool with that because I understand you're losing control.
Brian Ghafari-Naraghi 02:04:58
You know sometimes you have to care for the spouse dying, or of the dying, too. I had a lady that I had to teach how to balance a checkbook. Because her husband did the bills all their lives. She had never written a check. So I started teaching her and, we got a volunteer to, there was an accountant that was showing her how to do do that. And that, to me, the family is the unit of care. And family is who's the patient says, his family. We're born with family, and we collect family along the way. And sometimes the family we collect are more important than the ones that are related to us by blood. And, you know, because I want people to be surrounded by love, at the end of the day. They were loved. No matter. My grandmother was a nightmare of a person. I loved her, despite everything she did. But, you know, it's like, I moved her into my house and cared for her for two months, or no, no, not two months, eight months. And by the second day, I was calling my best friend because nurse going, why can't I do this? This is what I was trained to do. I'm a nurse. And she goes, Brian. When you nurse, you get to go home at the end of the day. Because you get to go home, home is work. And it made me prioritize. Making time for myself. self care is not a bad thing. You know, and teaching families that it's okay, I need you to go home and take a shower. I want you to go get them to the you know, just get out of this hospital just for a few moments. I promise you that they won't be left alone. And my poor husband has been left at a bedside before when I couldn't find anybody else. Because he knows how passionate I am about and, you know, he volunteered with many a hospice patients. Arthur was my god Arthur was just a little he was an Irish guy. He looks like a little leprechaun. But he had heart disease. And he was on diuretic so he was peeing all the time. And he told me that our he told me that he was going to die pissing himself to death. He died on the commode. You know, it's like, we all had to chuckle about it. Because that's what he said.You know, and then I learned learn from a wise Chaplain when I first started in hospice, that sometimes what we do to care for a patient has nothing to do with the patient. Because I was going out to ride along with him, he's like, you might want to wear some jeans and shirts and bring some gloves. Like, why? Because you'll see when we get there. This man had a beautiful lawn, manicure, soft graph, but he had a walnut tree in his yard. And as walnut trees break down, they release an acid and burn the grass. So his spiritual distress was related to watching his lawn go bad. So the correct treatment for him was we went out and picked up walnuts. And, you know, it's like How simple is that? You know? Yeah, I'm just lucky. I it's and I find it funny because it parties, people will walk, you know, what, what do you do? I work with people that are dying. And they start walking, taking steps back like, you know, it's not contagious. But, you know, it's like, like, it's just so funny that, you know, people are so scared, and we're all gonna go through it. So It's the unknown. You know, once you make peace with the unknown, it's all good. You know, I remember being in a rough area that had a guy pulling down on me. And I looked at him and I said, do what you got to do. Good work God. I'm at peace. So if you can shoot me shoot me, because that's how, that's my end. But if you're not get the hell out of here. And he ran away, calling me a crazy white man. But you know, it's like, okay, you can't, the worst you could do is kill me. And I'm okay with that. Or with, you know, the, the, the Spirit the big guy or big girl in sky. I, I think of him as the genie from Aladdin. Because that makes makes me happy. And well, I'll tell you the one one more story than that I pulled off that I have no idea how I did this. So I had, it was a little Hispanic boy, the father was in the gang. So I had him at camp. So they were from East LA. They had just moved to the Midwest. And they went to camp for a week. So there's woods, there's a lake there, you know, we taught them how to fish. A friend of mine, Joyce has been taking her fishing club up there for twenty years, teaching kids to fish. And she used to say that I would she goes, we know not to let them hook or put the bait on the hook. Because you know what l wants to get stuck. And she goes, and Lord knows Brian will come down here and let us know. But Enrique ended up getting a bone marrow transplant. And I would go in and see him I was the night supervisor at the time. I found these handheld games that were like a fishing reel. So youd cast. And so him and I would fish in the room. And he goes, Brian, what do you think heavens like? And I don't know where I came up with this. But I was like, you know, when you first came to Camp, how you were nervous and scared. Didn't know what it was gonna be like, by the end of the week, you didn't want to leave. I think that's what happens like. And he he found comfort in that. And I have no idea where I pulled that out of. But, you know, I'm like, that was like, the nurse who was on the unit. She goes, That was a good analogy. How long did you practice it? I said, I just popped into my head. You know, it's like, I think we're just given. We make mistakes, you know, and that's, it's all about life. And living the life we have, and being appreciative of what we have and who's in our lives. You know, whether their four legged friends or two legged friends are, you know, we're, we're blessed. And I think being able to share these stories with you. I I know this is the first time we met, but I feel close to you because, you know, some of the most topics about my life. But I'm not afraid to talk, you know, and I there is a balance between when I'm working with a family and giving them enough to know that I understand but not giving them so much. It puts more stress on them. But you know, the power of presence is an amazing gift. I tell people you know sometimes you don't have to say anything. Just being there holding their hand or just you know Doing something. I remember one of the things that I started when I first started joining the hospices of clinical director, I went out and bought polish, nail polish and fingernail polish remover. And every one of my staff had polish a kit, kit with them. And didn't matter what your discipline was, would you like to nails polished if it was a female? People loved that. And I would have said that I, I started getting smelly lotion, you know, lavender lotions, and because we all want to feel good. And if we can give them that little bit of, you know, special moments.
Brian Ghafari-Naraghi 02:15:52
Right now, I'm watching a dear friend, I convinced, she was actually a recruiter, when I met her. She was recruited office staff when I was a clinical director. And I convinced her to come work for the hospice. And then, so I had a lady that was my volunteer coordinator, that part of orientation, everybody had to go out with every discipline. So, nurses went out with the social workers, the chaplains, bath aide, everybody in administration, because I wanted everybody to know what each one of us did. And so, I hired a volunteer coordinator. She comes in on the second day, being on the job and she goes, Brian, I can't do it. She goes, this is just too hard. And I, I had been to New Orleans. Prior to this, and I had this sign in my office, it says, Why don't you pull up your big girl panties and get over it? And Cindy goes, I can't, can't get over it. I’m like, okay. I appreciate your time. You know, thank you for bringing one experience to have and your gifts. This is not the right place for you. I want you to be in the right place. So, Veronica, who was my staffing coordinator, and like I said, you'd be really good as a volunteer coordinator. And she goes, I don't know the first thing about I said, well, let me see if I can do something. So, I called Cindy. And I said, I have a favor to ask. Would you be willing to kind of mentor Veronica was taking over the volunteer program? And, she was sure. After two weeks of mentoring Veronica, she asked me to come back. Because she saw her place in there, and it was it. It was her home. You know, my staff was I told people at my you know, we're a family. We're going to fight. It's going to be ugly at times. But at the end of the day, we love each other. And no matter what, some some day, somebody's gonna walk in and they had a bad day, and they're just gonna lay into you. And you give them grace. Because you're gonna be there someday. And Veronica, her mom had early onset Alzheimer's. And Veronica, remember, she goes, I just remembered her teaching her mom like music and dancing. So, she goes every Friday, and they play music and dance at the nursing home. And, you know, it's like, Veronica, she goes, Brian, I started doing it for her, but oh my god, I get so close. I get she goes, I get a connection that I wouldn't otherwise have. You know, and I'm like, nobody wants you to just stand there and stare at them. So, you know, play music, read a book, you know, but just be present. And, you know, when I’m with a patient, so the only thing that matters in the world I had a habit of looking at my watch. Not that I was looking. I was just curious what time it was. Not that I was in a hurry to go anywhere. But a family thought I was in a hurry. So, I started stopped wearing a watch. Because I didn't want them to ever think that I had somewhere else better to be and you know, there are a few times that, in life that, like when my son got married, my daughter got married. And when my daughter had her baby, well, my daughter had her baby during COVID. So, not very well, we could go up, but, you know, I, I know not to waste my sacred moments. But then again, if I can be there for something sacred moment, I'm gonna be there. And I'm lucky that my husband, and my children understand, and they give me the grace to do when to do this.
Brian Ghafari-Naraghi 02:21:28
You know, if I can make a situation a tiny bit better, if I could be that spark, or that sparkle in that dull day. You know, by giving them something to do like paint nails, I mean, I can empower people to give some, some comfort or some bonding, you know, playing card games, or I hate I hate playing board games, but I will sit down and play a board game. If that's what the patient wants, because, again, I'm there for them, and to take care of them and to help people. And that's what I found myself doing a lot. During COVID is, you know, I did all my research, I read everything the CDC, NIH, published, so that I could answer a question, you know, because I'm really scared. And I, let me just talk to you about it. You know, not too long ago, my my friend who's my eye doctor, she called me and she has a rheumatoid arthritis. And so, she's on an immunosuppressant. Her neighbor came over to let him let her know that his wife died of COVID. And it's like, okay, [inaudible] call your doctors see if you need to go on preventative, I said, Because I said, but would you be on an immunosuppressant. I would rather not take that chance with you. Or, you know. I went with more people that got the shots to hold hands. I've given that up for those shots. And I'm a smartass by nature. And typically, when I'm given a shot, I typically say something about, there's gonna be a little prick. But don't worry, that's your nerves. And by the time they are processed, what I said, I'm the needles done. And, you know, it's like, and they didn't feel it. And, you know, it's like, my mom hated getting her blood drawn. And so that's why I learned those tricks of like, okay, I'm gonna give you a shot, I want you to yawn for me, or cough. And if you're doing that, you can't tense your muscles up. So, it doesn't hurt as bad. You know, I've had the privilege to learn from some of the best nurses in the world. Because when I went to school, part of your night care, as a night nurse, is you gave a backrub you massage them. They don't do that anymore. And I was teaching my nephew because his dad's a nurse, his mom's a doctor, his aunt is a nurse, you know, it's like, this is what you need to do. And I said, I said, you know, I'm always appreciative of the nursing assistants because I was a nursing assistant. But for me, give me a bath is a great time to one doing a full body assessment and to just talk and sometimes it's nonsense. I'm not a big sports guy. But I can talk sports if I needed to. I got a talent of being able to BS my way through, you know, conversations to make them think I know enough, just but, you know, it's like what kind of music? And you know, when I'm working with somebody that's planning their funeral? What kind of music do you want at your funeral? What? What do you see your funeral looking like, I have a playlist for my celebration of life. And one day, I got to pair it down because it's getting to be over 500 songs because I hear a song and and some of them are inappropriate, and you know, to say the least, but they have good memories for me. I remember playing Cheeseburger in Paradise, as we move to comfort care on this, this woman that that was her and her uncle song. And they would just bellow it out. So, everybody in the room was bellowing that song. The other ICU, we gotten complaints from the other nurses that we were making too much noise, but like, sorry, this is this is our sacred moment. And sometimes sacred is not quiet. And, you know, that's the other thing is that I always tell people, people die as they live. So, like, I've always lived in chaos, because I've had a big family.
Brian Ghafari-Naraghi 02:27:31
It, to this day, I have to have if I'm studying, I have to have the TV on and the radio on. So, I had that different noises. Because that's how I learned to study. So, you know, it's like, if, if you if you're allowed family, then talk, interact, tell stories. If you're a quiet family, that's okay. You quietly say prayer or read a book, or you do something. But like, I just put myself in, in the fog of if I'm in that bed, wondering if everybody's standing around me being quiet. I'd be thinking something bad's happening. Because my family's noisy. I like to do a couple of exercises, when I work with nurses, or healthcare professionals. And one of them is called my diner. So, you have an eight by ten Nursing homeroom. You have a three-bedroom house that you've lived in for 25 years. What are the twenty items thirty items that you're going to take them with you and put in your room? What what what what would be what's something that's important to you that you'd want to be you want to see pictures of family? An Afghan? You know, but I think that it helps to make make it real. And I always tell people, I'm gonna make you cry. And I'm sorry. And then I'm like, well, not really, because that's the whole purpose of this. And then I have a story. And so, I have them. I tell people to write out body parts, either motion by people, by things that are important to them. So then I start reading the story. And it's about a woman that's been diagnosed with cancer. And I'll say, cross out two items. And I'm like that, so when a patient that's what they're losing. So, you know, it's like, I had I, I had one woman walk out and she goes, I have my five children down. How do I pick which five? I'm like, sometimes we don't have that luxury of walking out. I said I said, but you know now that's not your calling in life and that's okay. But you know, it's I try to express being real. I want, because it's so important to be authentic. And to meet people where they come from, you know? Do I want an alcoholic to keep drinking? No. But they find comfort in it? Sure? What is it gonna do, kill 'em? You know, I've watched I've seen people take illegal drugs. And I'm like, Well, if you're going for the high, let me know, because I can get, I can increase your pharmaceutical grade, which is safer. But like, if you want to do a psychedelic, okay?
Brian Ghafari-Naraghi 02:31:50
I’m like, do you have somebody to be there to be safe? And I've been there, I've been the person to be the one we took it. But it gives them that sense of freedom, not being tied down to or defined as a diagnosis. And, you know, I find myself and I know, it's inappropriate. But if I hear a nurse, talk about a patient, you know, the guy, this are the heart attack that room six. I'll stop and say, the heart attack and room six has a name, what is his name? Because I don't want you to make it, if it's me in that bed, I don't want I don't want to be defined as my illness, or, you know, disability. And, you know, one of the things that we talked about I, people die of suicide. And I try to get people to understand they died of suicide, didn't die of bleeding out. They, you know, they didn't kill themselves, it was suicide. And to be in that dark and deep hole. I can't imagine that, that's your only option. You know, and so my heart breaks for those people. And I've told people, I'd rather spend all night talking with you, than having to attend your funeral. Call me, I'm there. I'll be there on the worst night. Because I don't want you to, I don't want you to feel like they're alone. Because nobody should be alone. And, you know, I have a lot of family that I've adopted along the way because they didn't have anybody. But that was kind of my mom, she, she fed everybody. We were poor, but there was always enough. And, you know, I get to live my life that way. And, you know, there are times I want to quit. I asked myself, Why did I become a nurse because of the politics or, you know, fighting with insurance companies. And then I think, Oh, I'm here. Back on my wall, here are some of my patients. There's pictures of my some of my patients with with me, or, like I had a picture. Some of the parents would send me a picture and a note about their child. And those to me are my prized possessions because it's priceless. And to be thought of, a mom made these Christmas ornaments one year with she took his shirts and made flowers and put them in ornaments, and I have one and it's so meaningful. I have a I have a bobber over over there for Enrique because I did, at camp we did a little memorial service and By using the example because Enrique loved the fish, about the bobber in life, we kind of just float down, sometimes we get pulled down, but we're all gonna be pulled back up, probably gonna pop back up and just kind of have faith that, you know, bad things happen. But that's part of life. And I would never trade, the bad things that occurred in my life because they made me who I am. They keep me humble, they keep me grounded. And what a great way to live life. You know, it's, it's an about who has the most junk at the end of it. But I do have a lot of junk. raising two kids, our parents dying 27 years together. You get a lot of junk. But I keep telling my son, you know, I'm not worried about it, it's gonna be your problem. But on a side note, my son nominated us for a show that they're going to be taping it over in Sweden, they have what they called Swedish death cleaning. So, you, you start cleaning your house to prepare for your death. I'm pretty sure as long as I pass the psychological evaluation, we're on the show. I've horrified that I'm going to be on the show. Danny's a, he is my extrovert. He's my flower. I'm like, oh, god, okay. But I said, there are rooms that they can't come into. Because these are my sacred spaces. Like, there's a line in my hallway, that nobody can go past that, because that that's my safe space. And, you know, that's, I think, part of my success of being able to do what I do, you know, because, you know, it's like, I write on a canvas, like, a patient's name that passes. So, I have years of starting back in 2010 of canvases that I've written their name on. Because, you know, I always say, you want to say their name, because that's the worst thing that can happen to somebody to be forgotten. And, you know, it's like, I, it's amazing how many people are afraid to talk to somebody, especially after they have a child that died. They don't want to say their name because they don't want to put them on. But then you lose, you know, part of that child dies as you don't acknowledge their existence. Or, you know, I, I try to correct parents when they say I have two children and, and one that passed. No, you have three children, two are living one is deceased, but you still have three children. Right? It doesn't change. Whether it's a day that you have with them, or lifetime. It's still important. My one last story when I was a night charge nurse in the large teaching hospital, I traumatize two units, all at the same time. So, we had a woman that was in a car wreck, she was 38 weeks pregnant. We knew the baby wasn't gonna make it. And there was question whether the mom was going to make it. So, I get my NICU nurses to bring the baby downstairs to the adult ICU. And we take pictures of mom holding the baby because I wanted that mom to have, she wouldn't remember it. But I, you know, and I hope they go What if she doesn't want them, then we throw them away. And that's something that you know, I can't recreate. So, my adult nurses were horrified by seeing the dead baby, and my pediatric nurses are horrified by seeing the sick adult. But, you know, it's like, but they still talk about it to this day. You know, it's like, what an amazing, I wouldn't have thought of that. It's like, you know, I tried to think of what I would want, you know, it's like, and I laugh because I never wanted children. And I have two, and I love them. But I never want them. Because you worry all the time. You know, it's like, now now, grandbabies. The worry, just continue is the new stages of worry. If I have a blessed life, I'm just so lucky. So that's kind of my story.
Kit Heintzman 02:42:01
I'm so curious. I think that the last two years for many has been an exposure to mass death that they haven't had before. Coming to it with your experience of so much death. Tell me something about what it felt like to be, to have deaths or around everyone for some of whom it felt kind of new.
Brian Ghafari-Naraghi 02:42:31
Well, I had that was a group of a population of people that I've never seen. But, you know, I never thought about as, as a death doula, you know, I’m thinking, I'm working with a family, somebody has a life limiting illness. But this got me thinking, I was talking to my friend who was a social worker, she moved to France, right before COVID started. And we started talking one day about you know, peoples need so we started posting on, on Facebook or on Instagram, if you need to talk. I'm here. And, you know, it's like, what do you charge? Nothing. Because, you know, it's like, it wouldn't be nice to make a living at it one day, but, there's no pair source for it. So, people wouldn't get it. So, it's how I give back to make my community better. You know its. Watching, I had a patient, that ALS patients that recently passed, and it was pretty sudden, and I got really close with him and his wife. He was a big governor of the university. So yeah, VIP. And my first introduction to him was he asked me, he told me I was gonna give him my cell phone. No, I don't know you, I don't give my cell phone out right away. And we kind of bonded over that. And when he died, his wife goes, Brian, I have this, these three wheelchairs that are in perfect shape. I said, Well, you could sell them. Or, if you want, you can donate them, and we can use them on patients that don't have the resources. And she did and the perfect patient got the perfect wheelchair. It was so amazing. Because this guy was six, five, and he's six, six. So those big wheelchairs are hard to find. And, you know, if I can make somebody's life a little easier, then I have you know, or laugh until they pee their pants. It's been a good day. I describe myself as I tell everyone, I’m a little bit crazy, you know, the best of us are you know, which helped me You know, one of the things that you learn early to have kind of a twisted sense of humor as an ICU nurse. And there's one, one shift, I come home and I won100 bucks. We had two patients actively dying. And we, we were betting on time. You know, and it was totally inappropriate. But it was the way we survived that shift. You know, do you know, I have, I have a collection of skeletons and coffins. And because after I got my masters people thought it was funny. And now I, I kind of like it. I have a large book, collection of death and dying grief and bereavement. And it's, it's a loaner library, I will loan out any other books or, you know, like, if I've worked with a family or friend or a patient, here, this might be helpful for you. And, you know, I had a patient or a husband, when I suggested that, he couldn't read. And I don't like the sound of my voice. You know, I just, but I have, I have a friend who has a beautiful voice. She could read the phone book, and it would sound good. So, she recorded it, she read the book, and we were able to give him the book where he could listen to it. And, you know, I love that aspect. Because I get to be creative. I get to MacGyver a lot of things. To make them work. I, I do have my stockpile of medical supplies that I that people give me and they're in my garage and drives my husband crazy. But, you know, somebody always needs them. And, you know, it's like, I have a wheelchair in my garage that just got returned, because my friend’s cousin had had surgery and needed a wheelchair for a month. And it was gonna cost him over $500 to rent it. And it's like, okay, it takes up a little space, I can hold on to it. And I joke about my nurses network of, if I don't have something, I have friends that I can call and say, Hey, do you know where I can find? Because, you know, some of the best nurses hold on to that stuff, because we know we're gonna need it.
Brian Ghafari-Naraghi 02:49:09
Yeah, I being able to support people during COVID has been a blessing. You know, I could easily become a hermit. Give me a book and a blanket and I can be lost for hours. But having to zoom or FaceTime with people to talk and sometimes it's just they just need to say it. You know, you have to name it. And once you name it, it's okay. You know, I've dealt with people who have never dealt with death in their life, and they were in their 40s. I was very thankful, you know, thinking back I'm thankful my mom took me to a funeral at five because I was exposed to it. It wasn't you know; it wasn't unusual for me. And, you know, being able to, to provide mementos or our keepsakes, so important. It cost nothing for me to do some of this stuff. And if it does cost me money, I come from the belief. You give what you have, and everything works out in the end. You cant take it with you. But I can actually say I love working in the death industry. I am mentoring a funeral director from Nairobi. She is interested in starting, like hospice in the life and the doula stuff. So, she reached out, kind of like you did on on my Doula page, and she goes, would you help teach me? Absolutely. She said, what do you charge? I said, if you can do something, give me something, you know, a decoration that is traditional for your country like, a little box or, you know, a little basket. Because those things, I have mean more to me than some of the things that we've spent tons of money on, because there's a story about them. And, you know, when I have bad days, I look at those things, and they get me through my days. Luckily, I don't have very many bad days, they do come, you know its. When my first friend, this was a nurse that died of COVID That was a kick in the stomach. And the sad part was, she was supposed to retire, retire, and then talked her into working one more month. And she died two weeks after she was supposed to retire. And, you know, I know she wouldn't be sorry for it. I felt horrible for her family. But you know, I always run towards danger. You know, they do active shooter training. And it's run, hide, fight. And I told them, and they're like, if somebody's shot, you step over. And I said, not going to happen. I said, its too ingrained in me to help somebody I, I beat the dumb person running after the shooter to tell you how they got me. At least I can mitigate multiple people because I'm just one person, you know, and I do what little I can. But you know, I cover this thing on Facebook that I saw one time that said, what if the person that had knows the cure for cancer isn't able to go to college? So as you know, I might be able to do this but somebody else might be able to do something that will change the world and I get to change the world a little bit at a time. You know. That's fine with me because that goes back to by working behind the scenes
Kit Heintzman 02:54:57
What are some of the ways that you've been taking care of yourself recently?
Brian Ghafari-Naraghi 02:55:02
Family time, massage, I paint. I started painting abstracts and part of it is I have chronic migraine. So I started painting what I see. But I also paint colors that I see around patients or feelings that I get from patients. I will kind of paint it out like it splattered across the canvas or you know I garden, but my friends and my family are my, my gift they're the one make it where I can do what I do.
Kit Heintzman 02:55:57
What's it been like negotiating your needs with your family, during COVID needs for safety you would mentioned being a homebody or husband more extroverted. How have you been navigating all of them?
Brian Ghafari-Naraghi 02:56:13
You know, you're just at the end of the day, it goes back to that you pull up your big girl panties and get over it, you know, life life goes on. Sometimes life sucks. And sometimes, you know, it's not what I would expect or hope for. A gift my mom always taught me is that there's always a silver lining. So I got closer with my husband during COVID You know, I got to share time with my my son and daughter in law, you know? So, you know, it's like I had time to do some genealogy research, or just stuff that I would consider wasting time in my normal everyday life I tend to just be lazy watch TV for one day I watch movies all day. So, I get it you know, I didn't have to feel guilty and you know, it's like I still mask when I'm out in public because I was working with ALS patients and I couldn't risk carrying something to one of them and because I wouldn't have been able to live with myself. Yes, it's uncomfortable. Yes, I don't like them. But a little bit of uncomfortable-ness to keep people safe. Not a bad thing. How about you what do you do to take care of yourself during COVID?
Kit Heintzman 02:58:08
I took up meditation.
Brian Ghafari-Naraghi 02:58:12
Well, I can only imagine this project is bringing up a lot of emotions.
Kit Heintzman 02:58:23
It does, um the primary one is actually gratitude. I am so grateful any anyone chooses to have this conversation with me.
Brian Ghafari-Naraghi 02:58:37
And know, you're always welcome to call me if you're having a bad day. I'm here I don't mind talking because that's how we're gonna get to get through this together that's the only way is we got to do it as a community and you know it's not ideal you know the world has changed and who knows if it'll go back to the same way, but I think it's a chance to learn and grow.
Kit Heintzman 02:59:27
How are you feeling about the immediate future?
Brian Ghafari-Naraghi 02:59:32
I'm positive I'm realistic I'm I'm afraid there's gonna be another surge, but I know we can handle it and you know it's all gonna work out me and one way or the other. And it might not be the way I want it to work out. But again, its not my play book.
Kit Heintzman 03:00:10
What are some of your hopes for a longer-term future?
Brian Ghafari-Naraghi 03:00:16
Oh, I love to see us, as a country, come together and help more people you know, or to learn from this, although, after watching Roe, Roe v. Wade, like okay, please don't repeat, we need to grow. But I am hopeful You know, one of the things that a lot of people talk about the millennials being entitled, but they're better at setting boundaries. You know, I was Gen X we suck it up and do it you know, keep on pushing through. And sometimes it's not bad to say, hey, I need a break. And, you know, it's I like to I do a lot of thinking and a lot of what ifs are kind of interesting and fun. But, you know, it's like, what if we don't do this? You know? I read I read the leaked Roe vs. Wade document. And they talked about domestic product, babies. And that's how they refer to them. And I'm like, okay, that's not okay. They're not a widget, but I think technology is making us lazier. And gentle, it's, I'm, I'm happy to be able to share as a they, they say old timers’ ways of doing things. Like, I don't need an IV pump to give medicine. I can count drips. I said, I can do so much without the monitor because I have those skills. And I'm grateful that I have those skills and being able to teach my nephew some of those tricks and tips. You know, because I really love old farm recipes or the old neighborhood mom. You know, like, for constipation I learned this years ago, you take two apples two oranges, a couple raisons. Put them in a blender with orange juice, till the top. You blend that down. You haven't drink three out of the first day and announced every day and they go regularly and there's no chemicals. I try not because I don't like medicines, you know because to get put on one medicine then you have to look for the side effect and. Thank you for letting me tell my story.
Kit Heintzman 03:04:04
Thank you so much for telling it.
Brian Ghafari-Naraghi 03:04:09
Hopefully it's something that was meaningful. You know, I think what I do is not special. Because because it's what what I'm supposed to do. You know? You know? I'm very humble about what, you know. I like my I get uncomfortable. I have a family that called me, Oh youre such an angel. No, I'm a nurse because it's like a whole different level of who I don't you know, it's like I was I do it was like you know, it's like it was just how I was raised, I had an amazing mom. I’m gonna, hold on just a second. Change my air buds, just a moment [inaudible]
Kit Heintzman 03:05:32
I can still hear you.
Brian Ghafari-Naraghi 03:05:39
[inaudible] what do you make of this?
Kit Heintzman 03:05:44
You dropped in and out there.
Brian Ghafari-Naraghi 03:05:44
Oh, I look forward to seeing what what I always thought to be interesting is to document nurses story. Know, in the twenty two years that I've been doing this just something just changed,[inaudible] I remember cus, they were being clinically trialed that were standard care. And, you know, it's like, I, when I was a volunteer, years ago, this nurse must have been nine, she worked her cap in our cape, she had a white starch uniform every day. And I think, well, I don't have to wear white, because I'm a dirt magnet., but it's like, just to see how far we've, we've come in critical thinking and, you know, anticipating being proactive, I think is amazing. So, I'm hopeful for the future. You know, what, that was one of the things that I enjoyed with Danny's getting a school superintendent, I get to meet some amazing kids turned into amazing adults. And, you know, that's what's going to change our world, is these bright, bright minds that would not traditionally have the chance.
Kit Heintzman 03:07:43
What would you want historians listening to this, to know about this moment that they might not know because they weren't here?
Brian Ghafari-Naraghi 03:07:51
We're resilient. No matter what, we're always gonna make it back. And the harder you, you make it, we're gonna push back harder. Because that's what we do. You know, I was raised, defeat is not have an option. Now your goals change, might change. But you're never beat, you never lose. Because you can always grow. And, you know, I think that we learned a lot about people during COVID, you know, some good, some bad. We've seen the good, the best and the worst of people. And, but we're still making it through, you know, we're still, We're surviving, and thriving, you know, in some ways, you know, because it's more than just surviving, we got to thrive. And we're growing and, you know, watching that vaccine be developed and knowing that it's been in development for three years prior to this is exciting. And, you know, to watch stuff that okay, we're gonna try this, you know, might not work. But, you know, one of the things that popped in my mind is I worked with muscular dystrophy and spinal muscular atrophy is a disease that was a terminal diagnosis. And actually, our my son's best friend in high school had it. Now they can do gene therapy, because they test at birth, and they can do this gene therapy. injection into their spine, and they can be normal kids. 20 years ago, that's unheard of. And I think we're just going to learn more and more. Yeah, it's, I just read about high schooler that develops sutures that change color when there's an infection. You know its like, what a simple idea. There's so much, University of Missouri where I was at just open this physician Research Building, called the next gem. So they have are bringing in the brightest for medical advancements and just watching it get built, my boss was the lead in that and, you know, him developing, getting in the right people in the right places. You know, it's like, like, I joke with him, I'm like, I did get to ride your coattails for a little bit. But you know, the thing that I think, like I keep coming back to is we're going to make it through will not be a little little worse for the wet. And, you know, I might need to learn to dress better again. I never used to wear sweatpants. So, I think that's pretty much what I wear but, yeah, you know, just looking over the last 100 years, the developments and how we've grown in, in our knowledge in our emotions. How we know how to we look, we're learning how to better to care for each other. And, you know, there's somethings that I don't understand. But I tried to learn, you know, it's like, sometimes I just don't know. But hey, it's always that's the thing about like, life is a learning opportunity always. And I think once you stop learning you die.
Kit Heintzman 03:12:43
I want to thank you so much. Those are all the questions I know how to ask right now.
Brian Ghafari-Naraghi 03:12:49
Ok.
Kit Heintzman 03:12:50
At this point, I just want to open some space. If there's anything you'd like to say that I haven't made room for. Please do so.
Brian Ghafari-Naraghi 03:12:57
Oh, I think youve just let me ramble on. But ya know, I had so much fun talking to you. And if you have more questions later on, hit me up. Or if you get overwhelmed. Hearing all the stories. And you need a safe place, I'm here.
Kit Heintzman 03:13:16
I really appreciate that. Thank you.
Brian Ghafari-Naraghi 03:13:19
No problem. Have a great night.
Kit Heintzman 03:13:21
You too.
This item was submitted on June 15, 2022 by [anonymous user] using the form “Upload” on the site “Oral Histories”: https://covid-19archive.org/s/oralhistory
Click here to view the collected data.